Introduction
Since the approval of the first transcatheter valves, there has been an exponential increase in interventional valve treatment. The enormous achievements in transcatheter techniques have raised hope that in the near future the therapeutic range can be expanded for tricuspid valve (TV) disease. The treatment of TV disease requires a comprehensive evaluation of the underlying causes.
In most cases, tricuspid regurgitation (TR) is caused not so much by intrinsic changes in the valvular apparatus but more because of the functional consequence of left-sided valvular heart disease and a pressure increase in the pulmonary circulation with subsequent right ventricular dilatation.
The prevalence of TR in patients with left-sided heart disease is about 50%. The prognostic impact of TR in such patients is directly related to its severity, with current guidelines proposing correction of TR at the time of left heart surgery.
Another group of patients present with late occurring TR after mitral valve surgery. This affects up to 37% of patients and is associated with worse clinical outcomes. Treatment options are limited, since operative mortality rates are described as being intolerably high (10-20%).
A third group includes patients with isolated “true TR”. In this group, reduction of TR seems directly related to relief of heart failure symptoms. However, in current guidelines there is a reluctance to advise isolated TR surgery for this group because the prognostic benefit of surgery is unclear and operative mortality is high. Treatment options for patients in groups two and three are limited and medical therapy alone does not prevent progression of global heart failure. Obviously, there is an “unmet need” for a safe, minimally invasive and effective way to treat patients with symptomatic TR at prohibitive surgical risk.
Minimally invasive catheter-based techniques might be an option for the treatment of TR in selected high-risk patients.
Interventional options
There are different approaches for the interventional therapy of TR. In the recent past we, and other groups, have demonstrated that treatment of TR with the Mitralign transcatheter annuloplasty system (Mitralign, Inc., Boston, MA, USA) might be a safe and effective treatment option. The procedure leads to a significant reduction of TR and reduction of heart failure symptoms in the treated patients.
Another promising option for the treatment of TR is to use the MitraClip® device (Abbott Vascular, Santa Clara, CA, USA). This might offer certain advantages compared to other interventional approaches to TR.
Interventional cardiologists are familiar with the MitraClip system and its use in atypical valve anatomies. The procedure can be performed without relevant modification of the device under echocardiographic guidance. The direct approach on the tricuspid valve leaflets enables treatment of degenerative valve disease or functional or mixed aetiology of TR.
Clinical experience
The first reported series of MitraClip procedures for the treatment of TR was published in early 2016. Three consecutive patients were treated for severe TR in advanced stages of right heart failure with functional NYHA Class III-IV and multi-organ damage. Echocardiography confirmed severe, isolated TR in all patients (effective regurgitant orifice area [EROA], patient 1: 0.7 cm², patient 2: 0.3 cm², patient 3: 1.5 cm²) with dilatation of the inferior caval vein (patient 1: 33 mm, patient 2: 22 mm, patient 3: 37 mm). The procedure was performed under general anaesthesia with interventional guidance from transoesophageal echocardiography (2D, 3D-TEE) and fluoroscopy (Figure 1, Moving image 1). Echocardiography showed acute reduction of TR in all patients (∆-EROA, 0.4±0.4 cm²), which was confirmed with TTE before discharge. Along with other TR-defining measures, IVC width (∆-IVC width, 3.5±2.1 mm) and TV annular diameters (∆-TV annular diameters, 14.3±8.9 mm) were reduced after the procedure (Figure 1, Moving image 2). No severe complications occurred during the procedures, mean procedural time was 133.7±42.2 min (87-169 min), without use of contrast dye. The patients were discharged after 5.5±2 days with improved clinical conditions.
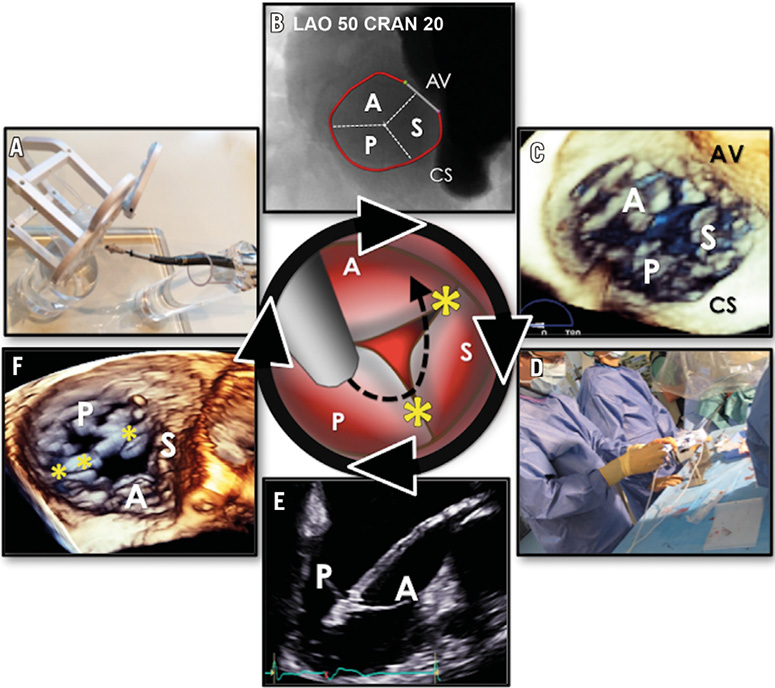
Figure 1. Interventional strategy and procedural set-up. Central image. Procedural strategy. A) Atypical approach simulation in a dedicated bench top model. B) CT reconstruction of the tricuspid annulus and anatomical landmarks (CS, AV) with 3mensio software. C) 3D-TEE showing an en face view of the tricuspid valve. D) Set-up in the cathlab. E) 2D-TEE visualisation of a leaflet grasp. F) 3D-TEE of final result after implantation of three clips. * clip device. A: anterior tricuspid valve leaflet; AV: aortic valve; CS: coronary sinus; P: posterior leaflet; S: septal leaflet
To date, over fifty tricuspid MitraClip procedures have been performed worldwide. Clinical and procedural information from these procedures is currently being collected and pooled in order to evaluate patient outcome, procedural safety and efficacy.
Despite promising initial results, it should be noted that the tricuspid apparatus has its own complexity, which must be taken into account when approaching severe or massive TR with large central coaptation defects. Therefore, refinements in procedural strategy will be necessary to expand the applicability of this technique.
With further development, interventional treatment of TR in inoperable patients might become clinical routine, under local anaesthesia, without thoracotomy and extracorporeal circulatory support.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
Moving image 1. 3D echocardiographic guidance of tricuspid clipping.
Moving image 2. 3D echocardiography: results after clip implantation in the anteroseptal commissure.
Supplementary data
To read the full content of this article, please download the PDF.
3D echocardiographic guidance of tricuspid clipping.
3D echocardiography: results after clip implantation in the anteroseptal commissure.

