Abstract
Aims: Lesion length remains a predictor of target lesion revascularisation and results of long lesion stenting remain poor. Sirolimus-eluting stents have been shown to perform better than paclitaxel eluting stents in long lesions. In this substudy of the LEADERS trial, we compared the performance of biolimus biodegradable polymer (BES) and sirolimus permanent polymer stents (SES) in long lesions.
Methods and results: A total of 1,707 ‘all-comer’ patients were randomly allocated to treatment with BES and SES. A stratified analysis of angiographic and clinical outcomes at nine months and one year, respectively was performed for vessels with lesion length <20 mm versus >20 mm (as measured by quantitative angiography).
Of 1,707 patients, 592 BES patients with 831 lesions and 619 SES patients with 876 lesions had only short lesions treated. One hundred and fifty-three BES patients with 166 lesions and 151 SES patients with 162 lesions had long lesions. There were no significant differences in baseline clinical characteristics, except for higher number of patients with long lesions presenting with acute myocardial infarction in both stent groups. Long lesions tended to have lower MLD and greater percent diameter stenosis at baseline than short lesions. Late loss was greater for long lesions than short lesions. There was no statistically significant difference in late loss between BES and SES stents (0.32±0.69 vs 0.24±0.57, p=0.59). Binary in-segment restenosis was present in 23.2% versus 13.1% of long lesions treated with BES and SES, respectively (p=0.042). In patients with long lesions, the overall MACE rate was similar for BES and SES (17% vs 14.6%; p=0.62). There was a trend towards higher overall TLR rate with BES (12.4 % vs 6.0%; HR=2.06; p=0.07) and clinically driven TLR (10.5% vs 5.3%: HR 1.94; p=0.13). Rates of definite stent thrombosis were 3.3% in the long lesion group and 1.3-1.7 % in the short lesion group.
Conclusions: BES and SES appear similar with respect to MACE in long lesions in this “all-comer” patient population. However, long lesions tended to have a higher rate of binary in-segment restenosis and TLR following BES than SES treatment.
Introduction
Drug eluting stents have considerably reduced restenosis and the need of repeat revascularisation compared to bare metal stents.1,2 The ADVANCE study was the first to demonstrate that stenting in long lesions (> 40 mm) was associated with higher MACE rates.3 Sirolimus eluting stents (SES) have been shown to yield superior results to paclitaxel eluting stents in most, but not all studies,1,4,5 particularly in complex lesions and patient populations.6,7 Patients with long lesions remain at increased risk for impaired long-term clinical outcome mainly related to repeat revascularisation procedures. In a study of 500 patients with long lesions, SES showed superior angiographic outcome in terms of late loss (0.09 vs 0.45 mm; p<0.001), percent diameter stenosis and binary restenosis (3.3% vs 14.6%; RR=0.23; p<0.001), as well as TLR rates (2.4% vs 7.2%; p=0.012) but not overall MACE rates.5
Biolimus is a highly lipophilic sirolimus analogue.8 It inhibits the mammalian target of rapamycin (mTOR) and cell-cycle transition in smooth muscle cells with similar potency to sirolimus. In the LEADERS multicentre randomised study of biolimus-eluting biodegradable polymer stent (BES) versus sirolimus-eluting permanent polymer stent (SES), we noted that late loss in the overall patient population was similar for BES than SES (0.13 versus 0.19 mm; p=0.34 at 9 months).9 In the present stratified analysis of lesion length, we investigated the outcome of patients with short and long lesions following treatment with BES and SES. We hypothesised that since late loss and TLR rates were non-inferior for the BES in the overall population in LEADERS, that this stent will also perform equivalently to SES in the long lesion subset.
Methods
Study population
LEADERS was a multicentre European non-inferiority trial comparing safety and efficacy of BES to SES in 1,707 ‘all comer’ patients. Patients over the age of 18 with chronic stable coronary artery disease or acute coronary syndromes including ST-elevation myocardial infarction were eligible if they had at least one lesion with > 50% diameter stenosis and reference vessel diameter 2.25 to 3.5 mm. The aim was for the patient population to reflect real clinical practice, and thus no limits were set on the number or complexity of the lesions stented. The only exclusion criteria were: known allergy to acetylsalicylic acid, clopidogrel, heparin, stainless steel, sirolimus, biolimus or contrast material that cannot be pre-medicated, planned surgery within six months of percutaneous coronary intervention – unless the dual anti-platelet therapy could be maintained throughout the peri-surgical period, pregnancy or participation in another trial before reaching the primary end-point and lastly, inability to give informed consent. The study complied with the Declaration of Helsinki and was approved by all institutional ethics committees. All patients provided written, informed consent for participation in the trial.
Randomisation and procedures
Randomisation was done centrally after diagnostic cardiac catheterisation and before PCI by use of a telephone allocation service (Limburgia Telefonische Antwoord Service BV, 3068 NP Rotterdam, The Netherlands). The allocation sequence was computer generated, stratified according to centre, and blocked with block sizes of eight and 16 which varied randomly. Randomisation was performed on a 1:1 basis to treatment with a stent eluting biolimus-A9 with a biodegradable polylactic acid polymer (Biomatrix Flex, Biosensors Inc., Newport Beach, CA, USA) (Figures 1a, b and c) or a sirolimus-eluting stent with a durable polymer (Cypher SELECT, Cordis, Miami Lakes, FL, USA) and to active angiographic follow-up at nine months, or clinical follow-up only on a 1:3 basis with a factorial design.


Figure 1. A9™ Eluting Stent: Structure of biolimus and scanning electron micrograph of the biolimus biodegradable polymer stent. 1a. Biolimus is a semi-synthetic sirolimus with 10x higher lipophilicity and similar potency as sirolimus. 1b. Biolimus is immersed at a concentration of 15.6 µg/mm into a biodegradable polymer, polylactic acid and applied solely to the abluminal stent surface by a fully automated process. Polylactic acid is co-released with biolimus and completely dissolves into carbon dioxide and water during a 6-9 months period. 1c. The stainless steel stent platform has a strut thickness of 112 µm with a quadrature link design.
BES were available in diameters of 2.25, 2.5, 3.0 and 3.5 mm and in lengths of 8, 11, 14, 18, 24 and 28 mm. SES were available in diameters of 2.25, 2.5, 2.75, 3.0 and 3.5 mm and in lengths of 8, 13, 18, 23, 28 and 33 mm. Balloon angioplasty and stent implantation was performed according to standard technique and direct stenting was allowed. No mixture of drug eluting stents was allowed within a given patient, unless the operator was unable to insert the study stent, in which case crossover to another device of the operator’s choice was permitted. The length of the stent was left at the discretion of the operators who followed good clinical practice guidelines which include using one stent to cover the lesion when possible. Before, or at the time of the procedure, patients were given at least 75 mg of acetylsalicylic acid, 300-600 mg loading dose of clopidogrel and unfractionated heparin in a dose at least 5,000 IU or 70-100 IU/kg. After the procedure, all patients were advised to take aspirin indefinitely and clopidogrel for at least 12 months. In case of inter-current revascularisation procedures needing stent implantation, treating cardiologists were encouraged to use the study stent. For other details please see the main manuscript.9
Study endpoints
Adverse events were assessed in the hospital and at nine and 12 months. An independent clinical events committee unaware of the patient’s treatment assignments adjudicated all endpoints. One in four patients was asked to return for angiographic follow-up at nine months. Definitions of all endpoints are explained in the main manuscript.9 Briefly, the pre-specified primary endpoint was the composite of cardiac death, myocardial infarction and clinically-indicated target vessel revascularisation (TVR) within nine and 12 months. Secondary endpoints were: any target lesion revascularisation (TLR) – both clinically and non-clinically indicated – which we defined as repeat revascularisation due to a stenosis within the stent or within a 5 mm border proximal or distal to the stent; any TVR, cardiac death, death from any cause, myocardial infarction, stent thrombosis (defined according to the ARC)10, device success (defined as achievement of a final residual diameter stenosis of less than 50% during the initial procedure), and lesion success (achievement of less than 50% stenosis with any approach for PCI).
The pre-specified principal outcome for angiographic substudy was in-stent percentage diameter stenosis. Secondary angiographic outcomes were: in-segment percentage diameter stenosis, minimal lumen diameter, late lumen loss and binary restenosis. We obtained angiographic measurements within the stented segment (in-stent) and over the entire segment consisting of the stent and 5 mm proximal and distal margins (in-segment). We defined percentage diameter stenosis as ([reference vessel diameter-minimal luminal diameter]/reference vessel diameter) X 100%; late lumen loss as the difference between minimal lumen diameter after the procedure and minimal lumen diameter at follow-up; and binary restenosis as percentage diameter stenosis of 50% or greater in the target lesion.
Independent study monitors (D-Target, Montagny-pres-Yverdon, Switzerland) verified all case reports from data on-site. Data were stored in a database (KIKA Medical, Paris, France), which was maintained by a contract research organisation (Cardialysis, Rotterdam, The Netherlands) in collaboration with an academic clinical trials unit (CTU Bern, Bern University Hospital, Bern, Switzerland). Clinical follow up was done at 1, 6, 9 and 12 months. The operators were, by necessity, aware of the assigned study stent during PCI and angiographic follow-up, but patients and staff involved in follow-up assessment were blinded to the allocated stent type. Angiographies were centrally assessed at one angiographic core laboratory (Cardialysis, Rotterdam, The Netherlands) with assessors unaware of the allocated stent.
Statistical analysis
A stratified analysis of clinical and angiographic outcomes, which was specified after completion of patient recruitment, was performed according to lesion length. Methodology similar to the previously published SIRTAX trial was used.11 Patients, who underwent stent implantation in lesions with an lesion length ≤20 mm (as measured by quantitative angiography at index procedure), were categorised as having undergone treatment of short lesion. Conversely, patients who underwent stent implantation in lesions with length >20 mm were classified as having had treatment of long lesion. Patients with stent implantations in both short and long lesions were classified as mixed. All randomised patients were included in the analysis of primary and secondary clinical endpoints in the groups that they were originally assigned (intention-to-treat analysis). Analyses of the angiographic substudy were restricted to lesions from patients who attended follow-up angiography. Angiographic outcomes were analysed using SAS v8 Proc Mixed for continuous, and Proc Genmod for binominal outcomes, taking into account the within-patient correlation structure of these data. We used a Cox proportional hazards model to compare clinical outcomes between the groups. All analyses were performed using SAS 8.02 by a dedicated statistician. All p-values and CIs were two-sided.
Results
Baseline clinical, angiographic, and procedural data
Of 1,707 patients, 592 patients in the BES group with 832 lesions and 619 patients in the SES group with 876 lesions had only short lesions treated. One hundred and fifty-three patients in the BES group with 166 lesions and 151 patients with 162 lesions in the SES group had long lesions. (Figure 2) 105 patients with 250 lesions in the biolimus group and 69 patients with 164 lesions in the sirolimus group had both short and long lesions.
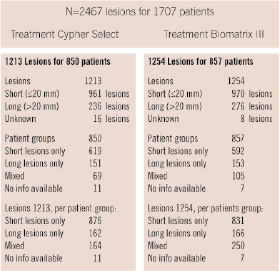
Figure 2. Flow chart.
Baseline clinical and angiographic characteristics are summarised in Table 1.
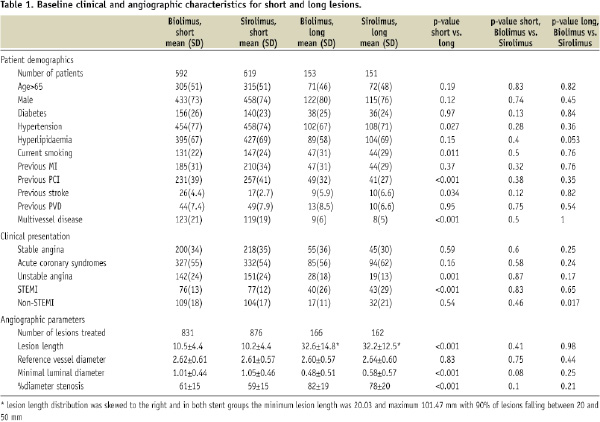
More patients with long lesions tended to present with ST-elevation MI (26-29% vs 12%) in both stent groups. Patients with long lesions treated with BES tended to have less hypertension (67% vs 77% for short lesions, p=0.027). Patients with long lesions treated with either stent had a greater number of current smokers (29%-31% vs 22%-24%; p=0.011). Patients with short lesions tended to have been previously treated with percutaneous revascularisation more often, had more strokes and more multivessel disease.
Mean lesion length for short lesions was 10.5±4.4 mm in the BES group and 10.2±4.4 mm in the SES group. Long lesions measured on average 32.6±14.8 mm in the BES group and 32.2±12.5 mm in the SES group. (Table 1) The distribution for long lesions was skewed to the right with minimum lesion length of 20.03 mm and maximum lesion length of 101.47 mm, 90% of the long lesions were 20-50 mm. Reference vessel diameters did not differ significantly between lesion or stent types. Long lesions tended to have much lower MLD (0.48-0.58 mm vs 1.01-1.05 mm) than short lesions and correspondingly greater percent diameter stenosis (78-82% vs 59-61%; p<0.001). The lower MLD in the long lesion group was significantly correlated with acute myocardial infarction at presentation (data not shown).
Procedural characteristics and results
Procedural results are shown in Table 2.
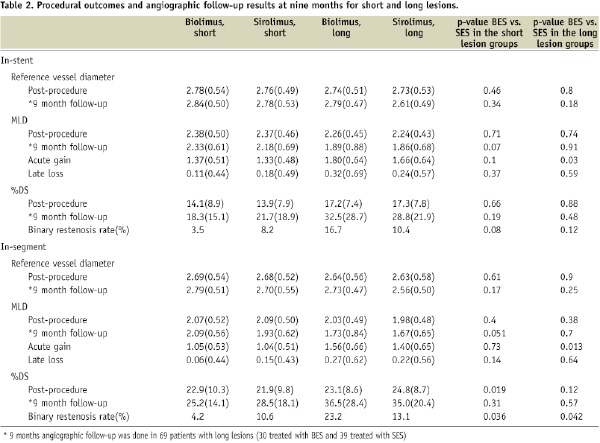
Average numbers of stents per lesion were 1.14-1.15 in the short lesions and 1.99-2.0 in the long lesions. Mean stent diameters per lesion were similar between lesion types and groups. Total stent length per lesion was 20±9 mm in the short lesions and 43±22 mm in the long lesions.
Percent diameter stenosis was 14.1±8.9% and 13.9±7.9% in the short lesions treated with BES and SES, respectively, 17.2±7.4% in the long lesions treated with BES and 17.3±7.8% in the long lesions treated with SES. The differences were not statistically significant. Long lesions had significantly greater absolute gain as the lesions treated had lower initial MLDs (p=0.05). This effect was consistent across stent groups.
Angiographic results
Angiographic follow-up at nine months was obtained in 313 short lesions and 69 long lesions. There was no statistically significant difference in late loss, minimal luminal diameter, percent diameter stenosis or binary restenosis in small or large vessels between BES and SES groups, although this could have been due to the relatively low number of lesions, particularly in the long lesion subgroup (Table 2). Late loss increased more with lesion length in the case of BES stents that in the case of SES stents (Figure 4).
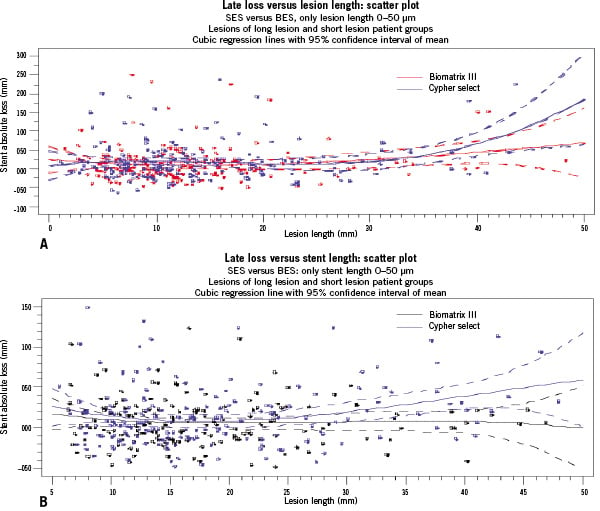
Figure 4. Late loss versus, A) lesion length and B) stent length for BES versus SES.
Corresponding MLDs and percent diameter stenoses were not significantly different (Table 2). Binary in-stent restenosis was present in 3.5% versus 8.2% of short lesions treated with BES and SES respectively, and in 16.7% versus 10.3% of long lesions treated with BES and SES (p=0.12). A similar pattern was observed for in-segment restenosis (23.2% vs 13.1% for long lesions; p=0.042). The proportion of patients and lesions treated with overlapping stents in long lesions did not differ between BES and SES.
Clinical outcomes
Clinical events at one year follow-up, stratified by lesion length, are listed in Table 3 and summarised in Figures 3a and 3b as Kaplan Meier curves.
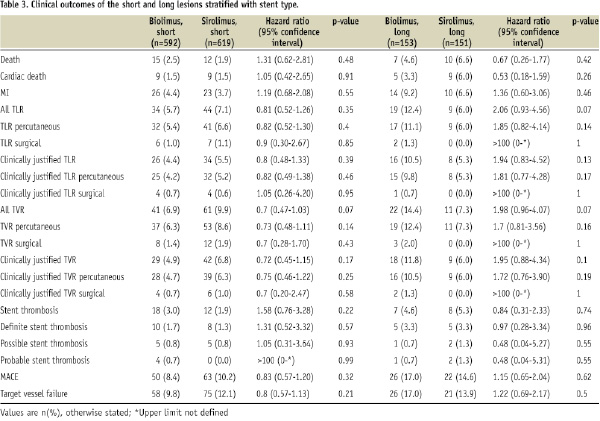
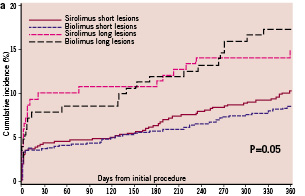
Figure 3a. Kaplan Meier curves for MACE rate at one year follow-up.
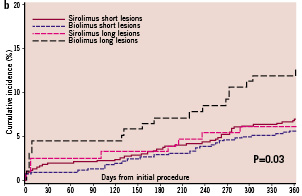
3b. Kaplan Meier curves for TLR rates at one year follow-up.
There were no significant differences in the rate of MACE through stent groups or lesion types. The overall rates of MACE were: 8.4% versus 10.2% in the short lesions treated with BES and SES, respectively (p=0.32). In patients with long lesions, MACE rate was 17% vs 14.6% in the BES and SES groups (p=0.62).
TVR rates were 6.9% versus 9.9% in the short lesions in favour of BES (p=0.07), 14.4% versus 7.3% in the long lesions in favour of SES (HR=1.98; p=0.07). TLR rates shown in Kaplan Meier curves demonstrated similar pattern of SES tending to perform better in long lesions. In addition, TLR increased proportionally to the stent length (divided by tertiles). For stent length of less than 12.9 mm, TLR rate was 4.1%, for stent length 12.9-19.5 mm 5.6% and for stent length >19.5 mm, TLR was 7.4% (p=0.0334).
The rates of definite stent thrombosis in the long lesion group were 3.3% in the long lesion group versus 1.3-1.7% in the short lesion group. For the long lesions group total stent thrombosis rates were 0.7% for acute, 3.0% for subacute and 1.3% for late stent thrombosis (at one year). These rates were comparable for short lesions in acute and late stent thrombosis rates. The rate of sub-acute stent thrombosis for short lesions was 0.8% (versus 3.0% for long lesions).
Discussion
We present here a novel stent technology now commercially available in Europe, which combines the biodegradable polymer technology with solely abluminal elution of biolimus. Use of drug eluting stents has improved outcomes in patients with coronary artery disease treated with PCI,12 including complex lesions.13,14 However, lesion length has remained a strong predictor of in-stent restenosis.15,16 Although the pattern of restenosis after drug eluting stents is more focal rather than diffuse, as with bare metal stents, and therefore more easily treated, it still remains increased for long lesions.5,7 Paclitaxel eluting stents have been shown to be inferior to sirolimus eluting stents with TVR rates of 7.6% versus 3.2% (p=0.03) in recent studies involving long lesions.5 Our study is the first to compare the performance of a biolimus biodegradable polymer stent (BES) with a sirolimus permanent polymer stent (SES) in long lesions. The population studied was an ‘all comers’ population within the LEADERS trial, with a considerable number of high risk lesions, average lesion length in the long lesion group of 32 mm and high proportion of ST elevation myocardial infarctions (28% in the long lesion group). The TVR rate in the long lesions was 14.4% in the BES group and 7.3% in the SES group with a hazard ratio of 1.98 and a trend towards statistical significance. This is compared to 6.9% and 9.9% TVR rates in short lesions, in BES and SES groups respectively. Therefore, SES tended to perform better than BES in long lesions, although the result did not reach statistical significance. Interestingly, in patients with multivessel disease and mixed lesions, the reverse was observed with statistically significant difference in favour of BES (2.9% versus 14.5%, HR=0.18; p<0.001; data not shown). This latter effect did not appear to be explainable by the interaction of stent type with patient diabetic status. In addition, it paralleled the results (presented elsewhere) of stenting by reference vessel diameter, where patients with mixed, small and large diameter reference vessel lesions derived benefit from stenting with BES.
No differences were observed between BES and SES in the rate of MACE, or rate of stent thrombosis in the long lesions although the incidence was rather high in this subgroup.
The angiographic follow-up was limited to one quarter of the patients, and although corresponding differences in late loss and percent diameter stenosis were found between BES and SES stented lesions in the long lesion group, given low patient and lesion numbers the results did not reach statistical significance. Further validation of the results will be needed in larger registries of equally complex patients.
Limitations
This substudy is limited by post hoc nature of the analysis, and limited number of long-lesions with angiographic follow-up. The study may be under-powered to detect differences in the angiographic outcomes. Longer term follow-up will be necessary to fully assess the performance of biolimus stent, especially with respect to stent thrombosis, since polymer fully degrades at six months.
Conclusions
Biolimus and sirolimus eluting stents appear equivalent with respect to MACE rate in long lesions in this “all-comer” patient population, however, biolimus treated long-lesion group appears to have higher TLR rates. There were no statistically significant differences in the late loss, percent diameter stenosis or binary restenosis rates for short of long lesions treated with either stent, although the study may have been underpowered to detect these differences in angiographic outcomes.
Acknowledgements
We would like to thank Dr. Pedro Eerdmans, MD, PhD for his assistance with manuscript preparation and data analysis.