Abstract
Aims: We sought to assess the impact of tricuspid regurgitation (TR) severity on patient outcome in a collective with relevant mitral regurgitation undergoing MitraClip implantation.
Methods and results: From August 2010 to July 2013, 766 patients (age 75.3±8.5 years, 61% male, median EuroSCORE 24.3%±18.4) were prospectively enrolled in the TRAMI registry and stratified by echocardiography into no/mild, moderate and severe TR. Overall, the mean number of implanted MitraClips was higher in patients with severe TR but increasing TR severity was not associated with procedural success. In-hospital and one-year mortality as well as MACE and MACCE (death, myocardial infarction±stroke) rates were higher with increasing TR severity. Kaplan-Meier curves indicated a significant difference for mortality (p<0.0001), but not for rehospitalisation for heart failure. After multivariate Cox regression, severe TR proved to be a predictor for one-year mortality (HR 2.01, 95% CI: 1.25-3.26, p=0.004). Higher rates of severe bleeding were more frequent with increasing TR grades.
Conclusions: In patients with MitraClip implantation, increasing TR severity is associated with adverse outcome, higher bleeding rates and decreased survival rates.
Abbreviations
COPD: chronic obstructive pulmonary disease
EQ-5D score: EuroQol five dimensions questionnaire
LVEF: left ventricular ejection fraction
MACCE: major adverse cardiac and cerebrovascular events
MACE: major adverse cardiac events
MR: mitral regurgitation
NT-proBNP: N-terminal pro-brain natriuretic peptide
PAP sys: systolic pulmonary artery pressure
6MWD: 6-minute walking distance
TAVI: transcatheter aortic valve implantation
TR: tricuspid regurgitation
TRAMI: TRAnscatheter Mitral valve Interventions registry
Introduction
High-risk patients suffering from severe mitral regurgitation (MR) not referable to open heart surgery can be treated by MitraClip® (MC) implantation (Abbott Vascular, Santa Clara, CA, USA).
Tricuspid regurgitation (TR) is frequently found in this patient cohort as left-sided heart disease represents the most frequent cause of functional TR1. In patients suffering from severe MR, relevant concomitant TR is found in about 30-50%2. Both increasing MR severity and TR severity are associated with reduced survival rates3. Yet, the impact of TR on long-term outcome seems to be independent of age, biventricular function or pulmonary artery pressure4. Nowadays, concomitant relevant TR repair is suggested at the time of mitral valve surgery5.
The worsening impact of concomitant TR in patients undergoing MC implantation has been raised in a recent publication by Puls et al6, but details have never been evaluated.
Analysing patients included in the German TRAnscatheter Mitral valve Interventions (TRAMI) registry, we sought to assess the impact of TR severity on affected patients regarding 30-day and one-year outcomes.
Methods
TRAnscatheter Mitral valve Interventions (TRAMI) REGISTRY
From August 2010 to July 2013, prospective patient enrolment was made available to all sites in Germany performing catheter-based techniques. Further details about the registry and the follow-up have already been presented at length6.
PARTICIPANTS
The present analysis includes 766 patients exclusively treated by MitraClip implantation, prospectively enrolled.
Transthoracic echocardiographic parameters were evaluated according to the institutional practice of the treatment centre. Mitral regurgitation severity as well as TR severity were scaled in three grades as I (mild), II (moderate), and III (severe)7.
Procedural failure was recorded if one of the following criteria was reached: severe residual MR (grade III), conversion to open heart surgery, abortion of procedure or failure as assessed by the interventionist.
STATISTICS
Statistical analyses were performed at the Institut für Herzinfarktforschung, Ludwigshafen, Germany. Categorical variables were presented as absolute numbers and percentages and compared by χ2 or Fisher’s exact test. Continuous variables were expressed as mean with standard deviation or median with interquartile range and compared using the Mann-Whitney-Wilcoxon test. The cumulative 30-day and one-year mortality rates as well as freedom from rehospitalisation for heart failure were estimated by Kaplan-Meier analysis.
The impact of TR on one-year mortality was analysed by Cox regression. In addition to age, female gender and TR severity, the following variables were considered for inclusion: NYHA Class IV, sinus rhythm, anaemia, ≥2 clips implanted, previous aortic intervention, creatinine ≥1.5 mg/dl, peripheral artery disease, chronic obstructive pulmonary disease (COPD), decompensated heart failure, past medical history of cardiac decompensation, left ventricular ejection fraction (LVEF) <30%, systolic pulmonary artery pressure (/mmHg), history of stroke, MR aetiology and procedural failure as defined above. The model was finalised with a forward selection using an entry level of p<0.05. All tests were two-tailed and p-values <0.05 were considered significant. SAS statistical package version 9.3 (SAS Institute Inc., Cary, NC, USA) was used for the computations.
Results
BASELINE PATIENT CHARACTERISTICS
Among 766 MitraClip patients (mean age 75.3±8.5 years, 61% male), there were 334 patients suffering from no/mild (43.6%), 326 from moderate (42.6%) and 106 patients from severe (13.8%) TR (Table 1). The median follow-up time was 385 days (interquartile range [IQR] 371-429). Baseline data indicated significant differences concerning recent cardiac decompensation (p<0.05), malignancy (p<0.05), anaemia (p<0.001) and creatinine (p<0.05). Pulmonary hypertension was most frequently found in patients with severe TR (no/mild TR 41.5%, moderate TR 52.1%, severe TR 58.5%, p<0.01). Yet, elevated systolic pulmonary artery pressure (PAP sys) was found in all subgroups (no/mild TR 41 mmHg [IQR 33-52], moderate TR 45 mmHg [IQR 36-56], severe TR 50 mmHg [IQR 35-60], p<0.01). A trend test (Jonckheere-Terpstra) for the statistical dependence of TR grade and PAP sys proved significant (p=0.0003).
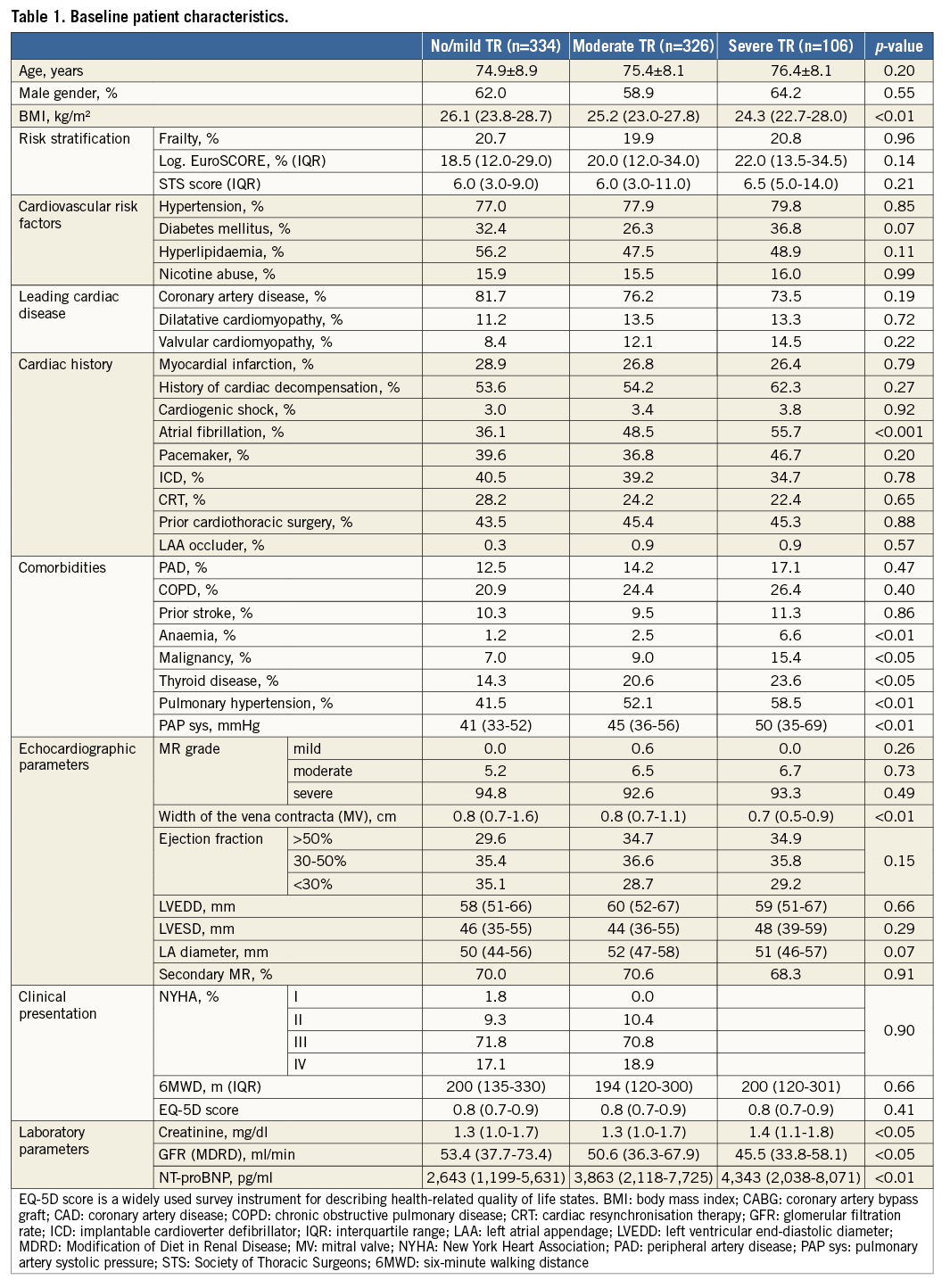
Coronary artery disease was the leading cardiac disease (about 75% in all subgroups, p=0.19). LVEF <30% was frequent (about 34%) and equally distributed (p=0.15). Previous cardiac interventions were comparable among the subgroups, except for previous transcatheter aortic valve implantation (TAVI) (TR in patients with previous TAVI: no/mild TR 10.3%, moderate TR 36.0%, severe TR 50.0%, p<0.05). For implanted cardiac pacing devices, there were no significant differences among the subgroups (p=0.20). Atrial fibrillation increased with TR severity (no/mild TR 36.1%, moderate TR 48.5%, severe TR 55.7%, p<0.001).
PROCEDURAL OUTCOME AND 30-DAY FOLLOW-UP
Procedural success was achieved in the majority of patients (no/mild TR 84.7%, moderate TR 85.8%, severe TR 77.4%, p=0.11), without significant differences regarding procedure (p=0.65) and radiation time (p=0.51) (Table 2). The highest mean number of implanted clips was found for severe TR (p<0.05). Intraprocedural complications were rare overall (n=5/766); however, the intra-hospital mortality and MACE rates were highest for severe TR (p<0.05).
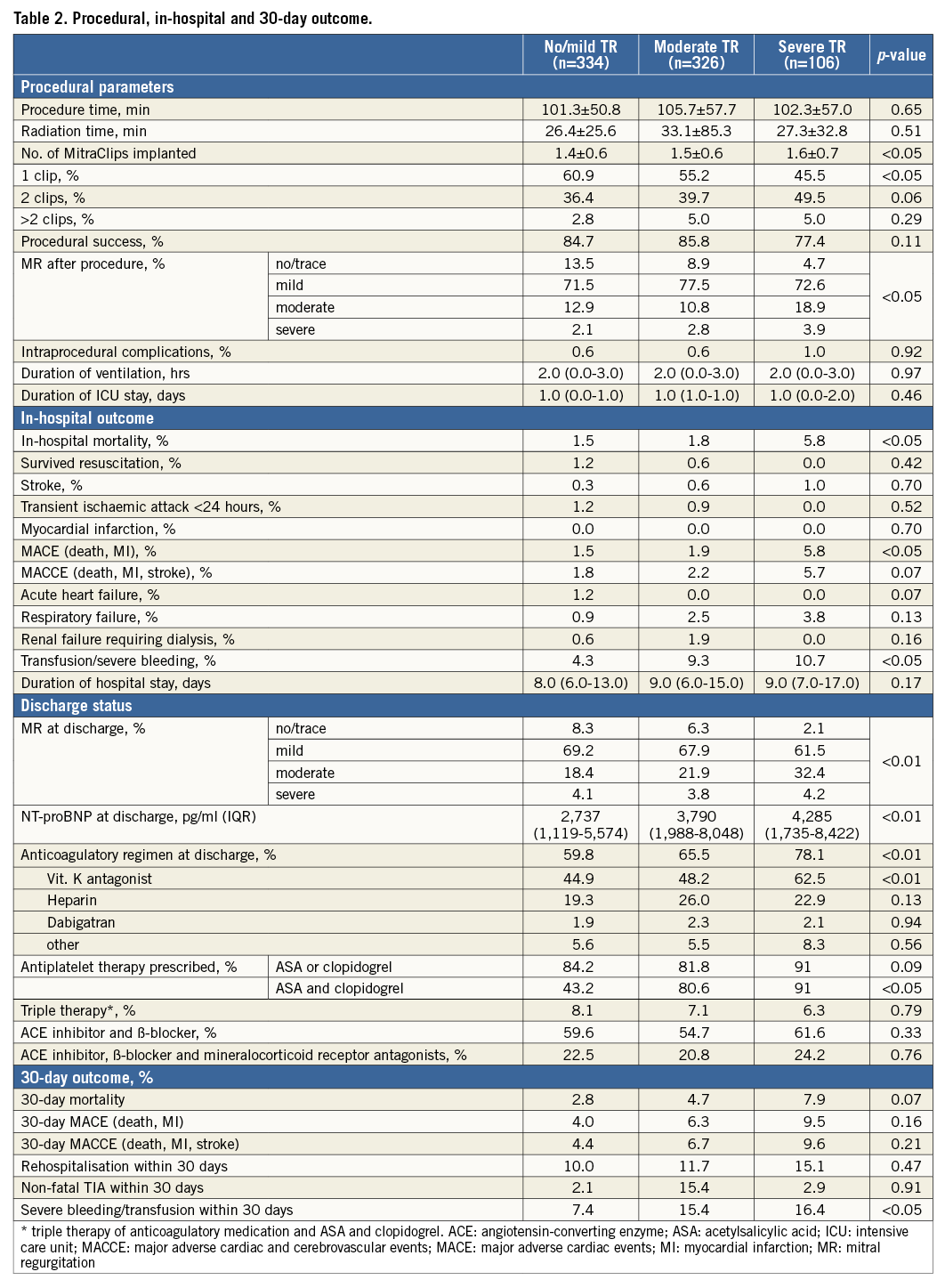
Among recorded in-hospital complications (survived resuscitation, low cardiac output failure, severe vascular complication, pericardial effusion or renal failure requiring dialysis) significant differences were only seen for transfusion/severe bleeding and associated with increasing TR severity (no/mild TR 4.3%, moderate TR 9.3%, severe TR 10.7%, p<0.05).
At hospital discharge, residual moderate MR was more frequent in patients with severe TR (no/mild TR 18.4%, moderate TR 21.9%, severe TR 32.3%). Furthermore, patients with severe TR were more frequently on vitamin-K antagonists (p<0.01), resulting in higher rates of severe bleeding (no/mild TR 7.4%, moderate TR 15.4%, severe TR 16.4%, p<0.05). Mortality, MACE, MACCE and rehospitalisation within 30 days were not significantly different, but with a clear trend towards worse outcome for moderate and severe TR.
Clinical variables (NYHA classification [p=0.91] and EQ-5D score [p=0.67]) indicated no significant differences up to 30-day follow-up, with a relevant number of patients still graded NYHA Class IV (no/mild TR 11.8%, moderate TR 10.9%, severe TR 11.1%).
ONE-YEAR FOLLOW-UP
Overall, mortality rates up to one-year follow-up were highest for patients with severe TR (no/mild TR 14.6%, moderate TR 21.0%, severe TR 34.0%, p<0.001). Total one-year MACE and MACCE rates were highest for severe TR (p<0.01) (Table 3, Figure 1). Although not significant, a strong trend was seen for higher rates of severe bleeding with increasing TR severity (no/mild TR 11.1%, moderate TR 17.6%, severe TR 23.1%, p=0.05). No differences were found for rehospitalisation (p=0.64), reintervention for mitral valve disease (p=0.13) or NYHA class distribution (p=0.07), again with a high proportion of patients in NYHA Class IV (no/mild TR 19.8%, moderate TR 11.1%, severe TR 18.4%). Concerning the anticoagulatory regimen, patients with severe TR received vitamin-K antagonists significantly more frequently (no/mild TR 47.6%, moderate TR 53.5%, severe TR 72.0%, p<0.01), whereas there was no difference in either antiplatelet (p=0.10) or triple therapy (p=0.16) (Table 3).
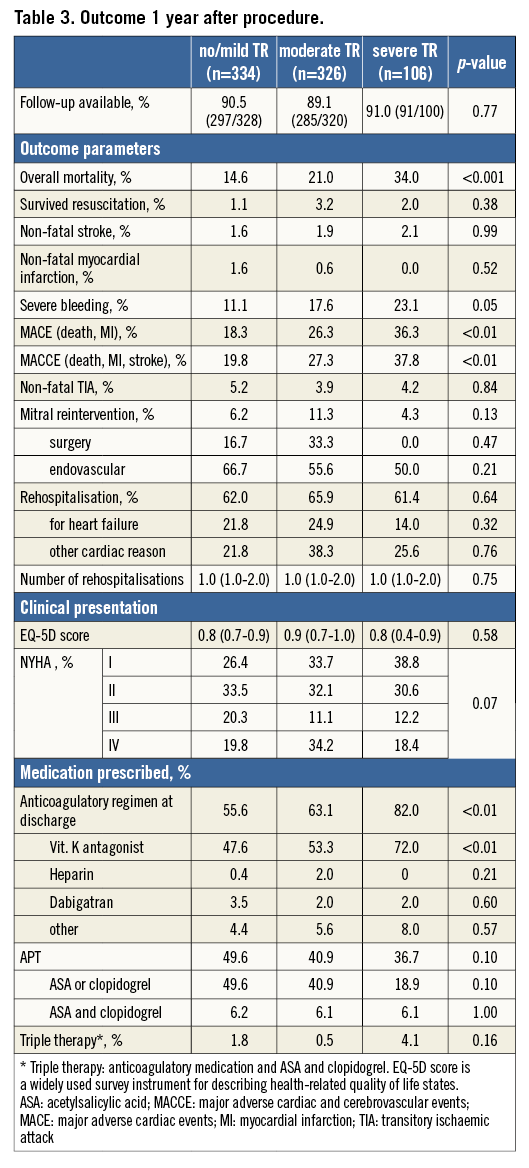
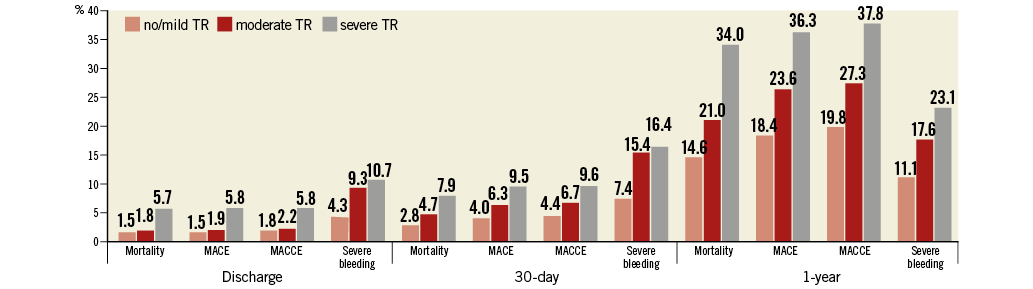
Figure 1. Mortality, MACE and MACCE rates, as well as severe intra-hospital bleeding, for 30-day and one-year follow-up.
An increasing risk for one-year mortality was related with increasing TR grades (Kaplan-Meier analysis, p<0.0001) (Figure 2A). Again, no differences were found for rehospitalisation (p=0.78) and the combined endpoint of death and rehospitalisation (p=0.36). Subgroup analysis for MR aetiology showed a significant impact on one-year mortality TR grade in degenerative MR (log-rank test, p<0.0001, Figure 2B; functional MR: log-rank test, p=0.055, Figure 2C). Pairwise log-rank tests indicated significantly decreased survival rates for severe TR, irrespective of the underlying MR aetiology (degenerative MR: moderate vs. no/mild TR: p=0.72; severe vs. no/mild TR: p=0.0003, and functional MR: moderate vs. no/mild TR: p=0.08; severe vs. no/mild TR: p=0.04).
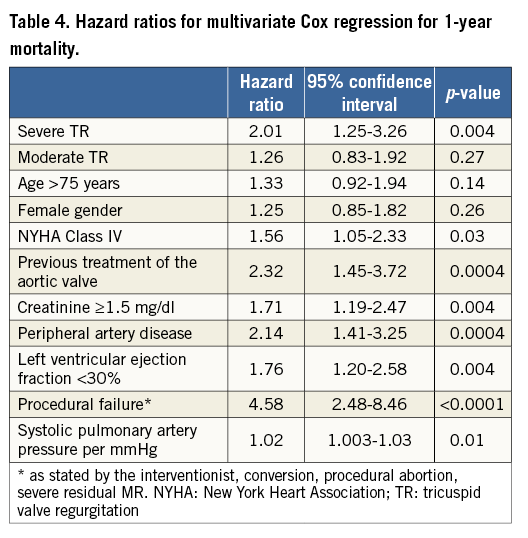
After multivariate Cox regression, severe TR, but not moderate TR, was significantly associated with increasing mortality rates (HR 2.01, 95% CI: 1.25-3.26, p=0.004) (Table 4), whereas MR aetiology did not prove to be significant in the stepwise forward selection model.
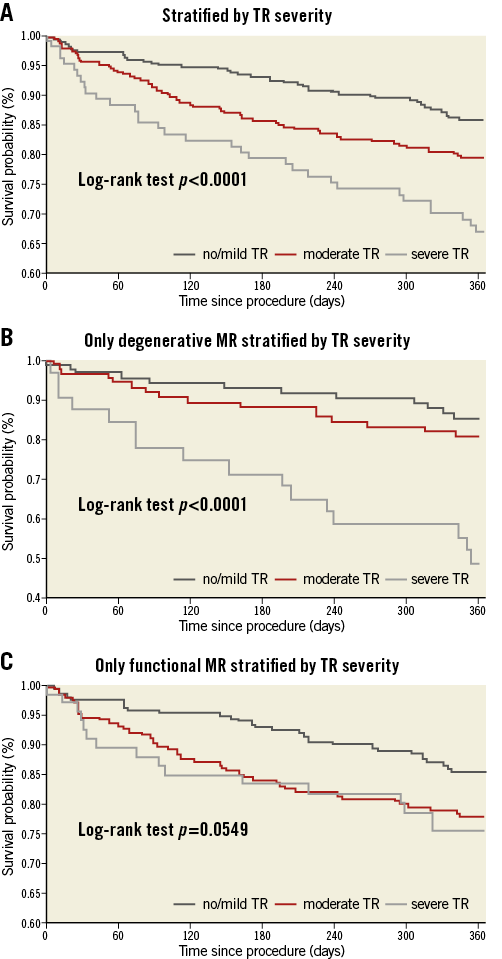
Figure 2. Kaplan-Meier curves for one-year mortality rates. A) Stratified by TR severity. B) Only degenerative MR stratified by TR severity. C) Only functional MR stratified by TR severity.
Discussion
The present study investigated the influence of concomitant TR on patient outcomes up to one year after MitraClip implantation.
There are three important findings to report: (i) the procedural success rate is not affected by TR severity; (ii) higher mortality rates are seen for moderate and severe TR, but only severe TR represents a predictor for one-year mortality; (iii) the risk for severe bleeding is higher with increasing TR grades, but this supposedly derives from a more frequent prescription of anticoagulatory medications due to higher rates of atrial fibrillation.
The TRAMI registry represents the largest cohort of patients worldwide treated by MitraClip implantation for relevant MR and reflects real-world practice. Although increasing TR severity is associated with a higher number of relevant comorbidities, procedural success rates were high (84.2%) throughout all subgroups.
Severe TR proved to be associated with adverse outcome and represents a predictor of death in this cohort. The association of TR severity and higher mortality rates is already known4. There is evidence that patients suffering from isolated severe TR have significantly lower survival rates than patients with moderate TR8.
Pulmonary hypertension leads to a worsening of TR severity but can improve after successful therapy9. Despite these findings, moderate or severe TR is associated with adverse events, even if pulmonary hypertension or left ventricular dysfunction is absent4.
In the present cohort, a significantly higher prevalence of pulmonary hypertension was found for increasing TR severity. Yet, significantly increased mortality, MACE and MACCE rates were seen even without elevated PAP sys. As pulmonary hypertension is strongly associated with TR, it is only one of many reasons that affect right ventricular function and size. It can alter the tricuspid annulus and consequently lead to relevant TR10. Although pacemaker and ICD leads increase the risk for relevant TR11, there was no difference among the subgroups in the prevalence of implanted cardiac pacing devices.
The main reason for functional TR is left-sided heart disease, mainly due to mitral valve pathologies. Yet, surgical correction of MR does not always lead to an improvement of TR1,10. Since fast progression of even mild TR is frequent12, guideline recommendations favour tricuspid valve correction in patients undergoing left-sided valvular surgery13.
In the present cohort, the mean number of implanted clips was significantly higher with increasing TR grades. A possible explanation might be that moderate and especially severe TR indicate a more serious deterioration of cardiac function due to advanced disease processes, including increased cardiac chamber sizes, higher rates of atrial fibrillation and pulmonary hypertension10. Therefore, a “two or more clip strategy” seemed to be the appropriate treatment option in a high number of patients.
For individuals treated by MitraClip implantation, TR is not routinely addressed at the time of intervention, although first successful implantations of the MitraClip device to treat relevant TR have been described14. Tricuspid regurgitation severity has been shown to improve in one third of patients successfully treated by MitraClip implantation, especially in those suffering from high systolic pulmonary artery pressure15. Due to its impact on prognosis, relevant TR should always be assessed and included in treatment considerations in patients undergoing MitraClip implantation. In order to decide whether a combined or staged approach of MR/TR disease should be pursued in each individual patient, further clinical experience and prospective studies are needed to confirm the safety and feasibility of interventional TR treatment.
Significant differences in atrial fibrillation and substantial differences in anticoagulatory medication prescribed are presumably the main reason for the higher bleeding rates found with increasing TR severity. After MitraClip implantation, the additional application of antiplatelet therapy is recommended. Interestingly, the increased bleeding risk obviously does not derive from the combination of anticoagulatory medication and dual antiplatelet therapy, as there were no differences found among the groups. Since severe bleeding complications affect morbidity and mortality, the medical regimen should be strictly revised, especially in patients already receiving anticoagulatory treatment. In this context, it has to be emphasised that a very limited number of patients were pre-treated with an LAA occlusion device (no/mild TR 0.3%, moderate TR 0.9%, severe TR 0.9%, p=0.57).
It might be worth noting that higher mortality rates are seen for moderate and severe TR, but only severe TR represents a predictor for one-year mortality. This appears to be relevant because the recorded rates for mortality, MACE and MACCE already differ significantly for the intra-hospital course (mortality: 1.8% vs. 5.8%; MACE: 1.9% vs. 5.8%; and MACCE: 2.2% vs. 5.8%, for moderate and severe TR, respectively). Different outcomes regarding survival were also seen when further stratifying patients to the underlying MR aetiology. Severe TR proved to be an independent predictor of death, significantly associated with decreased survival. Despite the completely different pathology in functional and degenerative MR, Cox regression by stepwise forward selection did not indicate that the underlying MR pathology proved to be significant for survival.
Additionally, unacceptably high rates of residual moderate MR (32.4% at discharge) are seen for patients with severe TR. The one-year mortality rate is high (34%) and consistent with formerly described patient cohorts4. This fact should be considered when treating this subgroup. Untreated severe TR seems to determine prognosis. In such cases, sole MitraClip implantation can be considered only as a symptomatic treatment option.
Limitations to the study
As the presented data are registry-derived, there are inevitable limitations due to the lack of predefined inclusion or exclusion criteria. The German TRAMI registry included enrolment for all sites on a voluntary basis. The result is an inhomogeneous patient population reflecting a large range of non-consecutive enrolment across sites.
The most important limitation is that all data acquisition was site-reported. As for MR, the assessment of TR is known to fluctuate and be load-dependent. None of the collected echocardiography data within the TRAMI registry was core lab adjudicated; therefore, it must be assumed that the data are only of limited quality. Additionally, due to missing echocardiographic protocols, assessment of right heart diameters and functional status has not been sufficiently and adequately carried out. Therefore, right heart parameters are lacking in the TRAMI registry.
For most cases, it remains unclear whether the diagnosis of pulmonary hypertension is based on invasive measurements or is merely transferred from the past medical history. To that extent, the estimated PAP sys (via echocardiography) is the only variable available in this collective.
Another noteworthy limitation is that all follow-up data were collected by telephone interview only. Since follow-up echocardiographic measurements were not realised in the TRAMI registry, follow-up data on concomitant TR grades will not be available.
Conclusions
Moderate and severe TR in high-risk patients undergoing MitraClip implantation are associated with higher one-year mortality rates. Atrial fibrillation, anticoagulatory medication prescribed and severe bleeding increase with TR severity, while triple anticoagulatory therapy is very infrequent overall. Severe TR especially represents a surrogate parameter for worse outcome and is associated with high rates of residual moderate MR. Clearly, further treatment modalities directly addressing severe TR in patients with combined TR and MR are warranted in the future.
| Impact on daily practice For patients undergoing MitraClip implantation, concomitant TR is prognosis-relevant, as moderate and severe TR are associated with higher mortality and bleeding rates. Combined percutaneous interventions to treat both severe MR and TR in affected patients should be examined regarding patient safety, efficacy and impact on patient outcome. |
Funding
The majority of funding of TRAMI is provided by proprietary means of the Stiftung Institut für Herzinfarktforschung. Additional funding is provided by the Deutsche Herzstiftung e.V. Additional funding for biometrics is provided by Abbott Vascular Germany.
Conflict of interest statement
W. Schillinger and U. Schäfer have received lecture fees, study honoraria and travel expenses from and are members of the advisory board of Abbott. H. Sievert has received consulting fees, travel expenses, and study honoraria from Abbott. E. Lubos has received lecture fees, study honoraria and travel expenses from Abbott. The other authors have no conflicts of interest to declare.