Abstract
Aims: Tricuspid regurgitation (TR) severity and right ventricular (RV) dysfunction have been identified as significant predictors of outcome after mitral valve surgery. The aim of the present study was to investigate the impact of percutaneous mitral valve repair (PMVR) with the MitraClip system on functional TR severity and RV function.
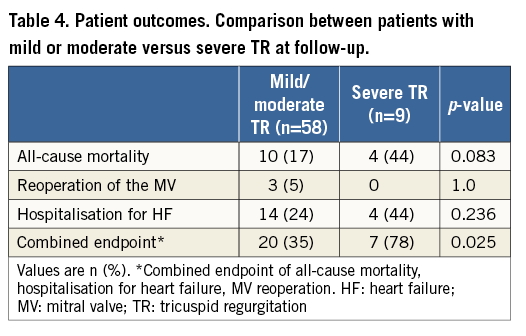
Methods and results: Among 119 consecutive patients with severe mitral regurgitation who underwent PMVR, 67 had complete baseline and follow-up transthoracic echocardiography after 3-12 months (6.8±2.9 months). TR severity was graded as mild, moderate, and severe. RV systolic function was assessed by fractional area change (FAC) and tricuspid annular plane systolic excursion (TAPSE). Clinical endpoints at follow-up included mortality, reoperation of the mitral valve, hospitalisation for congestive heart failure and New York Heart Association (NYHA) functional class. After PMVR, a significant decrease in TR severity (by at least one grade) was observed in 22 (33%) patients, while an increase occurred in only seven (10%) patients (p=0.02). Overall, systolic RV function (FAC and TAPSE), RV dimensions, and tricuspid annular diameter did not change significantly. Baseline SPAP was significantly higher (57±15 vs. 43±14 mmHg, p=0.002) and SPAP reduction significantly larger (-14±13 versus 1±15 mmHg, p=0.012) in patients who improved their TR. Multivariate logistic regression analysis identified the change in SPAP as the only significant predictor of changes in TR (odds ratio [OR] [for every change in SPAP by 10 mmHg] 1.90, 95% CI: 1.02±3.54; p=0.044). Patients with mild/moderate TR at follow-up after PMVR had lower event rates compared to those with severe TR (35% vs. 78%, respectively, p=0.025).
Conclusions: PMVR using the MitraClip device improves functional TR severity in approximately one third of patients, particularly in those who experience a significant SPAP reduction after the procedure.
Introduction
Severe mitral regurgitation (MR) is associated with progressive left ventricular dysfunction and congestive heart failure, leading to high rates of morbidity and mortality1. In Europe, MR is the second most frequent valve disease requiring surgery2. Recently, percutaneous mitral valve repair (PMVR) with the MitraClip® system (Abbott Vascular, Santa Clara, CA, USA) has emerged as a safe, less invasive, alternative therapeutic option to surgery, in patients with moderate to severe MR and high surgical risk. Based on the favourable results of several multicentric investigator-driven registries3-6 and the results of one randomised trial7, the technique has gained wide acceptance with more than 16,000 patients treated so far. On 24 October 2013 the MitraClip received FDA approval for use in patients with degenerative MR and at prohibitive surgical risk8.
Functional tricuspid regurgitation (TR), which occurs on structurally normal tricuspid valves, is frequently observed in patients with MR9. Paradoxically, TR tends to worsen after mitral valve surgery10 (particularly in patients with ischaemic or dilative cardiomyopathy), with close to 50% of patients having postoperative TR despite successful surgery with lowering of pulmonary pressure9. The severity of TR may increase even further in the years following surgery, and is associated with worse outcomes11. Some have proposed impaired right ventricular function6 and/or geometrical distortion of the tricuspid annulus after MV surgery as the underlying mechanism for postoperative TR9,12. PMVR with the MitraClip has only a slight impact on mitral annular geometry and has been shown to induce reverse left ventricular (LV) remodelling13, but its effect on RV dimensions and function, tricuspid annular geometry and TR has not been extensively investigated as yet14.
The purpose of this study was therefore to explore changes in TR severity and RV function after PMVR, and to relate these findings to acute and long-term procedural success and patient outcome.
Methods
PATIENT POPULATION AND STUDY DESIGN
We included consecutive patients who underwent PMVR using the MitraClip system at the University Hospital Zurich and had baseline and follow-up transthoracic echocardiography (TTE) available. Exclusion criteria included a recent myocardial infarction or revascularisation, any cardiac surgery, repeat PMVR, or cardiac resynchronisation therapy (CRT) device implantation <6 weeks prior to the index PMVR or during follow-up, or degenerative TR aetiology. Indications for PMVR included symptomatic moderate to severe (3+) or severe (4+) MR15, with a high risk for surgery. An interdisciplinary Heart Team, which included an interventional cardiologist, a cardiac surgeon, an echocardiographer, and a cardiac anaesthetist, discussed each subject’s eligibility for PMVR. All patients gave written informed consent to be included in a prospective MitraClip registry (KEK-ZH-Nr. 2010-0466). The protocol of the registry was approved by the cantonal ethical committee of Zurich.
PERCUTANEOUS MITRAL VALVE REPAIR (PMVR) PROCEDURE
PMVR with the MitraClip device was performed according to standard technique described elsewhere16 with echocardiographic (three-dimensional transoesophageal echocardiography) and fluoroscopic guidance, and under general anaesthesia. Acute procedural success (APS) was defined as successful MitraClip implantation with immediate MR reduction to grade 2+ or less by echocardiography.
ECHOCARDIOGRAPHY
Transthoracic echocardiography was performed at baseline (shortly prior to the PMVR procedure) and at follow-up three to 12 months after PMVR. All echocardiographic films were stored in our clinical image database and independently reviewed by an experienced reader, blinded to the clinical history of the patient. A second reader re-evaluated TR severity (baseline and follow-up) to assess inter-observer variability. TR quantification, as well as evaluation of RV dimensions and function, were performed according to the recommendations of the American Society of Echocardiography (ASE), the European Association of Echocardiography and the Canadian Society of Echocardiography15,17.
In brief, TR severity was graded as mild, moderate or severe based on integration of various Doppler parameters (central jet area, density and contour, vena contracta width and hepatic vein flow) and the dimensions of the right-sided chambers. End-systolic and end-diastolic RV dimensions were measured by planimetry from the RV-focused apical 4-chamber (4CH) view17. RV function was assessed through fractional area change (FAC) defined as ([4CH end-diastolic area–4CH end-systolic area]/4CH end-diastolic area×100) as well as the tricuspid annular plane systolic excursion (TAPSE) acquired on M-mode tracings through the tricuspid annulus17. MR severity was graded from 1+ to 4+ according to ASE recommendations15. Systolic pulmonary artery pressure (SPAP) was calculated from peak tricuspid regurgitant jet velocity using the simplified Bernoulli’s equation and adding an estimate of right atrial pressure estimated from the inferior vena cava diameter17.
CLINICAL FOLLOW-UP
Clinical outcome was obtained from hospital records or by direct interrogation of the patient or his/her general practitioner. Clinical endpoints included death, recurrent hospitalisation for congestive heart failure (CHF), mitral valve surgery, and New York Heart Association (NYHA) functional class. CHF was defined by the classic Framingham criteria, with two major or one major and two minor criteria required to diagnose CHF18.
STATISTICAL ANALYSIS
Statistical analysis was performed with SPSS, Version 20 (IBM Corp., Armonk, NY, USA). Quantitative data are expressed as mean±SD or median with interquartile range (IQR) where appropriate and were compared using the Student’s t-test or the Mann-Whitney U test, respectively. Categorical data are given in proportions and percentages and compared by the chi-square test or McNemar’s test. Inter-observer variability of TR severity was measured using Cohen’s kappa coefficient. Numerical data were correlated using Spearman’s method. Multivariate logistic regression analysis was used to correlate clinical and echocardiographic variables with changes in TR using a dichotomised population: better versus same/worse. The results of logistic regression are given as odds ratios (OR) with their respective 95% confidence intervals (CI). Survival curves were generated using the Kaplan-Meier method. Log-rank tests were used to evaluate differences between groups. The reproducibility coefficient was calculated as 1.96 times the SD of the differences, as proposed by Bland and Altman19. All p-values reported are two-sided and a value of p<0.05 was considered statistically significant for all tests.
Results
PATIENT POPULATION
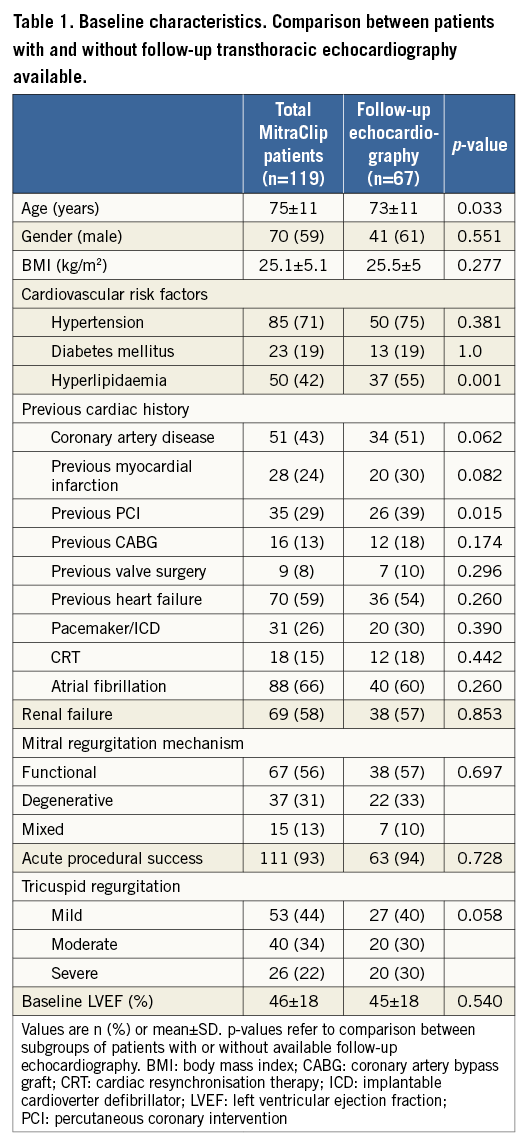
We included 119 consecutive patients who underwent PMVR using the MitraClip system (age 75±11, 59% males). MR was functional in 56%, degenerative in 31% and mixed in 13% (Table 1). Acute procedural success of PMVR was achieved in 111 (93%) patients. Baseline TR was mild in 53 (44%), moderate in 40 (34%), and severe in 26 (22%) patients. Left ventricular (LV) ejection fraction (EF) was <35% in 48 (40%) patients, 35 to 50% in 18 (15%) patients, and >50% in 53 (45%) patients.
Baseline and follow-up echocardiography was available in 67 of these 119 patients. There were no statistically significant differences between the two groups regarding baseline characteristics except for age, prevalence of hyperlipidaemia and previous percutaneous coronary intervention (PCI) (Table 1).
IMPACT OF PMVR ON ECHOCARDIOGRAPHIC PARAMETERS
Follow-up echocardiography was obtained at 6.8±2.9 months after PMVR. MR was grade 3 and 4 at baseline in 17 (22%) and 46 (78%) patients, respectively. At follow-up, five (8%) and seven (10%) patients remained in grade 3 or 4 MR, respectively (Table 2).
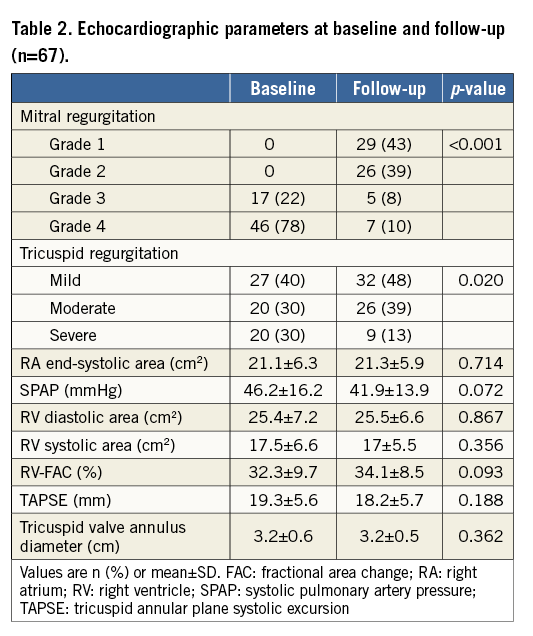
A significant decrease in TR severity (by at least one grade) was observed in 22 (33%) patients, while an increase occurred only in seven (10%) patients (p=0.02) (Figure 1). TR was mild, moderate or severe in 27 (40%), 20 (30%), and 20 (30%) patients at baseline, and in 32 (48%), 26 (39%), and 9 (13%) patients at follow-up, respectively (Figure 2). Inter-observer agreement for TR severity was good (Cohen’s kappa=0.56, p=0.002).
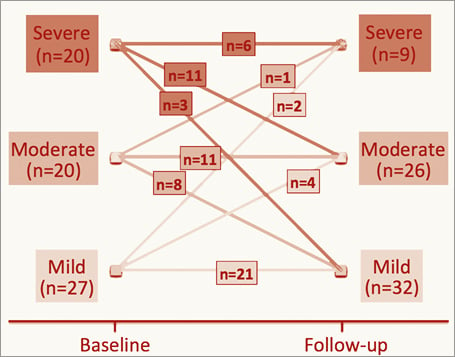
Figure 1. Evolution of tricuspid regurgitation severity at baseline and follow-up after MitraClip.
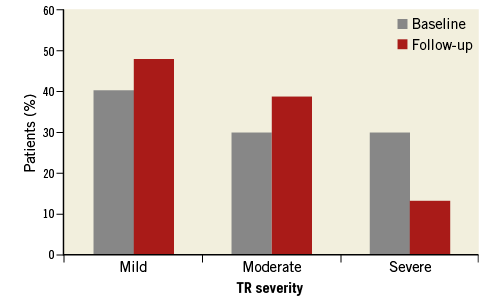
Figure 2. Tricuspid regurgitation severity at baseline and follow-up after MitraClip.
Systolic RV function (FAC and TAPSE), RV dimensions, and tricuspid annular diameter did not change significantly (Table 2). There was a trend towards a decrease in systolic pulmonary artery pressure (SPAP; 46.2±16.2 mmHg versus 41.9±14.0 mmHg, p=0.072).
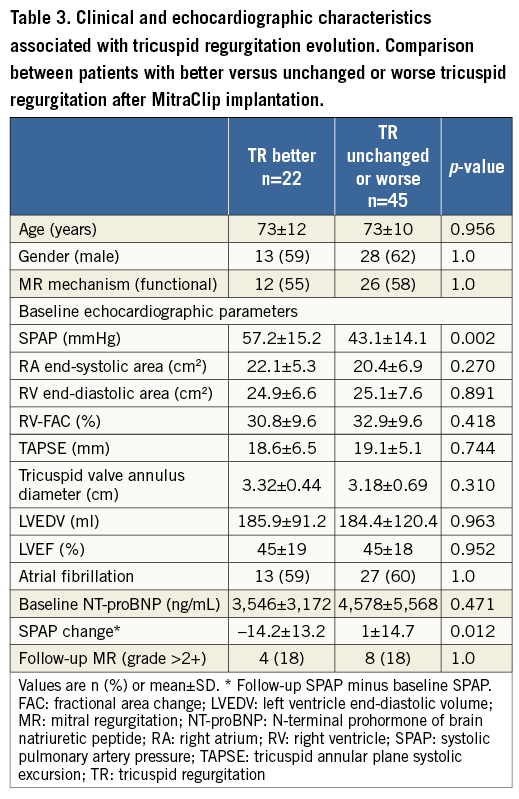
FACTORS ASSOCIATED WITH TR IMPROVEMENT
After PMVR, TR improved in 22 (33%) patients, and was unchanged or worse in 45 (77%) patients. Table 3 shows clinical and echocardiographic characteristics associated with TR evolution. Baseline SPAP was significantly higher (57±15 vs. 43±14 mmHg, p=0.002) and SPAP reduction significantly larger (-14±13 versus 1±15 mmHg, p=0.012) in patients who improved their TR. In fact, the magnitude of SPAP and TR change was directly correlated (r=0.41, p=0.006). There was no significant difference in any of the remaining parameters. Most importantly, neither LV nor RV parameters of dimension and function appeared to predict changes in TR. Multivariate logistic regression analysis identified the change in SPAP as the only significant predictor for changes in TR (OR [for every change in SPAP by 10 mmHg] 1.90, 95% CI: 1.02±3.54; p=0. 044).
CLINICAL FOLLOW-UP
PMVR improved NYHA functional class (Figure 3): NYHA Class III or IV was present in 76% of patients at baseline, which decreased to 23% at follow-up (p<0.001). As a consequence, the proportion of patients in NYHA I or II increased from 24% to 77%. N-terminal pro-brain natriuretic peptide (NT-proBNP) decreased from 4,246±671 to 3,642±526 ng/L, but the difference fell short of statistical significance.
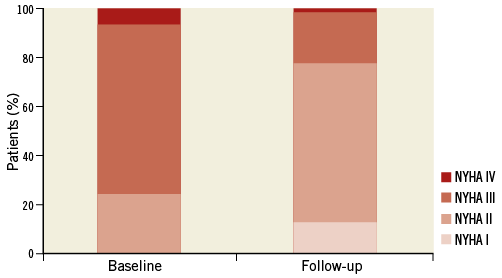
Figure 3. New York Heart Association (NYHA) functional class at baseline and follow-up after MitraClip.
Clinical events were recorded up to a median of 16 months (IQR 8-27 months). Patients with mild/moderate TR at follow-up after PMVR had lower event rates (death, rehospitalisation for heart failure, reoperation) compared to patients with severe TR (35% vs. 78%, respectively, p=0.025) (Figure 4, Table 4). On univariate Cox regression analysis, follow-up TR emerged as a significant predictor of outcome, but fell short of significance after adjusting for age, EF, SPAP, residual MR, NT-proBNP, and NYHA class.
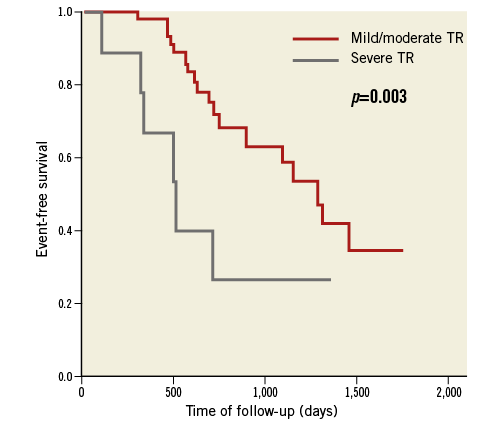
Figure 4. Kaplan-Meier survival free of the composite endpoint (death, rehospitalisation for heart failure, reoperation) for patients with mild/moderate TR versus severe TR at follow-up.
Discussion
The present study explored the impact of PMVR with the MitraClip system on functional TR severity. In our population of patients with predominantly functional MR and reduced systolic LV function, PMVR did not increase TR severity in the majority of patients at six-month follow-up. In fact, a significant TR reduction (by at least one grade) was observed in approximately one third of patients, while an increase occurred only in seven (10%) patients. However, systolic RV function (FAC and TAPSE), RV dimensions, and tricuspid annular diameter did not change significantly. Notably, of 20 patients with severe baseline TR, 14 patients improved to moderate or mild after PMVR, and only six remained in severe TR. Moreover, of the 20 patients who had moderate baseline TR, only one progressed to severe TR after PMVR. Overall, the majority of patients (87%) had only mild or moderate TR at follow-up after PMVR.
Surgical reports investigating the natural history of functional TR after mitral valve surgery have yielded conflicting results. For many years, the concept that functional TR decreases after successful mitral valve surgery was largely accepted by surgeons. Recent reports have challenged this concept, raising awareness about the potential undertreatment of functional TR9,10,20. Particularly in patients with functional MR aetiology (and underlying ischaemic or dilative cardiomyopathy), TR worsens early after surgery despite successful correction of left-sided valvular lesions, and may further deteriorate at longer-term follow-up10. Furthermore, TR progression is associated with a poorer prognosis in terms of morbidity and mortality21. Several mechanisms have been considered responsible for persistence or progression of TR after MV surgery. These include tricuspid annular dilatation, as well as RV remodelling and dilatation with increased leaflet tethering. The most important risk factors for TR progression after MV surgery are age, female gender, larger left atrial size, RV dilatation, higher pulmonary pressure, a history of rheumatic or ischaemic heart disease, and prosthetic valve dysfunction8. Thus, surgeons are now more in favour of correcting significant functional TR by reconstruction to prevent late deterioration, particularly if annular or RV dilatation is present at baseline22.
In contrast, in our patients none of the aforementioned risk factors was predictive of TR progression, except for SPAP. In fact, a high baseline SPAP, with a large reduction after PMVR was the only significant predictor of TR improvement. Neither RV nor LV dimensions nor function were predictive of any changes in TR. Thus, it appears that after PMVR the haemodynamic profile (i.e., pulmonary pressures) is the only variable that determines TR evolution8. We can only speculate on the possible explanations for this finding. On the one hand, PMVR avoids cardiopulmonary bypass and cardiotomy, which may lead to myocardial ischaemia, ventricular dysfunction and geometrical changes of annular planes. On the other hand, PMVR with the MitraClip system has been shown to spare LV contractility23 and to induce reverse LV remodelling (which may favourably affect the RV)24. Furthermore, the MitraClip has only a slight impact on mitral annular geometry22, while a rigid MV prosthesis (particularly when associated with chordal ablation) or annuloplasty device causes more annular distortion which could possibly exert disruptive forces on the neighbouring tricuspid annulus. Interestingly, further left atrial unloading into the right atrium through the iatrogenic atrial septal defect induced by the 22 Fr steerable guide catheter25 may contribute to TR worsening in the long term after PMVR. However, since tricuspid regurgitation tended to improve in our study population, we believe that the effect from atrial septal defect is rather marginal compared to the effect of SPAP reduction. Moreover, patients with mild/moderate TR at follow-up after PMVR had lower event rates (death, rehospitalisation for heart failure, reoperation) compared to patients with severe TR, which is consistent with previous surgical reports21 and first preliminary data from PMVR patients14.
Our findings have potentially relevant clinical implications for the treatment of double valve regurgitation. Functional TR improves in one third of patients after PMVR. This improvement can be predicted by higher baseline SPAP values and a significantly large reduction of SPAP after PMVR. Thus, a patient with severe baseline TR accompanying MR is likely to improve his TR after PMVR, particularly if baseline SPAP is elevated and a significant reduction in SPAP can be expected from successful MitraClip implantation. On the other hand, if TR is moderate at baseline, worsening remains unlikely regardless of age, gender, tricuspid annular enlargement, or RV dilatation or dysfunction. A transcatheter TR solution would allow the treatment of TR alongside MR in MitraClip candidates and may thereby provide better long-term outcomes.
Study limitations
We acknowledge a limited sample size. This is related to the fact that PMVR is a relatively novel intervention, and echocardiographic follow-up was not available in all of our patients. Nonetheless, the size of the cohort is comparable to previous surgical reports9,10. The limited sample size also prevented exploration of the differences between degenerative and functional MR patients or to perform multivariate Cox regression analysis. Moreover, grading of TR using TTE is only semi-quantitative, and using an integrative approach, as suggested by ASE recommendations15, may increase the accuracy in this regard. Nonetheless, TR quantification is subject to significant inter-observer variability. Moreover, cardiac magnetic resonance, not echocardiography, is considered the gold standard for evaluation of right ventricular function. Furthermore, the follow-up period was short. Previous surgical reports have followed patients for several years after the procedure, and have also reported late deterioration of TR9. We cannot exclude late TR impairment in our study population based on the present findings. It may well be that different mechanisms play a role in early versus late TR impairment. Potentially, haemodynamic changes (i.e., pulmonary pressures) play a more important role in the immediate postoperative period, while delayed RV and annular remodelling processes affect long-term TR evolution. The latter may also become relevant in our patients. However, PMVR patients tend to be significantly older and have shorter life expectancy than patients treated by surgery5. Hence, it seems justified to evaluate short-term follow-up periods.
Conclusions
PMVR using the MitraClip device improves functional TR severity in approximately one third of patients, particularly in those who experience a significant SPAP reduction after the procedure.
| Impact on daily practice Functional TR improves in one third of patients after PMVR. This improvement can be predicted by higher baseline SPAP values and a significantly large reduction of SPAP after PMVR. On the other hand, if TR is moderate at baseline, worsening remains unlikely regardless of age, gender, tricuspid annular enlargement, or RV dilatation or dysfunction. In the future, a transcatheter TR solution will possibly allow the treatment of TR alongside MR (or staged after PMVR) and may thereby provide better long-term outcomes. |
Funding
Outside of this study, T.F. Lüscher has received educational and research grants from Abbott to the institution.
Conflict of interest statement
The authors have no conflicts of interest to declare.