Abstract
Aims: This study analysed quality of life (QoL), anxiety and depression, headache and stress tolerance in patients with resistant hypertension before and after renal denervation (RDN).
Methods and results: RDN was performed in 119 patients (age 62±11 years, 55% male) with resistant hypertension (office blood pressure [BP] 165/91±22/15 mmHg), treated with 5.7±0.2 antihypertensive drugs. At baseline, at three and at six months after RDN, psychological status, intensity of headache and stress tolerance were documented. Stress was induced by a multitasking situation (Wiener Determination Task [DT]). Depression and anxiety (hospital anxiety and depression scale) and QoL (short form-12 health survey) were investigated. Intensity of headache was measured by visual analogous scale. Systolic and diastolic BP decreased by –20±2.4 and –10±1.4 mmHg, respectively, six months after RDN (p<0.0001). Patients showed more correct reactions (p<0.0001), fewer errors (p<0.05) and reacted faster (p<0.001) in the DT. Patients reported an improvement in QoL (p<0.05). Furthermore, anxiety (p<0.0001) and depression (p<0.0001) scores decreased. Intensity of headache decreased after RDN (p<0.01).
Conclusions: RDN is associated with reduced anxiety and depression, intensity of headache and with improved QoL and stress tolerance in patients with resistant hypertension.
Introduction
Therapy-resistant hypertension is associated with psychological comorbidities either contributing to or initiating the condition1-4. Dysfunction of the autonomic nervous system is considered to be the pathophysiological link between hypertension and psychological factors5. Depression may contribute as an independent risk factor to hypertension6. Psychological comorbidities like anxiety in addition to cardiovascular disease may contribute to significant impairments of quality of life (QoL), and consequently to increased rates of hospitalisation and morbidity7,8.
The associations between stressful life events, ongoing psychological stress, headache and hypertension are subjects of controversial debate9-13. The sympathetic nervous system and the hypothalamic-pituitary-adrenal axis are involved in stress reactions and in the regulation of blood pressure (BP) as well as in treatment resistance in hypertension14. Renal afferent and efferent sympathetic drive has been identified as a main contributor to the complex pathophysiology of resistant hypertension and the development of comorbidities and end-organ damage14-16. Renal denervation (RDN) has been demonstrated to reduce central and renal sympathetic activity, thereby improving BP control in patients with resistant hypertension17. Little is known about the extent of psychological impairments4,18,19 and the effect of RDN on these psychological entities4. The present study investigated anxiety, depression, QoL and stress levels in patients with resistant hypertension before and after RDN.
Methods
PARTICIPANTS
RDN was performed in 119 patients with resistant hypertension17. Patients were age ≥18 years and had an office BP of ≥160 mmHg despite being treated with ≥3 antihypertensive drugs (including a diuretic). Patients and treating physicians were instructed not to change antihypertensive medication during the study. Patients with known psychosis or dementia were excluded from the study. Inclusion and exclusion criteria for RDN have been described previously17. Patients were treated between March 2010 and January 2012, with subsequent follow-up at three and six months. All patients provided written informed consent. The study was approved by the local ethics committee in accordance with the Declaration of Helsinki.
DESIGN
In order to investigate the effects of RDN in patients with resistant hypertension we performed a pretest-treatment-posttest design. Pretest and posttest assessments were identical, both including a battery of cognitive tasks, questionnaires, and the assessment of clinical parameters. All patients were examined at each time point.
PSYCHOLOGICAL ASSESSMENT AND COGNITIVE TEST BATTERY
The cognitive test battery applied at pretest and posttests included the computerised standardised Wiener Determination Task (DT)20 validated for an age and gender-matched healthy normative control group. This multitasking test was used to measure reactive stress tolerance and executive functions (abilities like planning, action control, task switching). For this purpose patients had to react as exactly and quickly as possible to rapidly changing stimuli. Reaction time, number of correct reactions, incorrect reactions and omitted reactions and number of stimuli were scored. Anxiety and depression were measured by the self-assessment hospital anxiety and depression scale (HADS)21,22, specifically designed for physically diseased patients23. Clinically relevant depression and anxiety are assumed in patients’ scoring in the HADS subscales greater than 1124. To assess quality of life (QoL) the health status questionnaire (SF-12) was used. QoL is established as a relevant outcome parameter in patients with cardiac disease25,26. The SF-12 was validated not only for healthy persons but also for hypertensive patients (n=610)26. Patients were also instructed to rate their physical and mental state and arousal level on a 0-100% scale. Intensity of headache was assessed using the visual analogous scale (VAS; 0-10). Values greater than four points are interpreted as moderate to severe pain27.
PRIMARY AND SECONDARY ENDPOINTS
The primary endpoint was to examine stress tolerance and psychological factors like anxiety and depression in patients with resistant hypertension. We also investigated intensity of headache and QoL in patients with resistant hypertension. Secondary endpoints were to assess the delta between the previously described variables at baseline and follow-up measurement after RDN. We also assessed the impact of BP changes on psychological and cognitive functioning.
STATISTICAL ANALYSIS
Statistical analyses were performed using IBM SPSS version 20 Statistics for Windows (SPSS Inc., Chicago, IL, USA). Data were presented as mean ± SEM unless otherwise specified. We used a pretest-treatment-posttest design to determine the effects of RDN. Comparisons within the three sessions for categorical variables were performed using chi-square tests. We used repeated measures analysis of variance (ANOVA) with the within-subject factor session (baseline, three-month follow-up, six-month follow-up) to assess differences with respect to the cognitive data, depressive symptoms, anxiety, intensity of headache and QoL. To investigate the course of clinically relevant psychological disorders we performed subgroup analyses of variance. Correlative statistics were used to describe association between psychological factors and BP. Furthermore, we examined the effect of BP and heart rate on cognitive and psychological variables by calculating pre-RDN BP and heart rate as covariates in the ANOVA. To compare results of patients with resistant hypertension and normative controls (data derived from the corresponding manuals of specific tests) we calculated ratios based on the mean of performances. Sample size was calculated a priori by means of the software package G*Power 328.
Results
CLINICAL CHARACTERISTICS AND BP EFFECTS
The baseline characteristics of the 119 patients are presented in Table 1. Clinical data, cardiovascular risk factors, medical history as well as medication on admission are given. It has to be stated that the 84.9% of patients who were on beta-blockade at the start of treatment were maintained on beta-blockade throughout the six-month follow-up because of the known interactions between beta-blockade and intensity of headache29. Furthermore, as observed in clinical practice, in some patients the use of beta-blockers may also affect mood. Additionally, antidepressants and tranquillisers were used in approximately 15% of patients at the beginning of the trial and were not reduced in dosage or discontinued through six months. At baseline, the office BP of the patients was 165/91±22/15 mmHg despite being treated with 5.7±0.2 antihypertensive drugs. Changes in BP after RDN are summarised in Table 2. In the following paragraphs the results of the cognitive and psychological tests are presented.
STRESS TEST
In patients with resistant hypertension stress tolerance improved after RDN (Figure 1). Patients performed more correct reactions in the multitasking test at both measurement time points (p<0.001) compared to baseline values (Figure 1A). Furthermore, reaction times decreased (three-month follow-up vs. baseline p<0.01; six-month follow-up vs. baseline p<0.001) (Figure 1B) and the number of processed stimuli and correct reactions increased (for all p<0.001). While omissions decreased in patients (p<0.001) (Figure 1C), the number of commissions did not differ after RDN (Figure 1D).
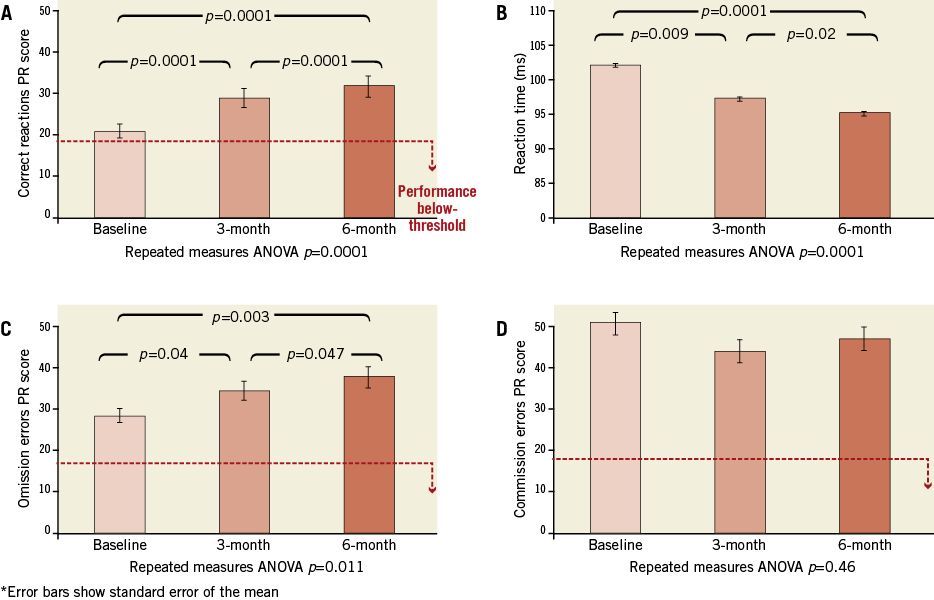
Figure 1. Reduced stress tolerance in patients with resistant hypertension after RDN. A) increase in correct reactions; B) decrease in reaction times; C) decrease in omission errors; D) commission errors.
ANXIETY AND DEPRESSION
Anxious (p<0.01) and depressive symptoms (p<0.001) were reduced in all patients undergoing RDN procedure (Figure 2A and Figure 2B).
The subgroup analysis of variance in clinically relevant anxious patients (21% of all patients) indicated an improvement after RDN (three-month vs. baseline p<0.01; six-month vs. baseline p<0.0001). According to HADS, 17% of all patients suffered from a clinically relevant depression, which improved after RDN (p<0.001) (Figure 2C).
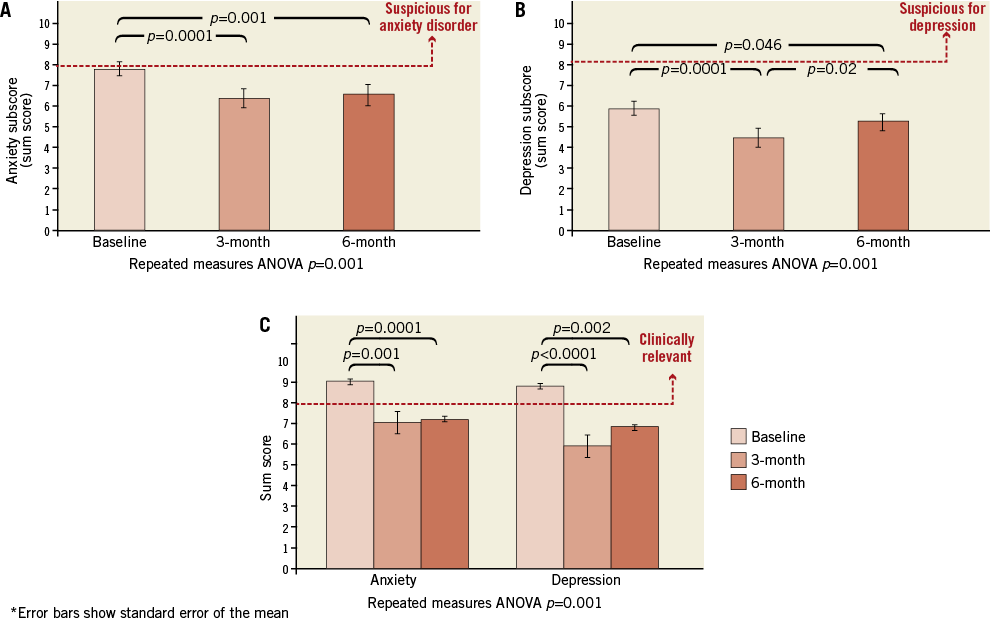
Figure 2. Reduced anxiety (A) and depression (B) in patients with resistant hypertension after RDN. Subgroup analysis of patients with clinically relevant anxiety and depression (C).
QUALITY OF LIFE, MENTAL AND PHYSICAL STATUS AND AROUSAL LEVEL
Evaluation by SF-12 revealed an improvement in physical health status after RDN (p=0.003) (Figure 3A). There was a trend towards an improved mental status (p=0.062) (Figure 3B) but not to the level of the hypertensive control group26. In contrast, regarding self-assessment on a 0-100% scale, physical state (p<0.0001) and mental state (p<0.001) improved after RDN. Self-reported arousal levels were reduced from 52% to 41% (p=0.001).
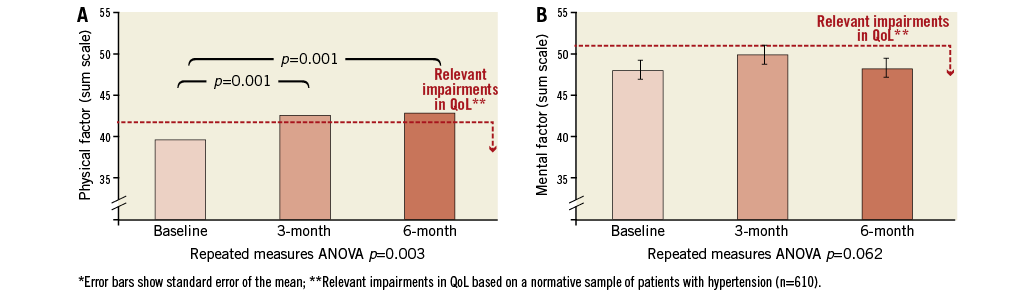
Figure 3. Quality of life, physical (A) and mental (B) health status, in patients with resistant hypertension before and after RDN.
HEADACHE
Intensity of headache decreased in all patients after RDN (p=0.008) (Figure 4). Twenty percent of all participants suffered from moderate to severe headache (VAS >4 points) (Figure 4). In these patients the intensity of headache decreased at three (p=0.009) and six-month follow-up (p<0.0001) after RDN compared to baseline values. All patients rated their pain lower than the critical four points after six months.
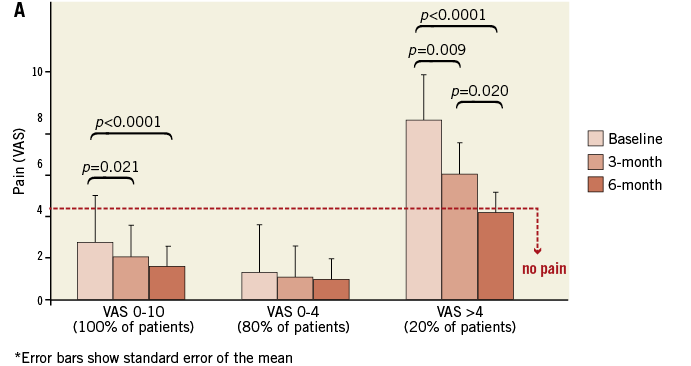
Figure 4. Intensity of headache measured by means of VAS for all patients, patients with no headache and patients with moderate to severe headache at baseline, 3 and 6-month follow-up.
THE ASSOCIATION OF BP, HEART RATE AND PSYCHOLOGICAL AND COGNITIVE FACTORS
There was a non-significant trend towards a correlation between heart rate and anxiety (p=0.06). Systolic BP was correlated with anxiety (p=0.01), depression (p<0.01) and the number of correct reactions in the DT (p=0.04). There was a trend towards an association between intensity of headache and diastolic BP (p=0.08).
By including vital parameters as covariates in the ANOVA measurements, we tested the influence of these factors on stress tolerance, anxiety, depression and intensity of headache. The number of correct items in the stress test was dependent on systolic BP at baseline (p=0.04). Heart rate trended to be predictive for anxiety levels (p=0.06).
To evaluate the association between psychological symptom change and BP changes after RDN, we divided our patient group into responders (systolic BP reduction of –10 mmHg) and non-responders, and put these as covariates in a repeated measures ANOVA. There were no significant differences regarding responders and non-responders in terms of psychological changes. Second, we used percentiles to calculate correlations between high, moderate or low systolic blood pressure reduction and changes in psychological variables. The improvement regarding psychological factors was independent from the extent of blood pressure reduction.
COMPARISON OF RESISTANT HYPERTENSION WITH CONTROL
Based on healthy normative sample groups we compared our results of patients regarding psychological factors and cognition (Figure 5). The HADS was validated in 4,410 healthy individuals21. Our patients (mean age 62±11 years) were 1.6-fold more anxious compared to the healthy sample of 60 to 70-year-old individuals. After RDN, the ratio was reduced to 1.35-fold. Regarding the multitasking stress test, patients performed 2.4-fold worse compared to the age and gender-matched sample. After RDN, the performance level was 1.6-fold worse.
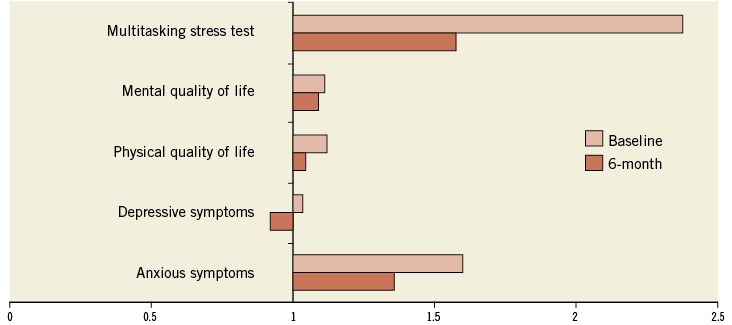
Figure 5. Comparison of patients with resistant hypertension before and after RDN with age and gender-matched healthy normative samples.
Discussion
RDN has been shown to reduce office BP and sympathetic activity in patients with resistant hypertension17,30-32. However, the effects of RDN on psychological processes can still be questioned. This study examined stress tolerance and psychological factors in patients with resistant hypertension before and after RDN. Patients with resistant hypertension are characterised by an impaired cognitive function, since the results of the multitasking stress test demonstrated a reduction of correct reactions and an elevation of omission errors compared to an age and gender-matched healthy normative sample20. The number of correct reactions was initially close to clinically relevant impairments in executive control processes. Patients improved significantly after a RDN procedure to a level comparable to the normative sample. The ability to react exactly and quickly to several task requirements is highly relevant in daily life activities and professional everyday life. Patients may focus better on rapidly changing situations and may be more flexible in their reactions after RDN. Among the elderly, about 30% suffer from mild to severe executive dysfunction, while in hypertensive patients as many as 50% are affected33,34. Antihypertensive treatment may lead to an improvement in executive dysfunction in the early stages34. Due to the high risk of conversion to dementia35, it is necessary to diagnose cognitive dysfunction in a timely manner. Cognitive dysfunction affects decision making and subsequent self-care36, leading to increased rates of hospitalisation and mortality37-39. In the multitasking test, systolic BP was predictive of the performance level at baseline. Therefore, systolic BP may play an important role regarding stress tolerance. Lowering sympathetic drive by RDN14 may result in a better stress tolerance. Heart rate is an indicator of cardiac autonomic activity and is reduced after RDN31. Recently, a study demonstrated the role of heart rate as a risk factor for mortality and cognitive decline in patients with stroke40.
In all patients with resistant hypertension, anxiety and depressive symptoms were reduced after RDN, while heart rate was an independent predictor of the anxiety level. Notably, 21% of the patients in the present study suffered from clinically relevant anxiety and 17% from clinically relevant depression. Depressive and anxious symptoms were reduced below the clinically relevant level after RDN, which is in line with the findings of Lambert et al4. Furthermore, QoL, mental and physical health status improved after RDN. Patients reported a reduction of their arousal level. The high prevalence of psychological comorbidities like anxiety disorder and depression in hypertensive patients is in line with the present findings3,5,19. Psychological comorbidities like depression lead to an impairment of QoL and may influence healthcare behaviour36. Depression in particular affects compliance and adherence to therapeutic interventions41, thereby raising the incidence of cardiovascular risk factors like diabetes, obesity and smoking42-44 and, as a consequence, hospitalisation and mortality rates increase39,45,46.
The association of headache and hypertension is the subject of controversial debate11,12. The results of the prospective and cross-sectional HUNT study (the Nord-Trondelag Health Study) showed that increasing systolic BP and pulse pressure were associated with decreased headache prevalence11. Other studies revealed that headache is more prevalent in patients with hypertension and especially in hypertensive crises12,47. In this study, 20% of patients suffered from moderate to severe headache. After RDN, these patients reported mild or no symptoms of headache, while there was no significant correlation with BP reduction. However, the results showed an association between the arousal level and the intensity of headache. This is consistent with cognitive behavioural models, postulating a significant role for psychological factors in maintaining symptoms of headache48.
The mechanisms of reduced stress tolerance, cognitive function and psychological impairment in patients with resistant hypertension after RDN remain unclear. Psychological factors like anxiety and depression symptoms2,6 in addition to lifestyle factors, such as smoking and physical inactivity as well as the metabolic syndrome42,49, may even contribute to the initiation of hypertension.
Based on the findings of this study, we hypothesised that the elevated sympathetic nervous activity in resistant hypertension leads to an impairment of stress tolerance, to a higher arousal level and consequently to higher anxiety levels and a reduction of QoL. One third of patients with major depressive disorder present a markedly elevated cardiac sympathetic activity50. Depression may also be associated with a dysregulation in the hypothalamic-pituitary-adrenal axis51. An activation of the renin-angiotensin system (RAS) and especially angiotensin II are not only associated with hypertension but also play a critical role in mood and anxiety disorders52. Activation of renal sympathetic efferent nerves causes renin release, sodium and water retention and reduced renal blood flow53,54. An increase in plasma levels of angiotensin II, mediated in part by renal sympathetic activation, has an effect on the central nervous system to increase global sympathetic activity further. Therefore, the reduction of sympathetic activity by RDN32,55 might be associated with a reduction of anxiety, depression and stress tolerance in patients with resistant hypertension.
Limitations
This is one of the first studies examining psychological comorbidities in patients with resistant hypertension before and after RDN. It has to be noted that future studies should address these issues in a randomised trial to confirm actual findings. Nevertheless, we used psychometric tests and questionnaires on the basis of healthy normative sample groups20,21,24. The computerised, standardised Wiener Determination Test is characterised by a high retest reliability20, and patients performed a training phase at each visit before the actual test started. The present study does not allow conclusions about the long-term development of psychological factors. Nevertheless, it has to be emphasised that there are no observational changes between the three and six-month follow-ups.
Conclusions
In patients with resistant hypertension, RDN significantly reduced office blood pressure and resting heart rate and did not affect psychological processes in a negative way. Moreover, RDN had a beneficial effect on psychological processes, stress perception and processing as well as QoL, and reduced the intensity of headache in patients with resistant hypertension. Hypertension is an important predictor of future cardiovascular events. The reported quality of life parameters may be added as relevant collateral benefits to the already known improvement of glucose control, ventricular diastolic function and heart rate31,56,57, all of which can occur independently from each other following RDN. Due to the prognostic relevance and taking into consideration the consequent healthcare costs of cognitive dysfunction and psychological disorders, it is important to take these factors into consideration during the process of prevention and treatment of hypertension and to include them as outcomes in future studies.
Funding
This study was funded by the Deutsche Gesellschaft für Kardiologie, Deutsche Herzstiftung (D. Lenski, I. Kindermann, M. Bunz and M. Böhm), Deutsche Forschungsgemeinschaft (DFG KFO 196 ZP, I. Kindermann, M. Böhm) and the Ministry for Education and Science of the Saarland (D. Lenski, I. Kindermann, M. Böhm). F. Mahfoud is supported by Deutsche Hochdruckliga.
Conflict of interest statement
All authors received scientific support from Medtronic/Ardian. F. Mahfoud, C. Ukena and M. Böhm received speaker honoraria from Medtronic.