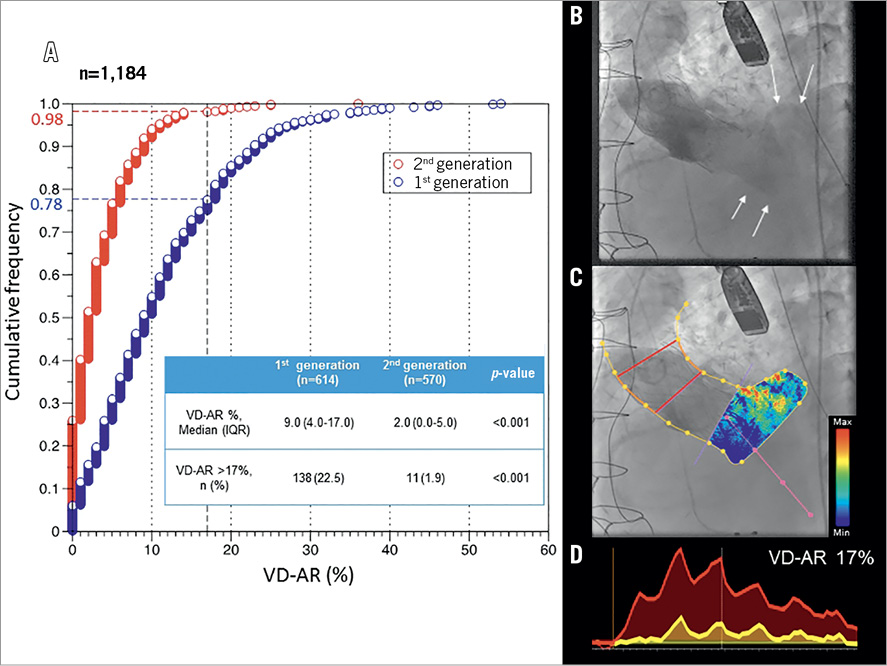
Paravalvular regurgitation (PVR) post transcatheter aortic valve implantation (TAVI) is a feared complication and relates greatly to clinical outcomes – increased late mortality. The development of newer devices with improved technology (enhancement of paravalvular sealing and retrieval/repositioning mechanisms) has decreased the incidence of moderate/severe PVR according to echocardiographic assessment in multiple studies. However, the assessment of PVR with echocardiography using standardised criteria from the Valve Academic Research Consortium (VARC-2) takes into account a wide range of parameters without thorough validation11. Abdelghani M, Soliman OI, Schultz C, Vahanian A, Serruys PW. Adjudicating paravalvular leaks of transcatheter aortic valves: a critical appraisal. Eur Heart J. 2016;37:2627-44. . PVR assessment during the procedure is challenging, especially in the era of the minimally invasive approach (without general anaesthesia). Videodensitometry assessment of aortic regurgitation (VD-AR) is an objective, quantitative, reproducible, well validated method, performed intraprocedurally with great correlation with magnetic resonance imaging22. Abdel-Wahab M, Abdelghani M, Miyazaki Y, Holy EW, Merten C, Zachow D, Tonino P, Rutten MCM, van de Vosse FN, Morel MA, Onuma Y, Serruys PW, Richardt G, Soliman OI. A Novel Angiographic Quantification of Aortic Regurgitation After TAVR Provides an Accurate Estimation of Regurgitation Fraction Derived From Cardiac Magnetic Resonance Imaging. JACC Cardiovasc Interv. 2018;11:287-97. ,33. Kapadia SR, Harb SC, Krishnaswamy A. Quantifying Paravalvular Aortic Regurgitation in Transcatheter Aortic Valve Replacement: The Pursuit of Perfection. JACC Cardiovasc Interv. 2018;11:298-300. ,44. Tateishi H, Campos CM, Abdelghani M, Leite RS, Mangione JA, Bary L, Soliman OI, Spitzer E, Perin MA, Onuma Y, Serruys PW, Lemos PA, Brito FS Jr. Video densitometric assessment of aortic regurgitation after transcatheter aortic valve implantation: results from the Brazilian TAVI registry. EuroIntervention. 2016;11:1409-18. . Briefly, it is a software-guided technique in which the density over time is measured in both the aortic root and the left ventricle outflow tract (region with the regurgitated jet) (Panel B, Panel C), and time-density curves are constructed (Panel D). Areas under the curves are calculated and their ratio is the result of the VD-AR assessment, representing the aortic regurgitation severity (Moving image 1). We conducted a retrospective post hoc analysis of post-TAVI aortograms from general clinical practice in an international, multicentre registry in Canada, the Netherlands, Brazil, USA, Germany and Japan. We have examined through an independent academic core laboratory 1,184 post-TAVI aortograms using the software CAAS A-valve 2.0.2 (Pie Medical Imaging BV, Maastricht, the Netherlands). Six different types of valve were implanted and divided into: (i) first-generation (CoreValve® [Medtronic, Minneapolis, MN, USA] and SAPIEN XT [Edwards Lifesciences, Irvine, CA, USA]), and (ii) second-generation (Evolut™ [Medtronic], SAPIEN 3 [Edwards Lifesciences], LOTUS™ [Boston Scientific, Marlborough, MA, USA] and CENTERA [Edwards Lifesciences]). Cumulative frequency curves for both generations were created (Panel A), showing that the second generation has a lower median value of VD-AR (2.0% vs. 9.0%, p<0.001) and a lower incidence of moderate to severe aortic regurgitation (VD-AR >17%)44. Tateishi H, Campos CM, Abdelghani M, Leite RS, Mangione JA, Bary L, Soliman OI, Spitzer E, Perin MA, Onuma Y, Serruys PW, Lemos PA, Brito FS Jr. Video densitometric assessment of aortic regurgitation after transcatheter aortic valve implantation: results from the Brazilian TAVI registry. EuroIntervention. 2016;11:1409-18. (1.9% vs. 22.5%, p<0.001) compared to the first. At first, this finding is easily explained by the device improvement over recent years. However, we also have to consider the growing experience of the operator, advancing on the “learning curve”, and the patient selection, evolving from inoperable to high- and intermediate-risk patients. From these results it might be prematurely concluded that the PVR has been resolved; however, interventions in bicuspid stenotic valves and aortic regurgitation are increasing, thus impacting negatively on the procedure. In conclusion, the improvement of the valves, operators and patient selection play roles in diminishing AR post TAVI. Glimpsing into the near future, the new VD-AR technology has excellent reproducibility, and its online assessment will probably become a useful tool for interventional cardiologists in assessing AR intraprocedurally and in guiding TAVI.
Guest Editor
This paper was guest edited by Alec Vahanian, MD, PhD; Department of Cardiology, Hôpital Bichat-Claude Bernard, and University Paris VII, Paris, France.
Acknowledgement
We thank Jean-Paul Aben for his help and support for the conception of this Interventional Flashlight article.
Conflict of interest statement
The authors have no conflicts of interest to declare. The Guest Editor is a consultant for Edwards Lifesciences.
Supplementary data
Moving image 1. Quantitative aortic regurgitation assessment with videodensitometry.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Quantitative aortic regurgitation assessment with videodensitometry.