Abstract
Clinical data have supported the advantages of the double kissing (DK) crush technique, which consists of stenting the side branch (SB), balloon crush, first kissing, stenting the main vessel (MV) and final kissing balloon inflation, for complex coronary bifurcation lesions compared to other stenting techniques. Careful rewiring from the proximal cell of the MV stent to make sure the wire is in the true lumen of the SB stent is key to acquiring optimal angiographic results. Balloon anchoring from the MV, alternative inflation and each kissing inflation using large enough non-compliant balloons at high pressure, and the proximal optimisation technique are mandatory to improve both angiographic and clinical outcomes. Stratification of a given bifurcation lesion is recommended before decision making.
Life is long, but the key is only a few steps at the intersection.
Qing Liu (Chinese poet)
Drawbacks of the classic crush technique
Crush stenting, a modified T-stenting technique, was introduced by Colombo and his colleagues in 20041, with the aim of fully covering the ostial side branch (SB). Originally, the crush stenting technique consisted of stenting the SB, stenting the main vessel (MV) and final kissing balloon inflation (FKBI). One of the advantages of crush stenting is that the SB is never lost, which is a main concern when stenting complex bifurcation lesions. However, several limitations of this technique were recognised in clinical practice: 1) a 7 Fr guiding catheter was required for two stents simultaneously positioned in both the MV and the SB, 2) impossible crossover from provisional stenting to crush stenting. As a result, there are some alternatives to the crush stenting technique, including balloon crush, and inner crush. Balloon crush requires the simultaneous advancement of one balloon in the MV and one stent in the SB. Thus, a 6 Fr guiding catheter is sufficient to accommodate the two devices. Moreover, the first crush is performed immediately after stenting the SB. Inner crush is, in fact, a rescue crush similar to rescue (or provisional) T-stenting. When there are anatomical requirements after stenting the MV, including a severely pinched SB, dissection or even acute closure of the SB, rescue stenting (provisional T or inner crush) for the SB is recommended. Inner crush has a relatively long protrusion of the SB stent into the MV compared to rescue T. In order to minimise the negative impact of a long protrusion into the MV, a balloon crush in the MV is necessary, followed by a FKBI. Of note, the protruded SB stent struts are easily malapposed2, even after FKBI. Indeed, all these crush stenting techniques have been renamed classic crush stenting.
Key points of the double kissing crush technique
A number of studies have reported that classic crush stenting, in particular when FKBI was unsuccessful was associated with a high rate of stent thrombosis (ST) and in-stent restenosis (ISR), most commonly seen at the ostial SB3. Although the rate of FKBI failure was around 20%~25% after classic crush stenting4, the underlying reasons still remained unclear. A bench test has shown that stent platform, irregular and small stent cells, severe distortion of the MV stent, and the presence of three layers of stent struts irregularly overlapping are potential factors affecting the successful rate of FKBI5. To overcome these disadvantages of classic crush, the double kissing and the double kissing (DK) crush stenting techniques (Figure 1) were introduced by our group in 20056. DK crush introduces kissing twice and includes the following steps: stenting the SB (with 1-2 mm protrusion), balloon crush, first kissing, stenting the MV, and FKBI. The main difference between classic and DK crush is the use of first kissing. After balloon crush of the implanted SB stent, there are two layers of stent struts from the ostial SB to the MV. Thus, first kissing can optimise the distorted SB stent and leave only one layer of metal struts at the ostial SB, which probably facilitates the second kissing after stenting the MV. Another advantage of DK crush over classic crush is that the first kissing balloon inflation minimises repeated distortion of the ostial SB stent when inflating the MV stent. In other words, first kissing rebuilds the shape of the bifurcation anatomy.
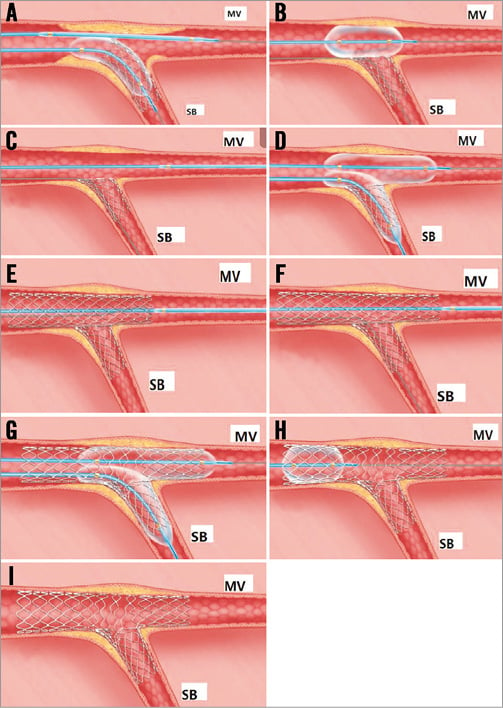
Figure 1. Schematic diagram presenting the DK crush stenting technique step by step. A) One balloon was introduced into the MV and the SB stent. B) & C) The balloon in the MV was then inflated to crush the SB stent after its deployment. D) After rewiring the SB proximally, a first kissing was performed. E) Stenting the MV. F) & G) Final kissing balloon inflation was conducted after rewiring the SB from the proximal MV stent cell. H) & I) After stenting both the MV and the SB, the proximal optimisation technique (POT) should be performed to improve MV stent strut apposition. DK: double kissing; MV: main vessel; SB: side branch
However, some caution is noteworthy. As we found from the bench test for classic crush, rewiring the SB is necessary to repair the distorted SB stent5. Operators always need to pay more attention to rewiring the SB from the proximal MV stent cell. Rewiring the SB from the distal MV stent cell could increase the possibility of the wire going between the stent and the vessel wall, which will leave a gap at the ostium after balloon crushing (Figure 2)5. The methods to confirm the exact position of the SB wire are as follows: visual assessment from fluoroscopy (orthogonal projections to confirm SB rewiring from the proximal MV stent cell, Moving image 1-Moving image 15), guidance with intravascular ultrasound (IVUS) or optical coherence tomography (OCT) from the MV. Sometimes, it is difficult to advance the balloon to the SB after positioning the wire in the true lumen of the SB stent. One alternative is to inflate a balloon in the distal MV to provide extra support (namely, balloon anchoring technique). Otherwise, a minimal size balloon (such as 1.25 mm) can be tried, followed by a relatively large one. Alternative inflation using a non-compliant balloon (with a balloon/stent ratio of 1:1) at ≥16 atm starting from the SB is recommended before first kissing and FKBI. Two non-compliant balloons are usually inflated at ≥12 atm during FKBI7. The proximal optimisation technique (POT) is mandated to achieve good apposition of the proximal MV stent unless IVUS or OCT confirms no stent strut malapposition at the proximal MB. A flow-limiting dissection at the proximal or distal edge of the MV, or the distal edge of the SB entails a bail-out stent.
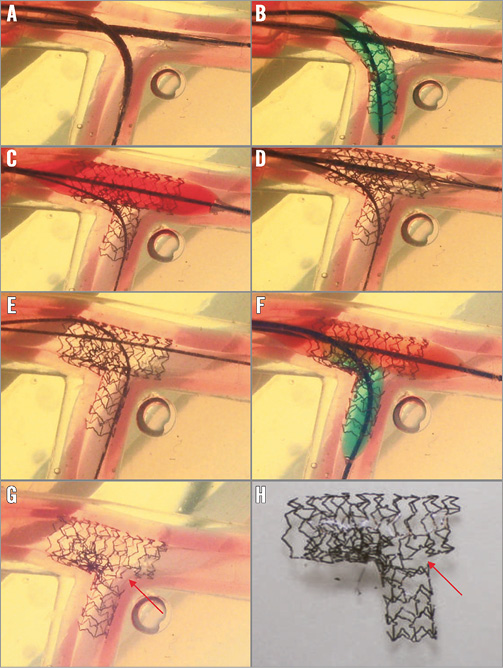
Figure 2. Drawback of too distal SB re-crossing in the classic crush technique. A) Position of MV and SB stents. B) SB stent deployment. C) MV stent deployment to crush the SB stent. D) Gap formation near the carina. E) Distal SB re-crossing, wire going between the SB stent and vessel wall. F) Final kissing balloon inflation. G) & H) Leaving a significant gap near the carina. MV: main vessel; SB: side branch.
Data from the DKCRUSH trials
Clinical data, comparing the DK crush with either classic crush or other stenting techniques, originate mainly from the serial randomised DKCRUSH trials. Initially, we reported that FKBI was successfully performed in 100% of cases by DK crush2, compared to 80% in the classic crush. In the DKCRUSH-I study, we demonstrated that DK crush was associated with a significant reduction of ST, ISR and major adverse cardiac events (MACE) in treating patients with true bifurcation lesions compared to the classic crush8. Interestingly, the DKCRUSH-II trial7 for the first time showed a significantly low rate of target lesion revascularisation (TLR) after DK crush for complex bifurcation lesions at one-year follow-up, compared to the provisional T-stenting technique. Recently, the DKCRUSH-III study, including patients with distal left main bifurcation lesions, showed that one-year clinical outcomes and 13-month angiographic results were in favour of DK crush when compared with the culotte stenting technique9. Furthermore, IVUS analysis confirmed better strut apposition in the DK crush stenting group10. In addition, clinical results from the studies also supported the superiority of DK crush compared to other stenting techniques for left main bifurcation lesions at long-term follow-up8,11. When analysing the DKCRUSH trials, it is too early to conclude that DK crush is the best “mousetrap” for stenting bifurcation lesions. Actually, whether DK crush can achieve favourable outcomes in patients with more frequent morbidities (myocardial infarction, left ventricular dysfunction), longer SB lesion length and more complex lesions (chronic total occlusion, calcified and thrombus-containing lesions) has not yet been defined. Furthermore, no two bifurcation lesions are identical and, while it may sound superficial, one needs to take note of the fact that all true bifurcation lesions belong to complex lesions. According to our DEFINITION study12 which relied on anatomical variables from 3,660 patients with Medina 1,1,1 and 0,1,1 bifurcations and a minimum SB diameter of 2.5 mm, complex bifurcation lesions amount to only 30% among all true bifurcation lesions, with 70% being classified as simple bifurcation lesions. All two-stent techniques did not show any benefits over a one-stent approach in simple bifurcation lesions. In contrast, two-stent techniques for complex bifurcation lesions were associated with less in-hospital mortality and one-year MACE than the one-stent technique.Therefore, before making a final decision on stenting technique selection, lesion stratification is recommended. The superiority of DK crush over provisional stenting or other complex stenting techniques for the newly defined complex lesion needs to be tested in future randomised studies.
Summary
In summary, the available clinical data support the advantages of DK crush over other stenting techniques for more complex coronary bifurcation lesions. This technique consists of stenting the SB, balloon crush, first kissing, stenting the MV, and FKBI. Careful rewiring from the proximal cell of the MV stent and maintaining the wire in the true lumen of the SB stent are critical for optimal angiographic results at follow-up. Balloon anchoring from the MV, alternative inflation and each kissing inflation using large enough non-compliant balloons at high pressure, and the POT technique are mandatory to improve both angiographic and clinical outcomes. Imaging modalities are useful to guide SB rewiring and assessment of procedure quality. Stratification of a given bifurcation lesion is recommended before decision making.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Online data supplement
Moving image 1. Baseline CAG1.
Moving image 2. Baseline CAG2.
Moving image 3. SB stent deployment.
Moving image 4. 3.5 mm balloon in MV inflation to crush SB stent.
Moving image 5. 4.0 mm balloon in MV inflation to crush SB stent.
Moving image 6. Rewiring the SB from the proximal cell.
Moving image 7. First kissing balloon inflation.
Moving image 8. MV stent deployment to crush the SB stent.
Moving image 9. POT with a 4.0 mm balloon.
Moving image 10. SB balloon inflation at 20 atm.
Moving image 11. Final kissing balloon inflation.
Moving image 12. Final result 1.
Moving image 13. Final result 2.
Moving image 14. 1-year angiographic FU 1.
Moving image 15. 1-year angiographic FU 2.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 8. MV stent deployment to crush the SB stent.
Moving image 9. POT with a 4.0 mm balloon.
Moving image 10. SB balloon inflation at 20 atm.
Moving image 11. Final kissing balloon inflation.
Moving image 12. Final result 1.
Moving image 13. Final result 2.
Moving image 14. 1-year angiographic FU 1.
Moving image 15. 1-year angiographic FU 2.
Moving image 1. Baseline CAG1.
Moving image 2. Baseline CAG2.
Moving image 3. SB stent deployment.
Moving image 4. 3.5 mm balloon in MV inflation to crush SB stent.
Moving image 5. 4.0 mm balloon in MV inflation to crush SB stent.
Moving image 6. Rewiring the SB from the proximal cell.
Moving image 7. First kissing balloon inflation.

