Abstract
Aims: The aim of this study was to determine the impact of tricuspid regurgitation (TR) on mortality after edge-to-edge percutaneous mitral valve repair (PMVR), and also to analyse whether there is a difference in outcome between patients with improvement of TR after PMVR compared to patients without.
Methods and results: Out of 197 consecutive patients who underwent PMVR, 139 patients with available follow-up (mean 428±386 days) were included in the study. Concomitant moderate/severe TR was present in 58.3% of patients. Kaplan-Meier analysis showed significantly reduced overall survival for patients with moderate/severe TR, compared to patients with none/mild TR (p=0.003). Cox multivariate regression analysis revealed severe TR at baseline as the strongest independent predictor of mortality (HR 4.367, p=0.003). An improvement of the baseline moderate/severe TR was observed in 45.5% of patients at 30-day follow-up. Patients with no improvement of TR after PMVR had a higher midterm mortality compared to patients in whom TR improved (40.5% versus 11.4%, p=0.005).
Conclusions: More than half of patients undergoing PMVR have concomitant moderate/severe TR, which is associated with a worse outcome. Among predictors of mortality after edge-to-edge PMVR, severe TR at baseline is the most important. Patients with no improvement of TR at 30 days after PMVR have a significantly higher mortality at follow-up.
Abbreviations
AF: atrial fibrillation
CKD: chronic kidney disease
GFR: glomerular filtration rate
LV: left ventricle
LVEDD: left ventricular end-diastolic diameter
LVEF: left ventricular ejection fraction
MR: mitral regurgitation
PMVR: percutaneous mitral valve repair
RV: right ventricle
RVEDD: right ventricular end-diastolic diameter
sPAP: systolic pulmonary artery pressure
TAPSE: tricuspid annular plane systolic excursion
TEE: transoesophageal echocardiography
TR: tricuspid regurgitation
TTE: transthoracic echocardiography
Introduction
Untreated severe tricuspid regurgitation (TR) is associated with worse survival independent of right ventricular (RV) function with a mortality rate of up to 36% at one-year follow-up1,2. In patients undergoing mitral valve surgery, the prevalence of TR is >30%3 and, left untreated, significant TR impairs long-term survival4. There is increasing evidence that a surgical approach with tricuspid valve repair in patients undergoing left-sided valve surgery improves outcome5-8, which is reflected by current guidelines9,10.
Edge-to-edge percutaneous mitral valve repair (PMVR) is an effective therapeutic option for inoperable or high surgical risk patients with symptomatic mitral regurgitation (MR)11-13. Compared to surgical candidates, most of these patients are suffering from a more advanced heart failure. As a consequence, the prevalence of TR is higher14. Only a few studies have aimed to identify predictors of long-term outcome after edge-to-edge PMVR14-17. Significant TR was one of the predictors14 for the combined endpoint death and rehospitalisation, whereas data on mortality are limited.
The aim of the present study was to determine the impact of TR on mortality after successful edge-to-edge PMVR and to analyse the proportion of patients who show an improvement of TR severity and whether there is a difference in outcome between patients with and without improvement of TR after PMVR.
Methods
STUDY POPULATION
Between October 2011 and June 2015, 197 consecutive patients underwent a MitraClip® procedure (Abbott Vascular, Santa Clara, CA, USA) in one institution by the same chief operator (Joachim Schofer) and 139 patients with available follow-up data were included in the study.
All patients were discussed by an interdisciplinary Heart Team and deemed to be at high surgical risk, which was defined as a logistic EuroSCORE I mortality rate ≥15% or specific risk factors associated with high perioperative morbidity and mortality.
PROCEDURAL TECHNIQUE
PMVR was performed under general anaesthesia with fluoroscopic, 2D and 3D transoesophageal guidance. The procedural steps are as previously described18,19. Procedural success was defined as implantation of at least one clip with MR reduction of at least one degree and/or residual MR ≤2. Residual MR grade was assessed by post-procedural transoesophageal echocardiography (TEE), under the same blood pressure as pre-procedural. A serious event was defined as the occurrence of death, stroke, myocardial infarction, cardiac tamponade or clip embolisation.
ECHOCARDIOGRAPHY
All patients underwent transthoracic echocardiography (TTE) and TEE at baseline, and TTE at 30 days. MR was defined as degenerative in the presence of primary pathologies of the leaflets and/or apparatus of the mitral valve, and as functional if MR developed in the context of ischaemic heart disease, dilated cardiomyopathy or severe LA dilatation, despite a structurally normal mitral valve10,20. The severity of MR and TR was classified as none/trace, mild, moderate or severe based on current recommendations9,20. MR severity was graded using vena contracta (VC) width and effective regurgitant orifice area (EROA) and regurgitant volume measured by the proximal isovelocity surface area (PISA) method20.
TR severity was assessed using the semi-quantitative parameters VC width and systolic hepatic flow reversal. A VC width ≥7 mm defined severe TR. Qualitative parameters such as colour flow TR jet and continuous wave Doppler signal of the TR jet were used to distinguish between none/trivial, mild and moderate TR20.
Systolic pulmonary artery pressure (sPAP) was calculated from peak TR jet velocity, using the simplified Bernoulli equation and adding an assumed right atrial pressure20,21.
FOLLOW-UP
Clinical follow-up was obtained according to our routine clinical practice by clinical visits or phone consultations. Thirty-day echocardiographic follow-up, defined as “early follow-up”, was obtained in 95.7% of patients. Six patients died before the echocardiographic control could be performed. Cardiovascular death was defined as death due to heart failure, myocardial infarction, stroke or any procedure-related death.
STATISTICS
Continuous variables are presented as mean±standard deviation and compared using the unpaired Student’s t-test or Mann-Whitney U test as appropriate. Categorical data are presented as counts (percentages) and compared by the Pearson chi-square or Fisher’s exact test. All p-values reported are two-tailed and p<0.05 was considered statistically significant. Survival curves were generated with the use of the Kaplan-Meier method, and log-rank tests were used to evaluate differences between groups. A multivariable analysis for mortality was performed using a Cox regression analysis with stepwise forward selection, which incorporated baseline clinical variables with a significance level of p<0.05 at univariate analysis. Statistical analysis was performed using GraphPad Prism version 7 (GraphPad Software, San Diego, CA, USA) and SPSS software, Version 20.0 (IBM Corp., Armonk, NY, USA).
Results
PATIENT CHARACTERISTICS
Baseline characteristics are shown in Table 1 and Table 2. Mean age was 76.4±7.5 years, 61.2% were male, mean logistic EuroSCORE I was 22.5±13.9% and the majority of patients were in NYHA Class III or IV (84.9%, n=118); 138/139 patients had moderate or severe MR, and the aetiology was functional in 84.2% of patients. Moderate or severe TR was present in 58.3% of patients (n=81) (Figure 1).
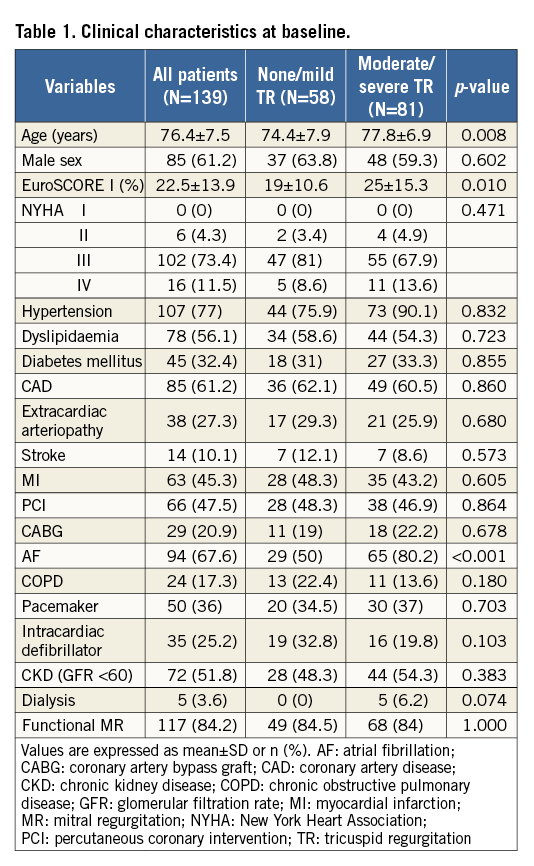
Compared to patients with none/mild TR (n=58), patients with moderate/severe TR (n=81) were significantly older (77.8±6.9 versus 74.4±7.9 years, p=0.008), had a higher EuroSCORE I (25±15.3 versus 19±10.6%, p=0.01) and a higher prevalence of AF (80.2% versus 50%, p<0.001) (Table 1).
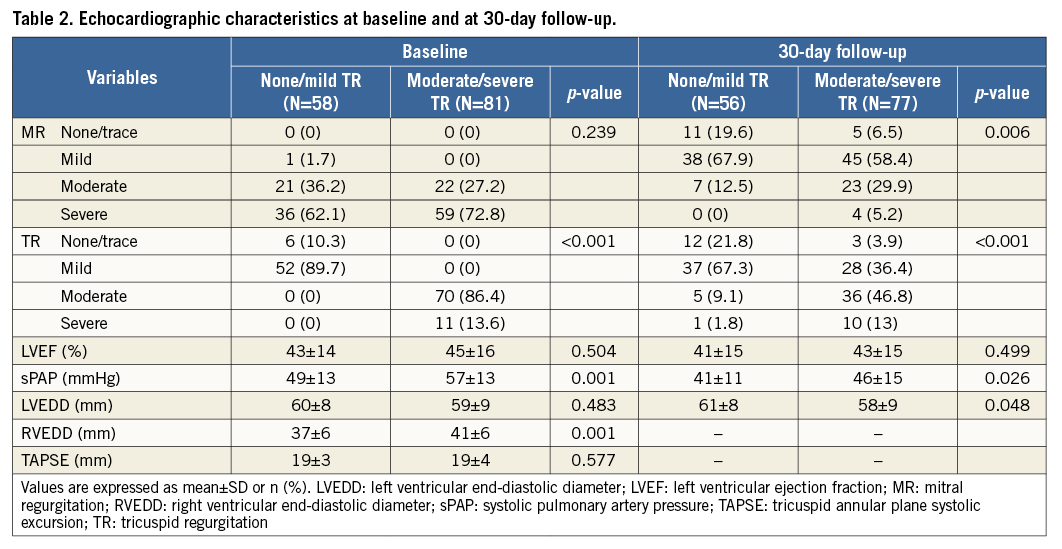
Echocardiography revealed that patients with moderate/severe TR had a larger RV diameter and higher sPAP compared to patients with none/mild TR. MR severity and LV dimension and function were comparable between the groups (Table 2).
30-DAY OUTCOME
Significant improvement of MR was achieved in most patients with a procedural success rate of 97.8%. The mortality rate at 30 days was 5% (7/139): this was due to heart failure in six patients (86%), while one patient died because of acute renal failure. No other serious events were observed. Thirty-day echocardiographic follow-up was obtained in 96.6% (56/58) of patients with none/mild TR and 95% (77/81) of patients with moderate/severe TR at baseline (Table 2). The incidence of moderate/severe MR at 30-day follow-up was significantly higher in patients with moderate/severe TR at baseline (p=0.006).
Although sPAP at 30 days was improved in both groups, it was significantly higher in patients with moderate/severe TR at baseline (46±15 versus 41±11 mmHg, p=0.026). At 30 days, we did not observe reverse remodelling of the LV (Table 2).
MIDTERM OUTCOME
At a mean follow-up of 428±386 days, the cumulative mortality rate was 25.2% (35/139 patients) (Figure 1): 26/35 patients (74%) experienced cardiovascular death (due to heart failure in 22 patients, myocardial infarction in three and stroke in one patient), 2/35 patients died because of renal failure, 3/35 patients because of cancer and in 4/35 patients the cause of death was unknown.
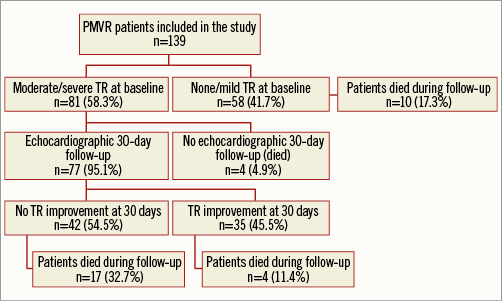
Figure 1. Flow chart showing 139 patients included in the study. Mean follow-up 428 days.
Kaplan-Meier analysis at 24 months showed a significantly reduced overall survival in patients with moderate/severe TR, compared to patients with none/mild TR (p=0.003) (Figure 2).
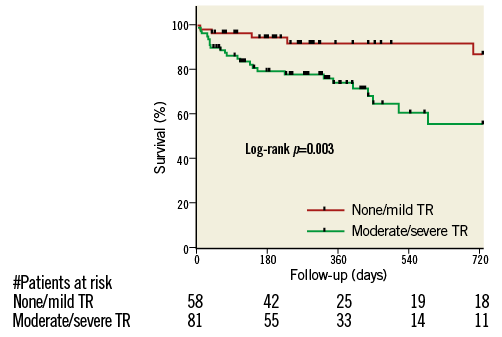
Figure 2. Kaplan-Meier survival curves stratified by TR severity at baseline.
PREDICTORS OF MORTALITY
Univariate analysis revealed EuroSCORE I ≥20%, NYHA functional Class IV, AF, chronic kidney disease (CKD), severe TR at baseline, sPAP ≥60 mmHg and moderate/severe residual MR grade as significant predictors of mortality (Table 3).
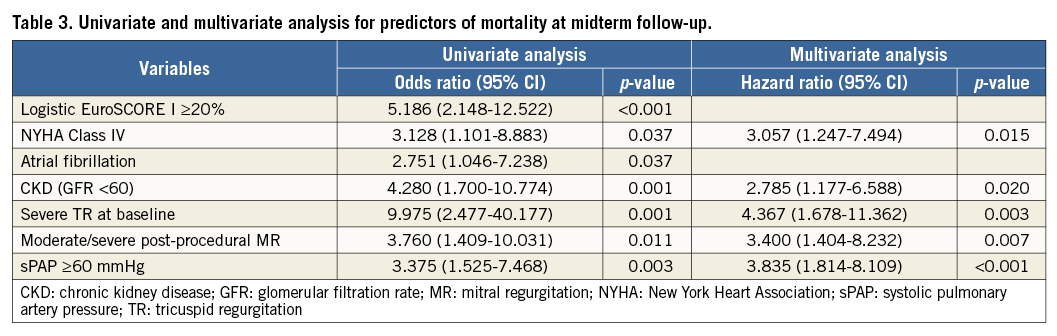
Multivariate Cox regression analyses showed severe TR at baseline as the strongest independent predictor of midterm mortality (HR 4.367, p=0.003). In addition, sPAP ≥60 mmHg (HR 3.835, p<0.001), residual moderate/severe MR (HR 3.400, p=0.007), NYHA Class IV (HR 3.057, p=0.015) and CKD (HR 2.785, p=0.020) were significantly associated with mortality (Table 3).
TR IMPROVEMENT AND IMPACT ON OUTCOME
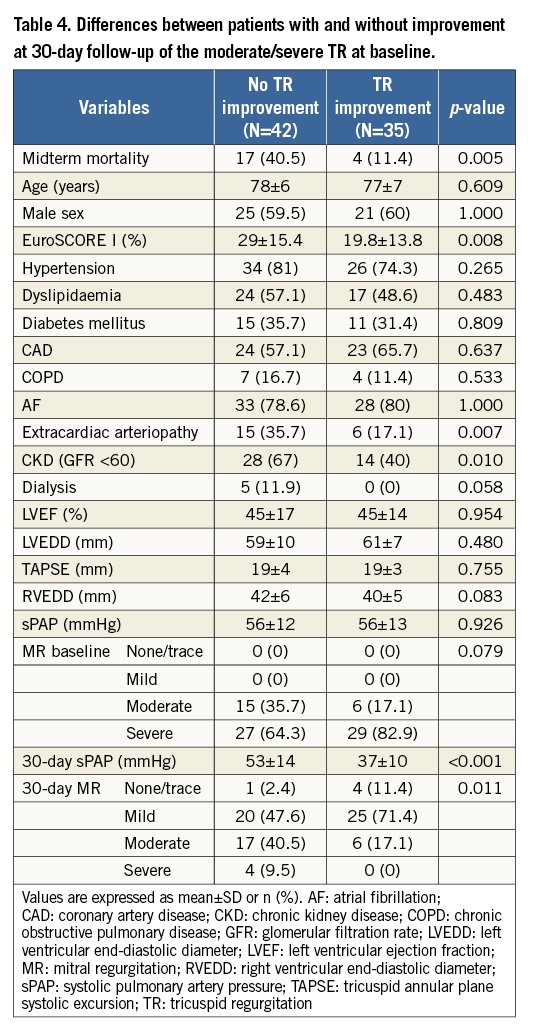
An early improvement at 30 days of TR (at least one grade) was observed in 45.5% of patients with moderate/severe TR at baseline (35/77 patients). At a mean follow-up of 428±386 days, patients without early improvement of moderate/severe TR had a significantly higher mortality rate compared to patients in whom TR improved (40.5% versus 11.4%, p=0.005) (Table 4).
Kaplan-Meier survival at 24 months was significantly reduced in patients without early improvement of the moderate/severe TR (p=0.033) (Figure 3).
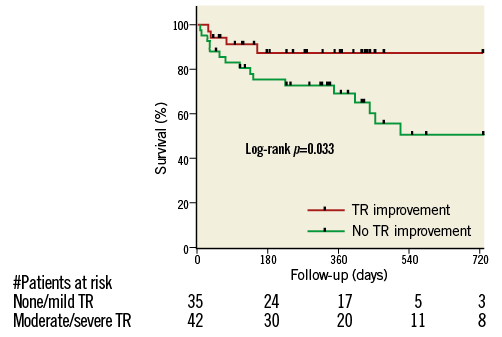
Figure 3. Kaplan-Meier survival curves stratified by TR improvement.
The absence of TR improvement was associated with a higher EuroSCORE I (29±15.4 versus 19.8±13.8%, p=0.008), a higher incidence of extracardiac arteriopathy (35.7% versus 17.1%, p=0.007) and CKD (67% versus 40%, p=0.010). LV diameter and function were not different between the two groups, but there was a trend for larger right ventricular end-diastolic diameter (RVEDD) at baseline in patients without TR improvement (42±6 versus 40±5 mm, p=0.083). sPAP at baseline was not significantly different between patients with and without TR improvement (56±13 mmHg versus 56±12 mmHg, p=926); however, at 30-day follow-up it was significantly lower in patients with TR improvement (37±10 versus 53±14 mmHg, p<0.001) (Table 4).
Discussion
The main findings of the present study are:
1. More than half of patients undergoing PMVR have concomitant moderate or severe TR (58.3%), which is associated with worse outcome.
2. The strongest predictor for mortality at follow-up is severe TR at baseline.
3. TR improves in 45.5% of patients with moderate/severe TR at baseline after successful PMVR and this improvement is observed early.
4. Patients with no early improvement of TR severity have a significantly higher mortality.
INCIDENCE OF TR IN PATIENTS UNDERGOING EDGE-TO-EDGE PMVR
TR is a common finding in patients undergoing surgical intervention for MR. The presence of moderate/severe compared to none/mild TR at baseline negatively impacts on the outcome after surgery4, and correction of concomitant TR in these patients exerts beneficial effects5-8.
In the present study, the prevalence of TR in patients undergoing PMVR was as high as 95.7% (133/139), with 58.3% suffering from moderate or severe TR. This is higher than that described by Ohno et al, who found a moderate or severe TR in 32.2% of patients14. This difference may be explained by differences in patient baseline characteristics. In particular, patients in our study were older, with higher sPAP and a higher prevalence of AF, which are known risk factors for functional TR by causing tricuspid annular dilatation22-24. TR severity in our study was associated with larger RV basal diameter and higher sPAP. This could be the cause of more TR, but on the other hand also the consequence of severe TR, which results in RV dilatation with restricted LV diastolic filling, which increases RV afterload and thereby closes a vicious cycle.
CLINICAL OUTCOME AND PREDICTORS OF MORTALITY AT FOLLOW-UP
In the present study, all-cause midterm mortality at a mean follow-up of 428±386 days was 25.2%, the majority (74.3%) experiencing a cardiovascular death. In the TRAMI registry17, with almost identical patient demographic characteristics, cardiovascular mortality was only 37%. However, the cause of death was unknown in 35.5% of the patients in the TRAMI registry.
In line with other studies, including the TRAMI17 and GRASP registry14, we found a prognostic benefit of MR reduction, suggesting that a maximal MR reduction should be attempted to optimise the outcome14,16,17. However, even in the presence of successful reduction of MR, two-year mortality among patients with moderate/severe TR was significantly higher (Figure 2).
In a study comprising 5,223 patients undergoing echocardiography for different reasons1, TR was associated with worse survival, independently of age, biventricular systolic function, RV size and dilatation of the inferior vena cava (IVC). After mitral valve surgery, severe TR, even if not present at the time of surgery, develops in more than 50% of patients over time, if the tricuspid annulus is >40 mm25, and significant TR is a predictor for worse survival after mitral valve surgery4.
Few studies have aimed to identify predictors of long-term outcome after edge-to-edge PMVR15,16. In our study, Cox regression analysis revealed that severe baseline TR was the strongest predictor of mortality (HR 4.367, p=0.003).
In the GRASP registry14, only the combined endpoint of death and re-hospitalisation was significantly associated with severe TR, whereas no association was found between baseline TR and mortality alone. Other studies have also found that TR severity, among several other predictors, is a predictor of mortality after PMVR16,17. However, in none of those studies was the proportion of patients who showed an improvement in TR severity after successful PMVR analysed. In addition, no data existed on the outcome of patients with improvement of TR after PMVR compared to patients without.
TR IMPROVEMENT AT EARLY FOLLOW-UP AND IMPACT ON OUTCOME
Successful edge-to-edge PMVR was associated with a 30-day improvement of TR in 45.5% of patients with moderate or severe TR at baseline. This finding is in line with other studies14,26.
In our study, patients with no improvement of TR had a trend for a larger basal diameter of the RV at baseline and a higher sPAP at 30-day follow-up (Table 4). These might be either the cause or the consequence of persistent significant TR, as discussed earlier. Mortality at midterm follow-up was significantly higher among patients with no improvement of moderate/severe TR (40.5% versus 11.4%, p=0.005). Kaplan-Meier survival curves stratified by TR improvement diverge significantly. Whereas patients with improvement of TR have a quite stable survival over two years of follow-up, in patients with no improvement mortality increases over time (Figure 3).
In future studies, it would be important to identify predictors of TR improvement after PMVR. For those patients without improvement, percutaneous interventions to reduce TR, which are currently under development, should be considered27,28.
Limitations
This is a single-centre registry with its inherent limitations. The sample size is relatively small; however, it comprises all-comer patients who underwent edge-to-edge PMVR with available follow-up. The criteria for quantification of TR was semi-quantitative based on VC, and qualitative to differentiate between none/trace, mild and moderate TR. However, these analyses were conducted by dedicated, highly experienced physicians using validated methods following current guidelines. Because follow-up data were obtained from routine echocardiography, we do not have the exact data for RV function and dimension in most of the patients.
Conclusions
More than half of patients undergoing PMVR have a concomitant moderate or severe TR, which is associated with worse outcome. Among the predictors for mortality after edge-to-edge PMVR, severe TR at baseline is the most important. Patients with moderate or severe TR without an improvement at 30 days have a worse outcome compared to patients in whom TR improves. An early indication for PMVR before the onset of severe TR might be considered, and for patients with moderate/severe TR it remains to be shown whether percutaneous approaches to reduce TR could improve patient outcome.
| Impact on daily practice Patients with severe MR, if accompanied by moderate/severe TR, have a higher mortality after edge-to-edge PMVR compared to patients without significant TR. Patients with no improvement of moderate or severe TR 30 days after PMVR have a significantly higher mortality compared to patients with improvement. This should be taken into consideration by the Heart Team. Because there is a 45% chance of TR improvement at 30 days after PMVR, we would not recommend a combined percutaneous MR and TR repair in one session but may consider a percutaneous TR repair if severe TR is persisting. |
Conflict of interest statement
The authors have no conflicts of interest to declare.