How best to treat intermediate coronary stenoses remains a dilemma for interventional cardiologists. The value of treating coronary stenosis by visual anatomical assessment alone in all but the most significant lesions, or in those with unstable coronary syndromes, is increasingly being challenged. The rationale for this is the increasing understanding that percutaneous coronary intervention (PCI) offers limited mortality benefit over and above medical therapy to patients with intermediate coronary disease. Whilst stenting for hard clinical outcomes is in counterpoise between PCI and medical therapy, accurate identification of patients with genuine ischaemia who are likely to gain from a significant reduction in angina following PCI remains crucial. Studies such as ISCHAEMIA1 (International Study of Comparative Health Effectiveness with Medical and Invasive Approaches) and ORBITA2 (Comparison of Coronary Angioplasty and Optimum Medical Therapy Versus Optimal Medical Therapy in the Stable Angina) are underway, both of which will assess this. These studies will help to address the fundamental questions that coronary physiology first set out to answer. For example, is a coronary lesion sufficiently severe to cause angina, and therefore potentially suitable to benefit from PCI? Fractional flow reserve (FFR) has been used increasingly over the past 10-15 years as a method to identify and effectively target the coronary stenoses most likely to benefit from PCI. Recent trials continue to show the value of using invasive physiological assessment to detect intermediate lesions necessitating treatment with PCI (FAME3, FAME 24).
In this issue of EuroIntervention, Papafaklis et al report on a new virtual functional assessment of coronary stenosis, derived from computed flow dynamics (CFD)5. Using models reconstructed from coronary angiographic images, they report on the calculation of a novel CFD-based virtual functional assessment index (vFAI). The vFAI discriminatory power for FFR significant lesions was high (area under the curve [AUC]: 92%), superior to percentage area stenosis derived from 3D QCA (AUC: 78%). These results follow other similar studies6-8, and are interesting not only because of the high discriminatory power with the method presented, tested in a data set of 139 lesions, but also because the results are based on computer-derived pressure drop estimated using relatively simple geometries obtained from 3D QCA.
What is the fundamental limitation in any CFD model of FFR?
Although appealing in principle to reduce cost and improve patient management, non-invasive CFD-based methods have inherent limitations, which should not be overlooked in the context of their applicability for routine practice.
In most virtual FFR methods based on CFD, including the study by Papafaklis et al, the flow used to calculate the FFR is pre-specified and assumed to be equal in all stenoses. However, we know from several studies that there is a large variation in hyperaemic blood flow in patients with CAD9-11. Such oversimplification of baseline flow boundary conditions and hyperaemic response may work on average but can lead to implausible results when applied to individual cases, across a wide spectrum of patient anatomies.
Imaging approaches such as angiography or CT also have limited spatial resolution compared with IVUS or optical coherence tomography (OCT), which is another limitation. QCA and 3D QCA are subject to movement artefacts and can artificially smooth the artery wall. Loss of high resolution vessel geometry can lead to underestimation of lesion severity and erroneous FFR computation12. Recent studies using the gold standard of intravascular lumen imaging OCT combined with patient-specific pressure and velocity phasic data have shown only modest correlation with invasive pressure drop measurements12, which also underlines the importance of flow and pressure boundary conditions for accurate evaluation of pressure drop using CFD.
How to compare virtual physiological assessment with FFR: impact of FFR variability and flow assumption
Non-invasive FFR has been tried with numerous approaches recently, giving ever-improving performance and diagnostic accuracy. The most highly tested uses the HeartFlow system (HeartFlow, Inc., Redwood City, CA, USA). A close examination of the three studies using the HeartFlow system shows a range of diagnostic accuracy among the studies. The Discover-Flow study found a good classification match and correlation (r=0.68)7, which could not be replicated in the DEFACTO study13 (r=0.63), and it was only in the recent HeartFlow NXT study14 that diagnostic agreement improved significantly (r=0.82). Whilst small differences in the CFD protocols and the administration of nitrates may have accounted for some of these differences, another explanation for the different results may lie in the distribution of lesion severities in each study. The agreement between virtual models of FFR and invasive FFR will vary according to the sample. If extremes of disease severity are included, agreement will be high. If more intermediate values predominate, agreement will be lower. This dependency of the test accuracy on the underlying sample is an underappreciated phenomenon not restricted to CFD models of FFR. Importantly, it also affects FFR reproducibility agreement, a ceiling upon which other tests cannot improve.
A mathematical analysis by Petraco et al15 based on DEFER16 revealed that FFR repeatability classification changed around 20% of the time when a single FFR result fell within 0.03 units around the cut point (0.77-0.83). This means that, in a clinical sample (formed predominantly by intermediate stenoses), in around 15% of stenoses FFR classification will change, moving from significant to non-significant and vice versa, if measured 10 minutes later15. Almost all of these cases in which classification changed lay very close to the FFR cut point. This means that if your first FFR is 0.6 the chance of the FFR becoming negative if measured again is very low, whereas if the first FFR is 0.79 the chance of the repeat FFR being >0.80 is high (Figure 1).
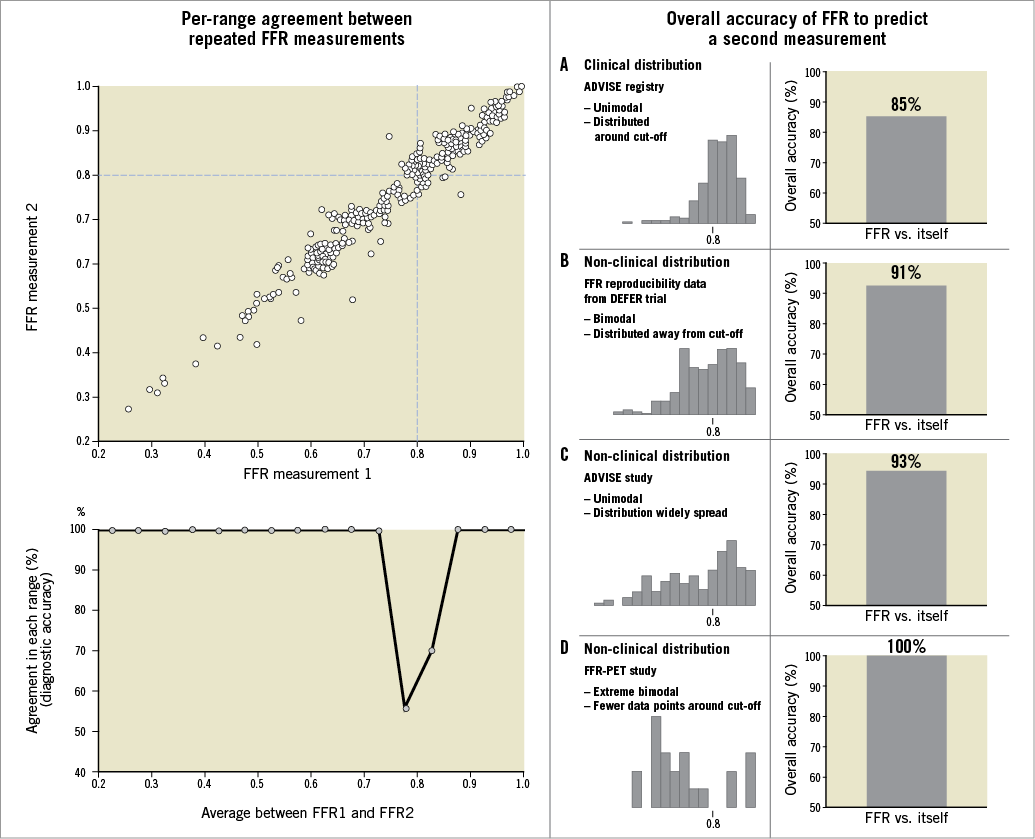
Figure 1. Per-range agreement between repeated measurements of FFR. Top left panel is a scatter plot of two repeated FFR measurements, taken 10 minutes apart. Bottom left panel reveals the level of agreement (“diagnostic accuracy”) between the two measurements for each quintile of disease (from 0.2 to 1 in bands of 0.05). Agreement between FFR values was considered when both FFR values were below (or equal) or above the established cut-off of 0.8014. Right panel: intrinsic agreement of repeated FFR measurements derived for different types of data distribution (histograms). Adapted with permission from Petraco et al15. This figure demonstrates how agreement between tests is largely affected by the sample distribution.
So why does this matter? Is this just an academic exercise in statistics, or is it of real relevance to the data in this field, and how is it relevant to this study by Papafaklis et al? By using distributions with very severe and very mild stenoses which are far away from the FFR cut point, it is possible to attain very high levels for diagnostic accuracy. However, in truly intermediate populations, where measures are close to the cut point, diagnostic accuracy will inherently be worse (even against a repeat measure of FFR). One approach to solve this problem is to display the agreement between tests in each range of FFR values15.
So should we go with the flow?
Systematic use of FFR can be difficult to implement, and in practice clinical decisions during interventions are still most often based on direct visual estimation of coronary stenosis by angiography. However, with intermediate stenosis in the range between 40 and 70% stenosis, we know that CTA or angiography diagnostic accuracy of a physiologically significant lesion is poor. Yet, despite the evidence and apparent clear clinical justification for the use of FFR, adoption remains pitifully low. This has led several groups to propose alternative invasive and non-invasive approaches to assess flow-limiting stenosis such as iFR10, BSR17, as well as entirely computer-simulated indices6,12,14.
The fundamental problem of physiological modelling of lesion significance is perhaps that it is simply not possible to predict using a computer model how a patient will respond in vivo to induction of hyperaemia and therefore how much trans-stenotic flow will actually occur on an individual basis. As it appears that most of the variability occurs at the FFR end – and not with the CFD model itself – it is perfectly plausible to imagine that these techniques would have a good ability to detect ischaemia, when compared to other perfusion or non-invasive measures of ischaemia. Any attempt to move away from pure anatomical assessment is welcome. Perhaps it is time for these CFD techniques to move away from FFR comparisons and find a niche as independent physiological tools to detect flow-limiting epicardial coronary disease.
We are now at an interesting crossroads in the field. Measurement of stenosis severity using coronary physiology clearly works. However, adoption remains stubbornly low. Recently, a range of technological innovations has been proposed as a solution to these problems. This will mean that the field will change sharply over the next few years. FFR really took off on the basis of large clinical outcome studies such as FAME. It is likely that the next large upswing in physiological adoption using newer approaches including computer-simulated physiological index will only take place when clinical outcome studies using these newer techniques show equivalence in the clinical laboratory.
Conflict of interest statement
J. Davies is a consultant for Volcano Corporation. The other authors have no conflicts of interest to declare.

