
In this issue of EuroIntervention Kjøller-Hansen and colleagues report the results of a post hoc analysis of the SORT OUT II trial comparing the 10-year rate of a composite outcome of death, myocardial infarction and repeat revascularisation between patients receiving a single drug-eluting stent in the proximal left anterior descending (LAD) vs. non-proximal LAD1. The authors report no difference between the two groups (HR 0.82, 95% CI: 0.65-1.03).
The analysis has some limitations. The definition used by the authors is somewhat arbitrary and difficult to understand: why not compare LAD vs. non-LAD lesions? Why group the distal LAD with the circumflex or right coronary artery? Lesions of the proximal LAD are traditionally considered to have significantly higher prognostic significance than any other coronary lesions2, so the biologic rationale for the comparison is also questionable.
Most importantly however, with only 365 patients and 90 events in the proximal LAD group, the study is largely underpowered to detect even moderate differences between groups.
It is interesting to note how the authors quote in the text two surgical series comparing percutaneous intervention with minimally invasive surgical revascularisation for treatment of proximal LAD disease3,4 that, with 189 and 130 patients respectively, share both the sample size limitations and the negative conclusions of their paper.
Power is a crucial factor of every analysis. Studies with a small sample size have a high risk of type I and type II errors (Figure 1). When negative (as in this case), underpowered studies have substantial chances of missing true treatment effects. When positive, they are very likely to provide wrong estimates of the treatment effect. The limitations of underpowered studies and the risk associated with their interpretation in different fields of medical research have been described repeatedly5.
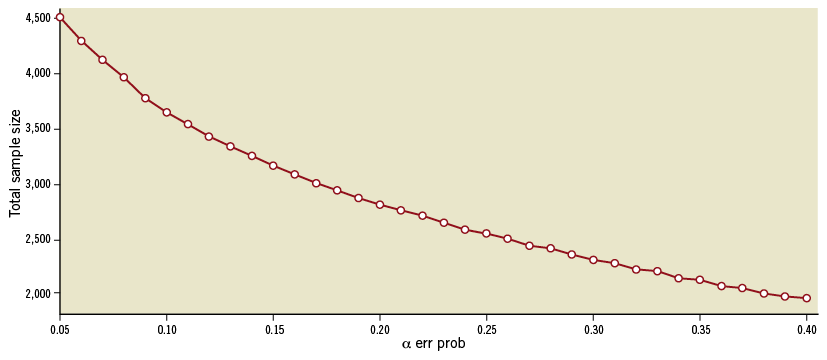
Figure 1. Correlation between sample size and p-value for a 20% assumed relative risk reduction between proximal LAD and non-proximal LAD groups.
It is worth noting that recently two very important clinical questions in the cardiovascular field have been answered using a meta-analytic approach. Head et al, combining the patient-level data of 11 randomised trials comparing coronary surgery with percutaneous interventions in the treatment of patients with multivessel disease, were able to show for the first time a significant difference in mortality in favour of the surgical arm6. Our group, by combining individual data from six trials comparing the use of the radial artery with the saphenous vein as the second conduit in coronary surgery provided the first demonstration of a clinical benefit associated with the arterial conduit based on randomised data7.
Unfortunately, the merging of individual data sets requires a substantial amount of resources, time and persistence. Despite the recommendations of scientific and professional societies and scientific journals, sharing of data is still a complex and often painful process. However, the uncertainty and risk inherent in small studies should not be underestimated, and every effort should be made to provide the scientific community and our patients with data from adequately powered studies.
Conflict of interest statement
The authors have no conflicts of interest to declare.

