Tricuspid valves surgeries are preferably performed fully endoscopically via right lateral mini-thoracotomy using extracorporeal circulation but without cardioplegic arrest (minimally invasive beating-heart tricuspid valve surgery [MIC-TVS]). Transcatheter edge-to-edge repair (TEER) is an increasingly performed alternative in patients with symptomatic tricuspid regurgitation (TR) at high surgical risk. Contemporary MIC-TVS and TEER outcomes have not been compared. The TRI-SCORE has been proposed as a risk stratification in TR patients. Therefore, the objective of this study was to compare clinical outcomes in patients with TR undergoing TEER versus MIC-TVS in an all-comers cohort and to stratify outcomes according to the TRI-SCORE.
This is a retrospective observational multicentre study of patients treated for TR with TEER using edge-to-edge repair (n=211) or isolated MIC-TVS beating-heart procedures (n=28) between 2016 and 2021.
Endpoints were all-cause mortality at 30 days and 1 year, grade of TR at discharge and 1 year, and all-cause mortality at 1 year, stratified by TRI-SCORE (<6 vs ≥6 points). Kaplan-Meier estimation was used for survival analyses, and curves were compared using the log-rank test.
Baseline parameters dichotomised by the 2 different treatment groups are shown in Figure 1A.
TR reduction in comparison to the baseline was significantly more pronounced in the MIC-TVS group (p<0.001) (Figure 1B). Thirty-day mortality was 2.8% (6/211) in the TEER cohort versus 10.7% (3/28) in the MIC-TVS cohort (p=0.07). The overall survival at 1 year was 80.4% after TEER and 78.6% after MIC-TVS (p=0.67) (Figure 1C).
One-year survival stratified by TRI-SCORE <6 versus ≥6 points was 89.7% versus 67.6% in TEER patients (p<0.01) (Figure 1D)1 and 90.0% versus 50.0% in MIC-TVS patients (p<0.01) (Figure 1E)1.
At 6 months, 100% (171/171) of TEER patients and 95.4% (21/22) of MIC-TVS patients were in NYHA Class I/II (p=1.00), and cardiac-related rehospitalisation occurred in 10.5% (18/171) in the TEER group and in 18.2% (4/22) in the MIC-TVS group (p=0.28).
This study compared 2 TR therapy techniques and herein shows the following:
- 1. Thirty-day mortality tended to be higher with MIC-TVS, but survival analysis showed no significant differences at 1 year.
- 2. MIC-TVS led to a significantly more efficient reduction in TR.
- 3. A TRI-SCORE of ≥6 points resulted in significantly lower survival rates in both groups, indicating that patients should be referred for treatment at an earlier stage of TR.
Because of its high prevalence and association with increased mortality and morbidity, surgery for isolated TR is rarely performed. MIC-TVS has been established as an evolved strategy of surgical treatment. It is believed to result in improved outcomes2. However, many TR patients are at high surgical risk, and therefore, catheter-based interventions for TR are increasingly performed. TEER is the most widely used technique, and its safety and effectiveness have been proven3. Given the confounders affecting treatment allocation, the results should be interpreted with caution. The study groups consisted of elderly patients at high risk for surgery (predicted risk by the TRI-SCORE 8-14%).
In our analysis, both treatment options led to a continued reduction in TR, but the reduction was more significantly pronounced in MIC-TVS. The potential benefits of a more efficient TR reduction were possibly counterbalanced by the slightly higher postprocedural mortality rate. In addition, before initiation of any interventional or surgical treatment, best medical guideline-directed therapy should be enforced. Generally, it has to be determined in which patients TR reduction confers a prognostic benefit and in which patients best medical treatment as a third option of therapy needs to be taken into account, as done in a recent contemporary trial4.
Given that improvement of right ventricular function after TR correction is associated with improved prognosis and absolute elimination of TR may result in right heart failure, TEER seems an attractive option in high-risk patients with TR. The role of transcatheter tricuspid valve replacement and its prognostic benefits in this setting are currently under investigation.
The TRI-SCORE was highly predictive of perioperative mortality even in this small cohort of MIC-TVS patients. As seen in patients with preserved right ventricular and renal function (TRI-SCORE <6 points), mortality was low.
The limitations of our study are apparent through its retrospective design, with inherent consequences such as bias and differences in patient characteristics. Symptomatic assessment, such as the Kansas City Cardiomyopathy Questionnaire (KCCQ), was missing from the present study. Conclusions should be seen as hypothesis-generating.
Based on our analysis, the timing of invasive treatment in TR patients remains a clinical challenge. Currently, edge-to-edge repair is the most advanced transcatheter solution, and data on catheter-based tricuspid valve replacement are limited, therefore, more evidence is needed. Larger studies should be performed to confirm our findings and to assist Heart Teams in the decision-making process in patients with tricuspid valve disease. These results should form the basis for randomised trials of TEER versus MIC-TVS.
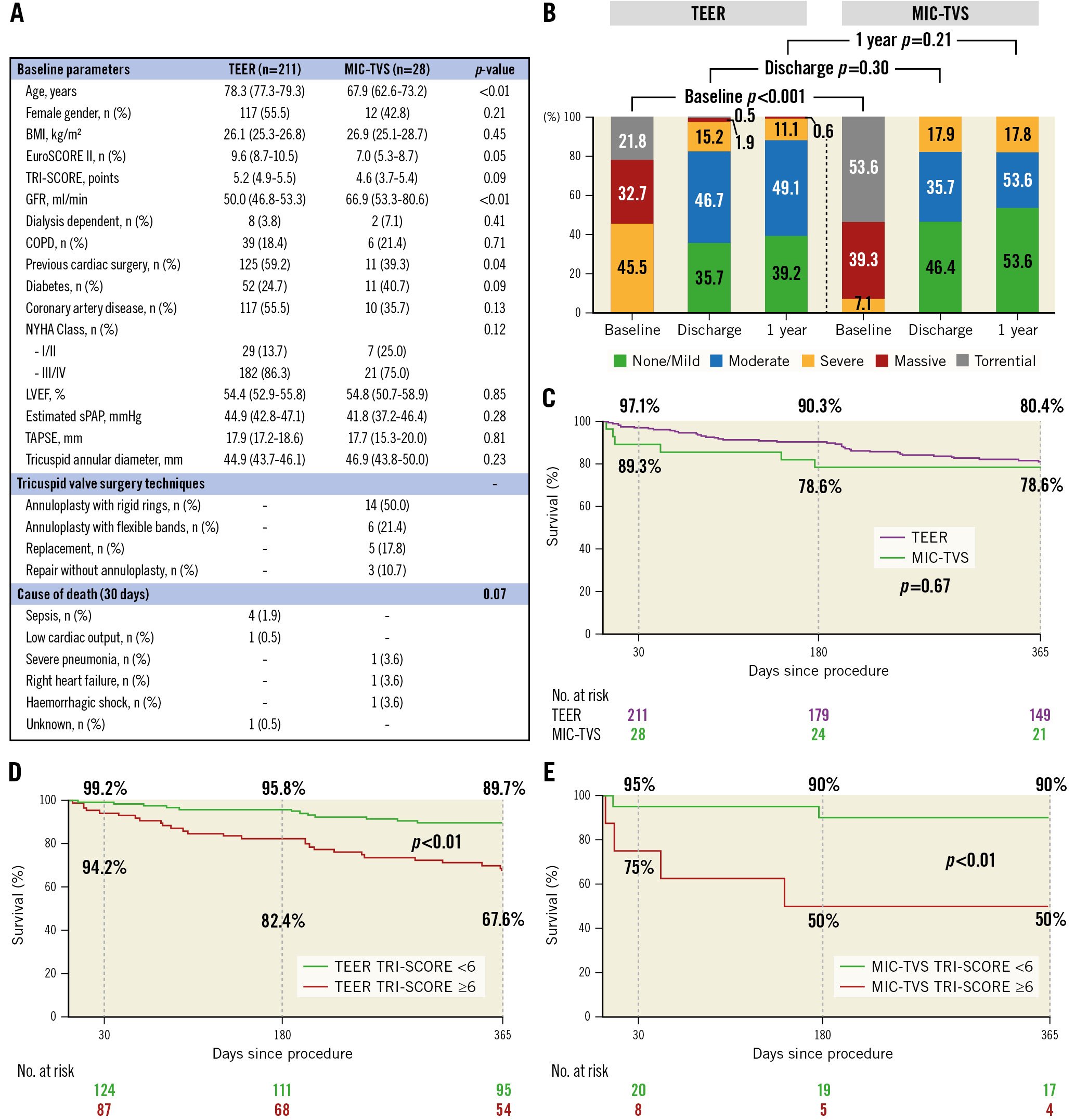
Figure 1. Transcatheter edge-to-edge valve repair versus minimally invasive beating-heart surgery of the tricuspid valve: an observational study. A) Table with baseline parameters, tricuspid valve surgery techniques of the MIC-TVS group and cause of death within 30 days for the TEER and MIC-TVS groups. Data are presented as n (%) or mean values with 95% lower and upper confidence intervals for continuous values. B) Changes in the severity of tricuspid regurgitation after the procedure at discharge and 1-year follow-up in the TEER and MIC-TVS groups. C) Kaplan-Meier curves of all-cause mortality within 1 year in the TEER and MIC-TVS groups. D) Survival after TEER stratified by preoperative TRI-SCORE ≥6 versus <6 points1. E) Survival after MIC-TVS stratified by preoperative TRI-SCORE ≥6 versus <6 points1. BMI: body mass index; COPD: chronic obstructive pulmonary disease; EuroSCORE: European System for Cardiac Operative Risk Evaluation; GFR: glomerular filtration rate; LVEF: left ventricular ejection fraction; MIC-TVS: minimally invasive beating-heart tricuspid valve surgery; NYHA: New York Heart Association; sPAP: systolic pulmonary artery pressure; TAPSE: tricuspid annular plane systolic excursion; TEER: transcatheter edge-to-edge repair
Funding
This research was not supported by grants from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest statement
M. Silaschi has received research grants from Medtronic and Artivion; and is an advisory board member of JenaValve. A. Sugiura has received honoraria for lectures from Edwards Lifesciences. T. Tanaka has been financially supported in part by fellowships from the Japanese College of Cardiology and the Uehara Memorial Foundation. G. Nickenig and S. Zimmer have received research funding from the Deutsche Forschungsgemeinschaft, the German Federal Ministry of Education and Research, the EU, Abbott, Edwards Lifesciences, and Medtronic; and have received honoraria for lectures or advisory boards from Abbott, Edwards Lifesciences, and Medtronic. M. Weber has received lecture or proctoring fees from Abbott and Edwards Lifesciences. The other authors have no conflicts of interest to declare.