Transcatheter heart valve (THV) intervention has been shown to be successful in the treatment of mitral stenosis, aortic stenosis and mitral regurgitation. The interest of the medical community is now moving towards tricuspid regurgitation (TR) which is an important clinical problem despite it having been considered as “the forgotten valve” for a long time. However, when attempting to fix it we face many challenges (Figure 1).
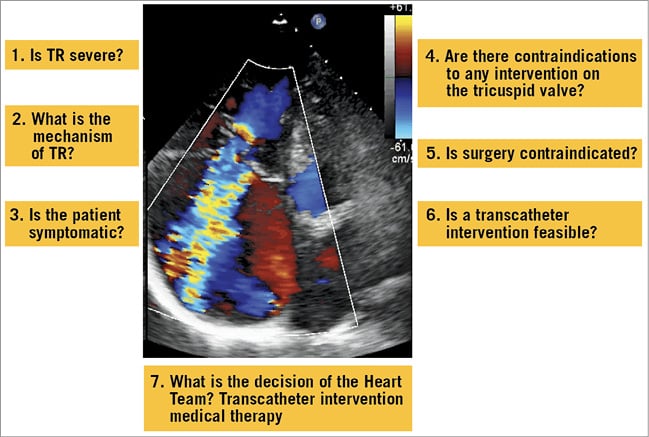
Figure 1. Main questions in the evaluation of a patient for transcatheter tricuspid intervention. TR: tricuspid regurgitation
Pathophysiology
Understanding the pathophysiology of TR is an essential step where there are still serious gaps. Similarly to mitral regurgitation (MR), it is necessary to separate primary TR, due to organic lesions, and the largely predominant secondary TR, which is the consequence of pulmonary hypertension, mostly due to left-sided lesions, annular dilatation, and right ventricular dysfunction. Secondary TR is caused by the combination of tricuspid annular dilatation and leaflet tethering related to right ventricular (RV) enlargement.
In parallel to what happens concerning secondary MR, it remains to be determined whether secondary TR is only a marker of RV dysfunction or a cause which could be effectively treated. When ventricular dysfunction is “extreme”, it is unlikely that any intervention on the tricuspid valve will change the prognosis. The same is true in cases with severe elevation pulmonary hypertension. In addition, surgical experience shows that a “pop-off” effect leading to poor clinical outcomes may occur after tricuspid intervention in patients with poor RV function.
The entity of secondary TR caused by tricuspid annular dilatation related to chronic atrial fibrillation is largely unexplored.
Finally, the presence of transvalvular pacing leads may contribute to TR by several mechanisms which should be analysed before intervention.
Tricuspid valve anatomy
Tricuspid valve anatomy has some particularities which should be considered. The tricuspid orifice is very large, up to 10 cm², making it challenging to obtain a significant reduction with repair techniques and for the implantation of valve prostheses. It is located more anteriorly than the mitral orifice, which explains why imaging using transoesophageal echocardiography (TOE) is challenging.
The tricuspid annulus is somewhat virtual and less “solid” than the mitral one which may be a concern for annuloplasty techniques. The subvalvular apparatus has a variable anatomy, and numerous chordae arise in the commissural area which may cause device entrapment. Leaflet tissue is fragile and may be at risk when grasping leaflets.
The relatively thin and trabeculated structure of the RV renders the transapical approach risky while the angulation between the orifice of the inferior vena cava and the tricuspid valve may make the transfemoral access and navigation of the devices difficult due to a lack of coaxiality.
Finally, there are important structures in the vicinity of the tricuspid valve, mainly the right coronary artery and the atrioventricular node, which can be injured during intervention.
Imaging TR
Imaging TR is also a challenge. In secondary TR, the complex interactions between the left-sided structures and the RV require a comprehensive work-up before decision making. The goals are the assessment of:
– valve anatomy
– severity of TR/RV function
– the other valves
– pulmonary pressures and resistances
– LV function.
Echocardiography should look not only at valve anatomy separating primary and secondary TR but also at valve tethering which has prognostic value after intervention.
Evaluation of severity relies mostly on echocardiography using an integrative approach combining semi-quantitative and quantitative evaluation (Figure 2). Three-dimensional (3D) echocardiographic methods may improve its accuracy. The grading scale adopted in the recent guidelines has been challenged; additional degrees of severity (“massive and torrential”) were recently proposed based on the observation of “more than severe” TR in candidates for THV intervention. However, the definition of severity goes beyond “hydrodynamics” and is mostly based on prognostic value. Thus, the usefulness of these new grades should be evaluated further before they are adopted.
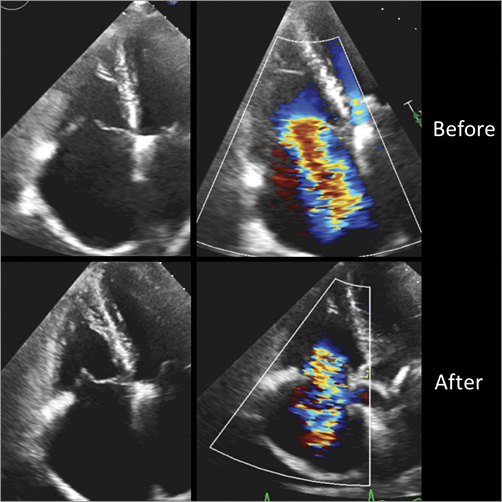
Figure 2. Efficacy of transcatheter tricuspid annuloplasty (Cardioband; Edwards Lifesciences). Transthoracic echocardiography before (top) and after (bottom) transcatheter tricuspid annuloplasty. After transcatheter tricuspid annuloplasty leaflet coaptation is improved (left) and the degree of tricuspid regurgitation decreases on Doppler colour flow (right).
Computed tomography (CT) will play a key role by assessing precisely the characteristics of the tricuspid annulus and the feasibility of specific THV techniques, in particular the relationship with adjacent structures such as the right coronary artery.
The optimal method for evaluating RV function remains unsettled. Here again, 3D imaging is needed and cardiac magnetic resonance (CMR) is considered the reference method.
Right heart catheterisation should be performed when needed to evaluate the pulmonary vascular pressures/resistances because of the caveats of echocardiography in such cases.
Finally, procedural guidance is much more challenging than on the left side. The best multimodality strategy should be evaluated, for example combining TOE and a transthoracic approach or intracardiac echography according to the specific device used.
Need for tricuspid intervention
It is essential to define the clinical need for tricuspid intervention better. There are many patients with severe TR, even if we do not know exactly how many is many! Most estimations are neither current nor based on prospective and comprehensive epidemiologic evaluation. This will require large prospective evaluation including echocardiographic evaluation of severity. A more “solid” illustration of the frequency of TR is the fact that >35% of candidates for mitral surgery have severe TR. In addition, TR is most often associated with left-sided disease and is still too often ignored or underassessed in the clinical work-up of left-sided lesions.
Longitudinal studies consistently show the poor prognosis of severe TR whether it is isolated, functional, or due to flail leaflets. In addition, patients undergoing left-sided valve intervention who also have severe TR have worse clinical outcomes.
Medical therapy alone only transiently improves symptoms but does not change the outcomes.
Surgical experience has provided several lessons which should be kept in mind when considering THV.
Surgical ring annuloplasty, mainly using incomplete rigid rings, is the best way to treat secondary TR, while valve replacement is preferable if there are organic lesions on the valves or excessive annular dilatation. These findings may lead to favouring a combination of annuloplasty combined with leaflet procedures or valve replacement at a late stage of the disease.
Adding a tricuspid repair, if indicated during left-sided surgery, does not increase operative risk. On the other hand, re-operative tricuspid valve surgery after previous left-sided surgery carries a high risk (up to 30% mortality), often due to operations carried out too late. This argues in favour of earlier intervention.
Transcatheter heart valve intervention
THV is in its infancy as only a few hundred patients have been treated using this technique. Besides the early experience with caval valve implantation, the goal of which is only to decrease the peripheral signs of right heart congestion, THV tricuspid experience mostly includes devices acting on the leaflets (MitraClip®; Abbott Vascular, Santa Clara, CA, USA) or on the regurgitant orifice (FORMA tricuspid repair system; Edwards Lifesciences, Irvine, CA, USA) or annuloplasty (Trialign™ [Mitralign, Tewksbury, MA, USA]; Cardioband [Edwards Lifesciences]). The first-in-man for valve implantation was just recently performed. Patients treated were at a very late stage in terms of clinical and anatomical aspects. Today we only have case reports and short series in fewer than 100 cases. The preliminary results suggest that THV is feasible and quite safe. On the other hand, the reduction of the degree of TR is only moderate, something which is to be expected because the patients treated often present with extreme dilatation of the annulus. Functional improvement is observed midterm in the majority of cases.
In parallel to the search for better devices, it is necessary to improve evidence on the results of THV using larger series with longer follow-up and randomised clinical trials (which will start in the near future). Specific endpoints for tricuspid intervention should be defined, taking into account the characteristics of this population where palliation is the main goal. In addition to the criteria used in VARC and MVARC, more attention should probably be paid to functional parameters and the use of drugs.
The indications for interventions were recently updated both in European and in US guidelines. The most recent ESC/EACTS Guidelines state “The potential role of transcatheter tricuspid valve treatment in high-risk patients needs to be determined”!
The indications for tricuspid THV could be expected to be the following with all the necessary reservations at this early stage of development.
In the near future, intervention may only be considered in inoperable/high-risk patients with severe TR. However, the consensus is to avoid intervention too late, something which may well be futile. When TR persists, or recurs after mitral valve surgery or mitral THV, intervention should also be considered early but only when the predominant role of TR is suggested, i.e., when there is no severe pulmonary hypertension, LV or RV dysfunction, or significant residual left-sided valve disease.
Assuming that tricuspid THV proves to be effective and durable, the best indication will be to combine it with THV mitral repair because severe TR will not disappear after treatment of MR. If it is doable, based on experience and economics, THV on TR should ideally be performed during the same session or early after the mitral procedure. Recent short series have suggested that it is feasible with good results.
The key messages here are that in these complex patients the indication for THV should be taken in valve centres of excellence, by a multidisciplinary Heart Team which will make an individualised choice between medical therapy (in patients where any intervention is futile), surgery, intervention, and cardiac transplantation/assistance.
Conclusions
Thus, the awareness of tricuspid disease has improved even if it is still not perfect. If we are successful, tricuspid interventions will no doubt move THV significantly towards the surgical standards.
Conflict of interest statement
A. Vahanian is a consultant to Abbott Vascular, Edwards Lifesciences and Mitraltech.