Abstract
Aims: The aim of this study was to analyse the feasibility, safety and effectiveness of tricuspid valve (TV) repair using the MitraClip system in patients at high surgical risk.
Methods and results: Forty-two elderly high-risk patients (76.8±7.3 years, EuroSCORE II 8.1±5.7) with isolated TR or combined TR and mitral regurgitation (MR) underwent edge-to-edge repair of the TV (n=11) or combined edge-to-edge repair of the TV and mitral valve (n=31). Procedural details, success rate, impact on TR severity and predictors of success at 30-day follow-up were analysed. Successful edge-to-edge repair of TR was achieved in 35/42 patients (83%, 68 clips in total, 94% in the anteroseptal commissure, 6% in the posteroseptal commissure). In five patients, grasping of the leaflets was impossible and two patients had no decrease in TR after clipping. In those with procedural success, clipping of the TV led to a reduction in effective regurgitant orifice area by -62.5% (from 0.8±0.4 to 0.3±0.2 cm2; p<0.0001). In both patients with isolated TV and combined procedures, six-minute walking distance improved (from 285±118 to 344±81 m and from 225±113 to 261±130 m, p=0.02 and 0.03, respectively). Predominant anteroseptal or central TR was identified as a predictor of procedural success (p=0.025).
Conclusions: Edge-to-edge repair of the TV is feasible with a promising reduction in TR, which could result in clinical improvement.
Abbreviations
EROA: effective regurgitant orifice area
ICD: implantable cardioverter defibrillator
MLHFQ: Minnesota Living with Heart Failure Questionnaire
MR: mitral regurgitation
NYHA: New York Heart Association
RV: right ventricle
SD: standard deviation
TR: tricuspid regurgitation
TV: tricuspid valve
Introduction
Moderate to severe tricuspid regurgitation (TR) is associated with significant morbidity and reduced long-term survival in several cohorts of patients1. This observation holds true irrespective of TR aetiology and left ventricular function2. Furthermore, relevant TR is a well-established predictor of inferior outcome following surgical or transcatheter treatment of mitral regurgitation3-5 and aortic stenosis6,7.
Given the high procedural mortality of surgical tricuspid valve (TV) repair or replacement and in particular when combined with MV repair, there is increasing interest in transcatheter therapies for these patients. Several transcatheter techniques and devices have demonstrated promising early feasibility results8,9. Amongst them, the edge-to-edge repair technique in the TV using the MitraClip™ (Abbott Vascular, Santa Clara, CA, USA) is, so far, the most commonly used technique. Small reports on isolated TV as well as combined mitral valve (MV) and TV procedures for valvular regurgitation have demonstrated a reduction in TR and consequently some clinical benefit10-12. Recently, Nickenig et al reported results from a multicentre experience including 64 patients13. In addition, a registry on percutaneous tricuspid valve intervention shed light on patients currently considered for these interventions14. Here we report a single-centre experience of 42 patients undergoing edge-to-edge repair for the treatment of TR with complete clinical and echocardiographic 30-day follow-up and, for the first time, provide predictors of procedural success.
Methods
PATIENTS
This retrospective analysis was conducted at the Heart Center, Leipzig University, Germany. Forty-two consecutive patients with New York Heart Association (NYHA) functional Class ≥II despite optimal medical therapy, relevant TR and at high surgical risk with or without concomitant relevant mitral regurgitation were considered. All patients were discussed within the Heart Team and considered to be at prohibitive risk for surgery. Therefore, an interventional approach for the treatment of TR using the MitraClip device on a compassionate use basis was suggested (Supplementary Appendix, Supplementary Table 1).
Preprocedural routine clinical assessment included transthoracic as well as transoesophageal echocardiography (Supplementary Appendix, Figure 1), a six-minute walk test, evaluation of NT-proBNP levels (Cobas, Elecsys NT-proBNP II; Roche Diagnostics, Rotkreuz, Switzerland) and a quality of life assessment using the Minnesota Living with Heart Failure Questionnaire (MLHFQ). Risk of malnutrition at baseline was evaluated by a nutritional risk screening (NRS) questionnaire. Edge-to-edge treatment of TR using transcatheter techniques was first performed in June 2016, and this report contains all consecutive patients who were treated until April 2017. The present analysis complies with the Declaration of Helsinki and was approved by the local ethics committee.
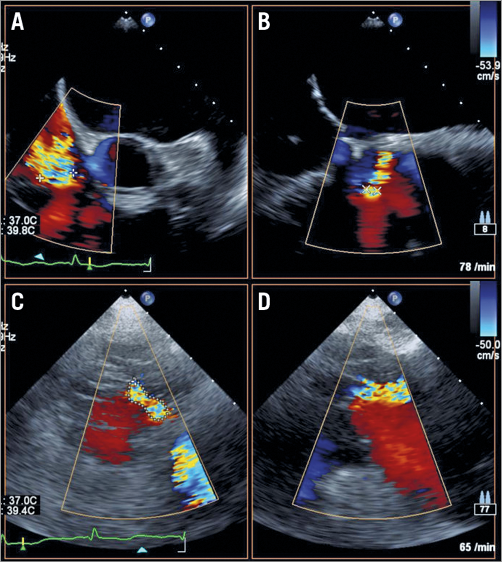
Figure 1. Echocardiographic assessment of vena contracta and planimetric EROA. Mid-oesophageal X-plane images in two orthogonal planes, 90° rotation (A), 0° rotation (B), for quantification of the minor and major vena contracta diameters. Planimetric assessment of the anatomic effective regurgitant orifice area on transoesophageal transgastric en face view, 30° rotation (C), of the tricuspid valve with the help of colour Doppler imaging and verification of true coaptation level on X-plane view (D).
TRANSCATHETER TRICUSPID REPAIR
Tricuspid repair was performed under general anaesthesia with interventional guidance by 2D and 3D transoesophageal echocardiography and fluoroscopy. In cases with simultaneous treatment of TR and mitral regurgitation, MV repair was carried out first and the MitraClip system was withdrawn into the right atrium afterwards. After 18 patients were treated, the steering technique for TV edge-to-edge repair was modified and the clip delivery system was inserted 90° counter-clockwise to improve alignment of the clip delivery system perpendicular to the targeted commissure, as described recently by Braun et al12. Transoesophageal multiplane 2D and 3D echocardiography was used to confirm correct clip orientation in relation to the TV. Transgastric imaging supported clip orientation and localisation in the designated commissure. Leaflet grasping was documented using mid- to deep-transoesophageal four-chamber views corresponding to long-axis and transgastric views. More than one clip was used if a satisfactory reduction of TR was not achieved after implantation of the first clip.
FOLLOW-UP EXAMINATIONS
All patients underwent repeat transthoracic and transoesophageal echocardiography before discharge (i.e., two to five days after TV repair and at 30-day follow-up). On each visit, symptoms were recorded, and a physical examination was performed. In addition, patients underwent routine blood sampling (including repeat measurements of NT-proBNP levels) and six-minute walk testing.
STATISTICAL ANALYSIS
Supplementary Appendix.
Results
BASELINE CHARACTERISTICS
Edge-to-edge repair of the TV for TR was attempted in 42 patients. A combined procedure of the MV and TV was performed in 31 patients, in 11 patients in the TV position only. Baseline characteristics are summarised in Table 1. Patients with isolated TV procedures had significantly lower levels of γ-glutamyl transferase, degree of severe mitral regurgitation (0% vs. 84%) and better LV function with borderline significance (LV ejection fraction <45%, 18 vs. 26%; p=0.054). Patients were at high risk for surgery (mean age 76.8±7.3 years, EuroSCORE II 8.1±5.7%) with no significant differences between the two groups. All patients reported dyspnoea, 29% exhibited ascites, 33% pleural effusion and 71% peripheral oedema. The mean score on NRS for all patients was 3.2±0.8.
PROCEDURAL RESULTS
The median procedure time was 102.5 min (range 18-207) with a median fluoroscopy time of 27.9 min (range 4.3-46.9 min). Successful clip placement in the TV position with a reduction in TR by at least one degree was achieved in 35/42 patients (see Supplementary Appendix for reasons for unsuccessful clip placement). The overall procedural success rate (successful clip placement leading to a reduction in TR of at least one grade) was 83%. In total, 68 clips were implanted in the TV position, 6% between the septal and posterior leaflets, 0% between the anterior and posterior leaflets (removed in two cases due to insufficient TR reduction), and 94% between the septal and anterior leaflets.
In total, there were four complications with details outlined in the Supplementary Appendix. In three patients with unsuccessful TR treatment, the iatrogenic atrial septal defect following MitraClip implantation in the mitral position was closed due to right-to-left shunting across the defect. There were no intraprocedural deaths or device migration.
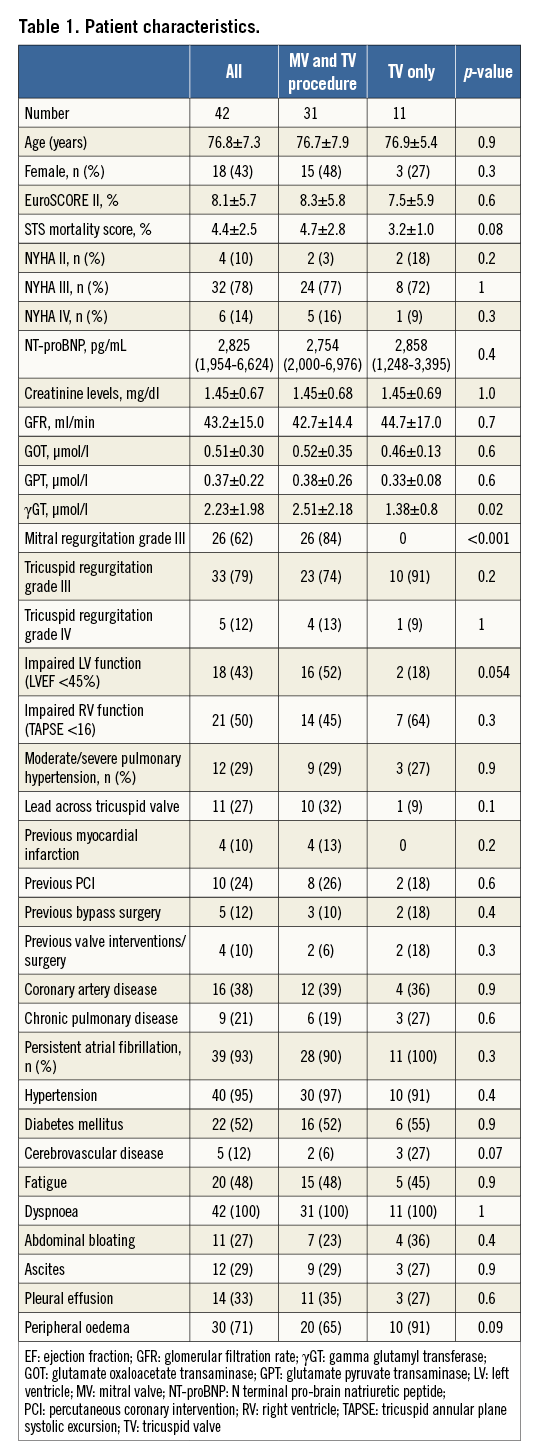
Acute echocardiographic evaluation in 37 patients with clip placement demonstrated a reduction in TR grade to I or II in 71%; the EROA was reduced from 0.79±0.4 to 0.33±0.2 cm2 (p<0.0001) (Figure 2).
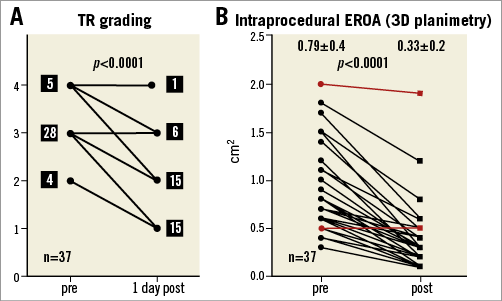
Figure 2. Intraprocedural assessment of tricuspid regurgitation. Intraprocedural tricuspid regurgitation grades (A) and anatomic effective regurgitant orifice area (planimetry) (B) before and immediately after transcatheter treatment of all 37 patients with clip placement in tricuspid valve position (red lines indicate the two patients with no tricuspid regurgitation reduction despite clip placement).
ECHOCARDIOGRAPHIC AND CLINICAL OUTCOME
Two patients died during the 30-day follow-up period (both in the combined group), leading to a 30-day mortality of 4.7% (in the combined cohort 6.45%). One patient with severe MR and TR died in hospital 29 days after combined edge-to-edge repair with implantation of two clips in the tricuspid and two clips in the mitral position. No relevant reduction of MR and TR was achieved due to massive annular dilatation and the patient died from progressive right heart failure. The other patient died at home 15 days after successful combined MV and TV repair. TR and MR were reduced from severe to mild; the cause of death in this patient is unclear. No autopsy was performed. Hence, mortality at 30 days was 2.8% and 12.8% in those with a successful and unsuccessful procedure, respectively.
Clinical and echocardiographic 30-day follow-up was complete for all patients alive with initial clip implantation in the TV position (35/37 patients). Results on follow-up echocardiography are summarised in Table 2.
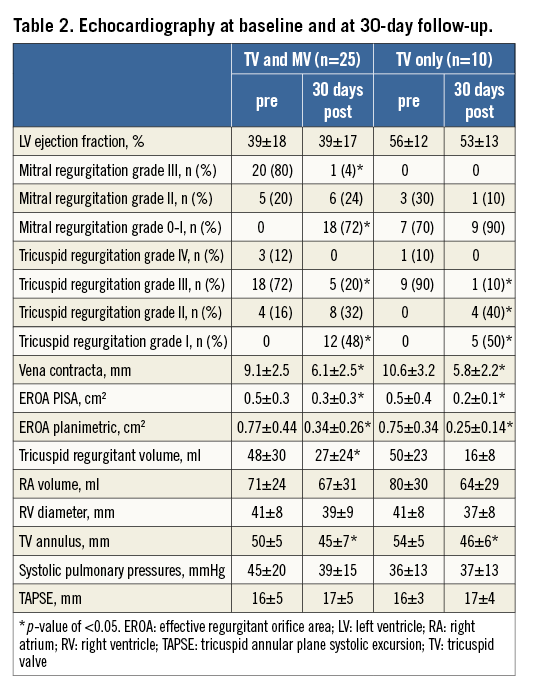
In both groups, significant improvements in NYHA functional class (Figure 3) and six-minute walking distance were observed during follow-up (Figure 4). Eight patients in both groups did not show any improvement in NYHA functional class during follow-up. Among these patients, TR grade remained stable despite tricuspid valve edge-to-edge repair in three patients. In one patient, TR grade was reduced from massive to severe (Supplementary Table 2). NT-proBNP levels decreased at 30-day follow-up in both groups numerically with statistical significance in the TV only group (Figure 4). No significant change in MLHFQ score was apparent after 30 days of follow-up both in patients with combined MV and TV repair (36.9±14.3 vs. 28.4±15.9, p=0.071) and in patients with isolated TV repair (27.4±10.4 vs. 31.6±18.2, p=0.351).
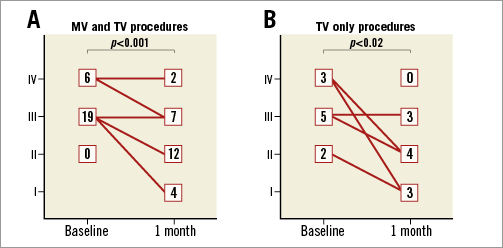
Figure 3. Change in NYHA functional class. Changes in NYHA functional class before and 30 days post procedure in patients with mitral and tricuspid procedures (A) and isolated tricuspid valve interventions (B).
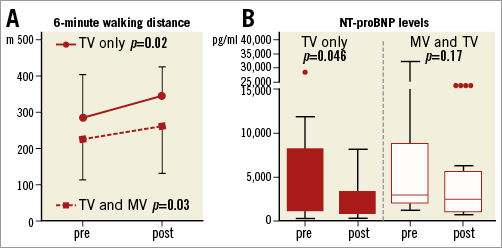
Figure 4. Change in six-minute walking distance and NT-proBNP. A) Changes in six-minute walking distance in combined mitral and tricuspid interventions (dotted line) and isolated tricuspid valve interventions (solid line). B) Box plots of changes in NT-proBNP in combined mitral and tricuspid interventions (unfilled boxes) and isolated tricuspid valve interventions (filled boxes).
In the 29 out of 35 patients completing one-month follow-up, three-month follow-up was also complete (Supplementary Appendix). The initial reductions in vena contracta (VC) and EROA were well maintained (Figure 5). The percentage of patients with peripheral oedema and ascites in both groups was significantly reduced after three months of follow-up (Supplementary Table 3).
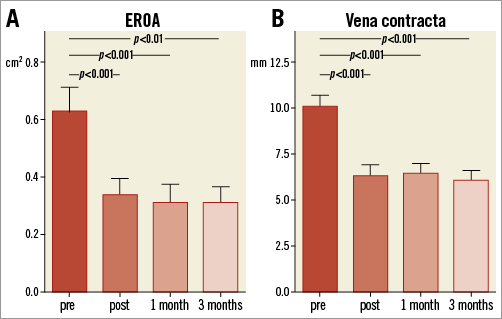
Figure 5. Change in EROA and vena contracta during follow-up.
Tricuspid effective regurgitant orifice area (A) and vena contracta (B) at baseline, pre-discharge, one- and three-month follow-up in 29 patients completing a three-month follow-up visit.
PREDICTORS FOR FAILURE OF TRICUSPID EDGE-TO-EDGE REPAIR
A predominantly non-central or non-anteroseptal TR jet appeared as the only significant predictor of procedural failure. Procedural failure was defined as less than at least one grade of TR reduction at one month or death during follow-up and was noted in 10 out of 42 patients (odds ratio 6.0, confidence interval 1.3 to 28.3; p=0.025) (Figure 6).
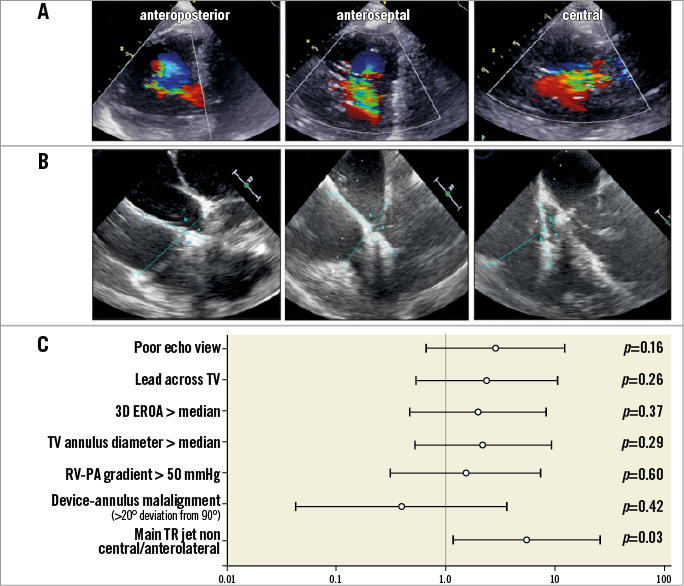
Figure 6. Analysis of predictors of procedural failure. A) Examples of patients with a tricuspid regurgitant jet located predominantly in an anteroposterior (left), anteroseptal (mid) and central (right) position. B) Examples of patients with a shallow angle between the delivery system and the tricuspid annulus (left), a near perpendicular orientation (middle) and a steeper angle (right). C) Odds ratios, lower and upper confidence intervals and corresponding p-values of potential predictors of procedural success.
Discussion
Our results are in line with a recent report on a multicentre experience including 64 patients undergoing TV repair using the clipping technique13 with baseline characteristics comparable to a multicentre registry of patients undergoing various different percutaneous TV interventions14. Of note, the increased surgical risk attributable to the present study cohort appears not to be completely reflected by risk scores such as the STS mortality score or EuroSCORE II, as these patients display additional factors pointing towards an increased vulnerability, such as limited exercise capacity, exhaustion and risk of malnutrition.
There are a number of important points which should be considered in the interpretation of our results. TR graded as severe remained in 16% of patients following edge-to-edge repair and EROA remained at 0.33±0.2 mm² after the procedure, suggesting that there is still room for improvement with respect to technical and procedural aspects during TV repair. Recent data indicate that after minimally invasive mitral and TV surgery TR is reduced to grade 2 or less in more than 95% of cases and, therefore, one should be cautious not to fuel unrealistic expectations when alternative transcatheter options for TR are discussed with referring physicians, patients and relatives19.
The present analysis of our single-centre experience represents the result of a multidisciplinary learning curve. Selection criteria for this intervention were not predefined but evolved during our experience. At present, patients with excessive TR and lack of any remaining leaflet coaptation appear less suitable candidates for this procedure. We also learned that steering of the device can be difficult in some cases, and adequate echocardiographic visualisation of the TV is key to procedural success and should be evaluated in depth before transcatheter edge-to-edge repair is considered.
In our cohort, the reduction in TR was not associated with an improvement in RV function, which is in line with previous reports on percutaneous TV interventions13. From surgical reports, there is some evidence suggesting that RV function rarely improves after treatment but can even worsen, especially in patients with severe TR prior to surgery20,21. Pathophysiologically, reduction in TR reduces preload at the expense of introducing additional afterload. In our experience, neither impaired RV function nor the presence of pulmonary hypertension predicted a lower clinical benefit after the intervention. Nevertheless, there is the potential of worse RV function with reduction in TR, which needs to be addressed in future larger trials.
In patients with combined MR and TR, we decided to perform a combined procedure rather than a staged procedure based on two considerations: i) avoiding an additional intervention in a rather frail patient population with potential risks, and ii) we and others demonstrated that MV edge-to-edge repair improves TR during follow-up in a minority of patients22-24. However, a combined approach could introduce significant confounding with regard to the assessment of functional implications. Data on NYHA functional class by Braun et al suggested that functional improvement at one month of follow-up was similar in patients who had received combined mitral and tricuspid treatment and patients who underwent isolated TV repair12. Functional improvement and NT-proBNP levels were even better in patients with isolated TV treatment, supporting the concept that treatment of TR using transcatheter edge-to-edge repair can confer a clinical benefit. Nevertheless, causes of TR probably differ between the combined and the isolated TV repair group. Considering the differences in left ventricular ejection fraction between both groups of patients in the present study, TR was probably a consequence of left heart failure in most patients with combined MV and TV repair. However, causes of TR in the isolated TV repair group are less clear.
Our study contains a first analysis on predictors of success of TV edge-to-edge repair. Given these data, the location of the TR jet was a main predictor of success, and patients with a posteroseptal or anteroposterior TR jet had less benefit than patients with an anteroseptal or central TR jet. This is supported by a recent experimental work by Vismara and co-workers applying the MitraClip edge-to-edge repair technique to an ex vivo pulsatile model of functional TR in explanted porcine hearts which indicated that medial grasping of the anterior and septal leaflets is superior to posterior and septal leaflet or anterior and posterior leaflet grasping25. Importantly, in our cohort, clip placement between the anterior and posterior leaflets resulted in unchanged or even increased TR in two patients with subsequent clip removal. Future studies are needed to address the question of morphological assessment for prediction of procedural success.
Limitations
The number of patients treated in this retrospective analysis is limited. No predefined inclusion criteria were applied, and the clinical characteristics and morphometric measures of the TV complex varied substantially. The present analysis used intermediate endpoints to assess the clinical benefit of TV edge-to-edge repair; hard clinical endpoints are still missing.
The interpretation of the functional implications of tricuspid valve edge-to-edge repair in patients with combined procedures could be confounded, with the contribution of the individual interventions being difficult to dissect. Finally, given the limited experience with transcatheter TV repair and the small number of patients treated by the edge-to-edge repair technique so far, the choice of parameters included in the present regression analyses had to be based on clinical intuition. This analysis should be considered as hypothesis-generating at present.
Conclusions
The results of the present retrospective analysis indicate that TV edge-to-edge repair using the MitraClip system in patients with symptomatic TR and at high surgical risk is feasible and safe with an overall success rate of 83%. Although TR is significantly reduced by TV edge-to-edge repair, residual TR remains in most patients, highlighting the need for further technical and procedural refinement. Nevertheless, TR reduction was maintained during three months of follow-up and translated into stable improvements in NYHA functional class and six-minute walking distance.
| Impact on daily practice The results of our study support the application of transcatheter TV edge-to-edge repair for amelioration of symptoms in selected patients. Anteroseptal TV pathologies appear to be more favourable subjects for TV edge-to-edge repair, which should be considered during patient screening and selection. |
Conflict of interest statement
P. Lurz, J. Seeburger, J. Ender and A. Linke have received speaker fees from Abbott. The other authors have no conflicts of interest to declare.
Supplementary data
Supplementary Appendix. Methods and results.
Supplementary Table 1. Excluded patients.
Supplementary Table 2. Clinically improved versus unimproved patients.
Supplementary Table 3. Change in clinical signs and liver enzymes.
To read the full content of this article, please download the PDF.