In recent years, treatment with transcatheter edge-to-edge repair (TEER) for tricuspid regurgitation has increased rapidly123. For optimal guidance, the transoesophageal echocardiographic probe has to be moved between transgastric and various oesophageal positions4. Patients undergoing this procedure appear to be at higher risk for gastric bleeding, possibly because of increased vulnerability of the gastrointestinal mucosa. The probe manipulation during tricuspid TEER may further increase the risk for bleeding. The purpose of this study was to determine the prevalence and risk factors for injury caused by transoesophageal echocardiography probe manipulation during TEER for tricuspid regurgitation.
In this single-centre, retrospective, observational cohort study, we analysed data from all consecutive adult patients between November 2020 and July 2022 undergoing TEER for tricuspid regurgitation at our centre. All patients received gastroscopy before and after tricuspid TEER per protocol. Endoscopic findings were categorised into four groups (1: no lesion; 2: minor lesion; 3: major lesion; 4: endoscopic therapy necessary). Patients with either oesophageal and/or gastric lesions (groups 2-4) and those without injuries (group 1) were compared with regard to clinical characteristics and procedural features, including positional changes of the echocardiographic probe.
Overall, 40 patients were included in this analysis; the mean age was 78.7 (±6.9) years, and 45% were male. There were no significant differences in clinical characteristics between both groups concerning age, sex, pacemaker/defibrillator leads, ascites, European System for Cardiac Operative Risk Evaluation (EuroSCORE), diabetes, coronary heart disease, renal function, left ventricular ejection fraction, tricuspid regurgitation or the number of clips applied. Twenty-four patients (60%) had post-intervention gastric or oesophageal lesions (group 2-4), and 8 patients (20%) required endoscopic haemoclip therapy (group 4). The lesions were predominantly mid-oesophageal (62.5% of group 4) (Figure 1). Sixteen patients had no sign of injury at all (group 1). The procedural characteristics of tricuspid TEER did not differ between patients with lesions and those without lesions (mean procedure time 83.2 min±30.8 min vs 82.5 min±29.5 min; p=0.94; number of echocardiographic probe positional changes [oesophageal to transgastric] 6.9±2.6 vs 6.1±2.9; p=0.19; number of applied clips; 1.75±0.57 vs 1.83±0.56; p=0.65; reduction of tricuspid regurgitation; 1.75±0.57 vs 1.83±0.56; p=0.65). Arterial hypertension was more frequent (p=0.01) and body mass index (BMI) was lower (p=0.04) in patients with postinterventional injuries.
The rate of major bleeding complications in the setting of TEER for tricuspid regurgitation is reported in the literature to be approximately 11%1, which is in line with the severe upper gastric bleeding found in our study. Of the patients receiving endoscopic haemoclips, there was bleeding in five cases (12.5%): two patients had active bleeding, three patients had vessel stumps. The remaining three patients received prophylactic haemoclip therapy due to the physician’s individual decision. Compared with patients documented in the TRILUMINATE trial, our patient cohort had a higher EuroSCORE II and may, therefore, have been significantly frailer (8.7% vs 16.8%). Two patients had lesions in the hypopharynx, and three had lesions in the upper oesophagus. These lesions were probably caused by the probe intubation and not by the procedure itself.
We expected major lesions in the cardia and upper gastric areas, due to the frequent positional changes between the transgastric and mid-oesophageal areas4. Contrary to our assumption, most lesions were found in the mid-oesophageal region. Moreover, most lesions requiring a haemoclip intervention also occurred in the mid-oesophageal region at 25-32 cm from the dental arch (62.5%, 5/8 of group 4). This is probably because there is less space in the oesophagus compared to the stomach and each movement of the probe may have a greater impact on the mucosa.
Injuries of the oesophagus have been described for left-sided heart procedures, such as left atrial appendage closure or mitral TEER, by Freitas-Ferraz et al5. In contrast to their results, the procedure duration and positional changes did not predict lesions. Pre-existing gastritis was not a significant predictor of lesions after tricuspid TEER. The high prevalence of injuries following TEER for tricuspid regurgitation highlights the need to identify risk factors for potential bleeding and injury. In our study, we found more lesions in patients with arterial hypertension and lower BMI.
This is a retrospective, monocentric, cohort study. However, our study findings point to a possibly underappreciated complication with potentially life-threatening implications for an evolving therapy, especially in frail patients. The pressure applied to the mucosa by the transoesophageal echocardiography probe and the length of time the pressure is applied could themselves be potential risk factors for injuries. There are techniques to measure applied pressure with ablation catheters; this might help to clarify the problem of pressure points in future studies. Further investigations are needed to identify potential risk factors.
Injuries during TEER for tricuspid regurgitation of the mid-oesophageal region caused by the echocardiographic ultrasound probe manipulation do not seem to be predicted by the number of probe positional changes or the procedure duration in our small cohort. However, injuries of the oesophagus after tricuspid TEER are nonetheless common and more awareness should be brought to this subject; gastric injuries are less common.
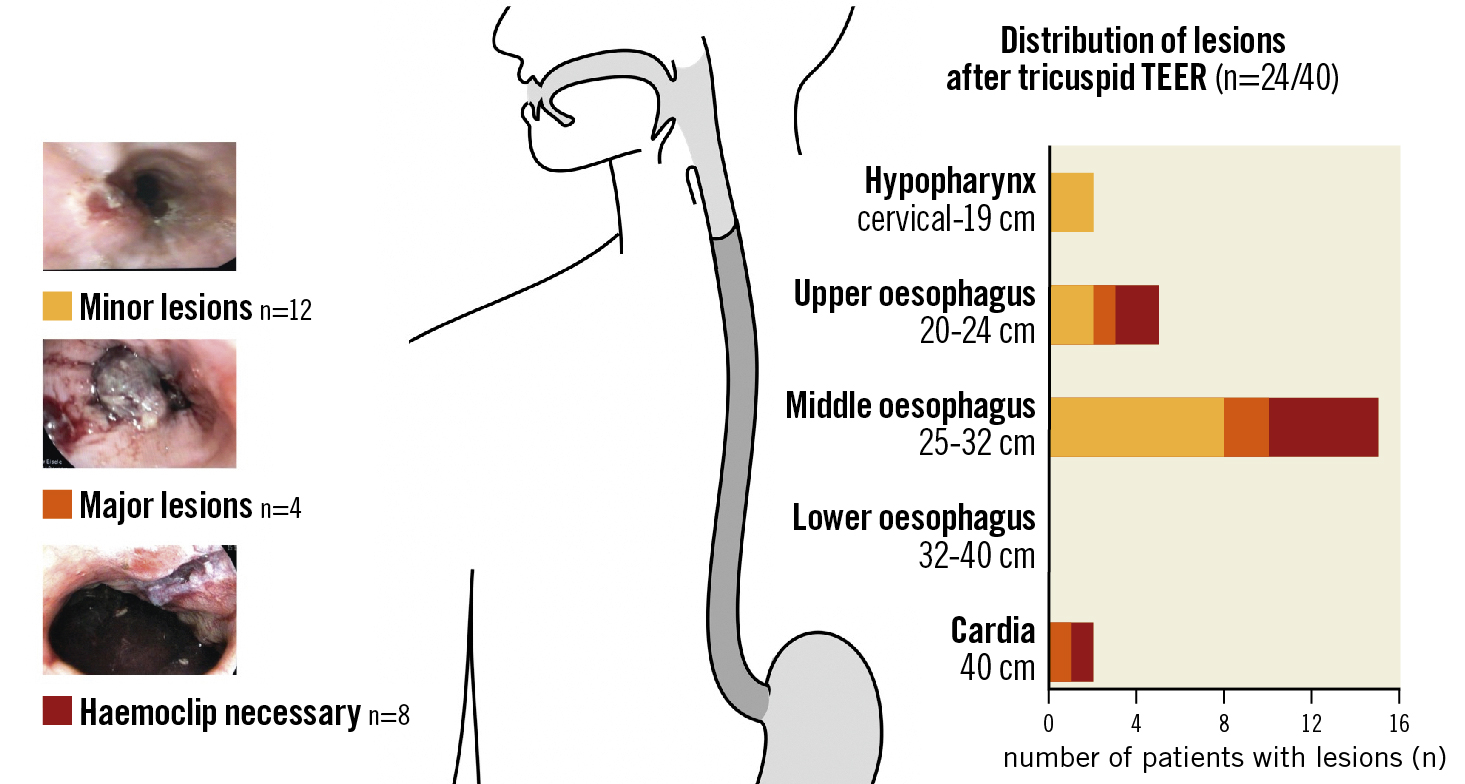
Figure 1. Distribution of injuries caused by the echocardiographic probe manipulation during tricuspid transcatheter edge-to-edge repair (TEER) (n=24).
Funding
This study was funded by the Brandenburg Medical School (MHB) publication fund supported by DFG.
Conflict of interest statement
The authors have no conflicts of interest to declare.