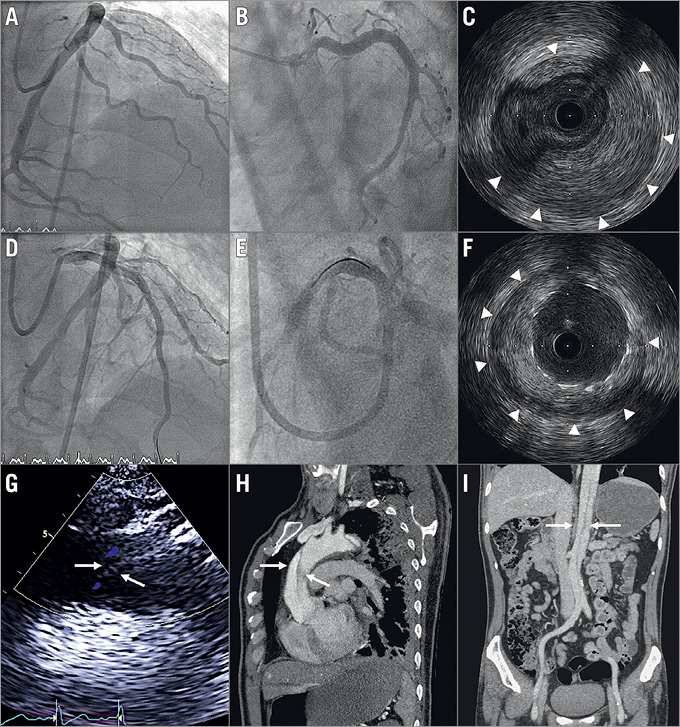
Figure 1. Multimodality cardiac imaging leads to prompt and correct diagnosis. A) Coronary angiogram from anterior-posterior (AP) cranial and (B) spider view showed occlusion of the left anterior descending (LAD) artery. C) Intravascular ultrasound (IVUS) revealed that the lumen of the LAD was compressed by a heavy intramural haematoma (IMH) (arrowheads). D) Final angiogram from the AP cranial and (E) spider view showed good LAD flow after stenting. F) IVUS showed well-expanded stents pushing the IMH (arrowheads) outwards. G) An intimal flap (arrows) was identified by the transthoracic echocardiogram from a suprasternal view. H) Sagittal and (I) coronal view of computed tomography confirmed the aortic dissection (arrows), Stanford type A.
A 49-year-old man who had smoked two packs of cigarettes per day for thirty years presented with acute onset of chest pain. Twelve-lead electrocardiography indicated acute ST-segment elevation myocardial infarction (STEMI) of the anterior wall. He subsequently underwent percutaneous coronary intervention. Coronary angiography showed an occluded left anterior descending (LAD) coronary artery from the ostium (Figure 1A, Figure 1B). An extensive intramural haematoma (IMH) was found on intravascular ultrasound (IVUS), which extended from the ostium of the left main coronary artery to the mid LAD (Figure 1C, Moving image 1). Balloon dilation was performed to create a fenestration. The LAD blood flow improved after stents were deployed from the ostial to mid LAD (Figure 1D, Figure 1E), pushing the haematoma towards the vessel wall (Figure 1F, Moving image 2).
Noting that IMH in proximal coronary arteries is an unusual cause of STEMI, we arranged transthoracic echocardiography to check for possible aortic diseases. An intima flap was found in the aortic arch (Figure 1G). Computed tomography of the chest confirmed a Stanford type A aortic dissection (Figure 1H, Figure 1I). The patient underwent surgical aortic repair and was discharged three weeks later.
Aortic dissection is a rare cause of acute myocardial infarction (AMI). The suspicion of dissection often arises from an abnormality on the aortogram1. In this case, the proximal IMH found by IVUS gave us a hint of concomitant aortic dissection before aortography was performed.
Intracoronary imaging, such as IVUS or optical coherence tomography (OCT), is helpful for evaluating coronary lesions. However, optimal OCT imaging is usually technically unfeasible for ostial lesions2. OCT has also been associated with a higher risk of vessel dissection due to forceful contrast injection3,4. Thus, IVUS is suggested first to examine the proximal vessel structure in AMI patients. Interventional cardiologists need to be aware of possible concomitant acute aortic syndrome in patients with acute coronary syndrome, especially when a proximal IMH is present.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
Moving image 1. Initial intravascular ultrasound images acquired from distal left anterior descending (LAD) artery to left main coronary artery revealed extensive intramural haematoma extending from the left main ostium to middle LAD.
Moving image 2. Intravascular ultrasound images acquired from the distal left anterior descending artery to the left main coronary artery after stenting. The stents were well expanded and the intramural haematoma was pushed towards the vessel wall.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Initial intravascular ultrasound images acquired from distal left anterior descending (LAD) artery to left main coronary artery revealed extensive intramural haematoma extending from the left main ostium to middle LAD.
Moving image 2. Intravascular ultrasound images acquired from the distal left anterior descending artery to the left main coronary artery after stenting. The stents were well expanded and the intramural haematoma was pushed towards the vessel wall.