When an ischaemia-provoking lesion in the proximal right coronary artery (RCA) or left circumflex (LCx) artery is detected, operators may immediately proceed to perform percutaneous coronary intervention (PCI). However, if the lesion is located in the proximal left anterior descending (LAD) artery, current guidelines advise pausing first to discuss the need for and the optimal method of revascularisation.
As the LAD artery supplies 45-55% of the left ventricular myocardium, LAD disease is thought to represent a higher cardiovascular risk. Consequently, in the revascularisation guidelines there are special sections dedicated not only to left main coronary artery disease and three-vessel disease but also to the proximal LAD coronary artery segment.
Data that compare outcomes after revascularisation for proximal versus non-proximal LAD lesions are limited and quite old. Data on clinical outcomes in isolated proximal LAD revascularisation are predominantly from the bare metal stent era. These outdated trials found no significant difference in mortality, myocardial infarction (MI) or stroke, but a threefold higher rate of recurrent angina and a fivefold higher rate of repeat revascularisation after PCI versus coronary artery bypass surgery (CABG).
In recent years we have seen major efforts to improve PCI outcomes. However, the impact of proximal LAD lesion location on long-term outcomes is poorly understood in the context of PCI with contemporary stents, superior procedural techniques, risk factor modification, and current medical therapy. Randomised studies such as NOBLE and EXCEL have advanced our knowledge regarding treatment of the left main stem. Still, it is not well understood whether the presence of a significant proximal LAD narrowing is a predictor of adverse outcome. But what would happen if we find that the clinical outcome is similar whether a stent is implanted in the proximal LAD or in the RCA or in the LCx? Would this change the guidelines and the way we practise?
In this issue of EuroIntervention, a Danish research group reports highly interesting 10-year outcome data of the SORT OUT II trial that assessed 2,131 patients treated with first-generation (CYPHER® [Cordis, formerly Johnson & Johnson, now Cardinal Health, Milpitas, CA, USA] or TAXUS™ [Boston Scientific, Marlborough, MA, USA]) drug-eluting stents (DES)1.
In 1,479 (69.4%) patients with single lesion treatment, 365 patients with proximal LAD stenting were compared with 1,114 patients who were stented in a single other (i.e., non-proximal LAD) segment. Follow-up was available in 99.3% of patients, showing a similar long-term prognosis for the proximal LAD and non-proximal LAD groups with a similar all-cause mortality (24.9% vs. 26.3%). Major adverse cardiac events (MACE) occurred less frequently in the proximal LAD group (24.6% vs. 31.0%). While this difference was significant in an unadjusted analysis (p=0.02), multivariate analysis showed that the non-proximal LAD lesion site was not an independent predictor of MACE (p=0.09). In an additional secondary analysis, including patients treated for multiple lesions, the 10-year MACE and survival rates were still similar for both lesion site groups. The authors concluded that patients treated with DES implantation in the proximal LAD have a similar, if not better, long-term clinical outcome compared with patients stented in other coronary segments.
Interestingly, in the SORT OUT II trial, patients treated with TAXUS and CYPHER stents showed similar outcomes. As outlined by the authors, stent and lesion characteristics might partly explain the somewhat lower MACE rate in the proximal LAD group. The present study complements previous research as it provides very long follow-up data with important insights into the natural course and progression of atherosclerosis, which contributed to the observed event rates. For instance, the rate of MI that could be ascribed to a treatment failure was 60.9% (proximal LAD) and 54.5% (non-proximal LAD), while almost half of all MI events were not directly related to an index target lesion.
In clinical practice, many of our patients with proximal LAD lesions do not have single target lesions. We oftenface the question: what is the optimal revascularisation method in patients with proximal LAD lesion and multivessel disease? Two recent publications have addressed this issue (Table 1).
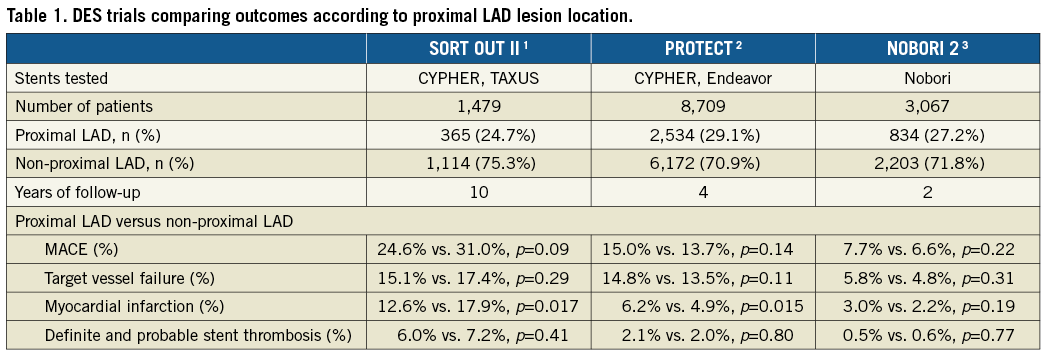
The PROTECT trial enrolled 8,709 patients treated with CYPHER or Endeavor® (Medtronic, Minneapolis, MN, USA) DES2. Patients who received at least one stent in the proximal LAD were compared to patients stented in non-proximal LAD segments. Notably, patients with stent implantation in the proximal LAD plus another location were classified as being in the proximal LAD group. At four-year follow-up, mortality rates were identical (5.8% vs. 5.8%, p>0.99), while more MI occurred in the proximal LAD group (6.2% vs. 4.9%, p=0.015). Event rates were similar for the endpoints: clinically driven target vessel failure (TVF) (14.8% vs. 13.5%, p=0.11), MACE (15.0% vs. 13.7%, p=0.14), and stent thrombosis (2.1% vs. 2.0%, p=0.80). DES type showed no interaction with MACE or TVF. Moreover, in a multivariate analysis the proximal LAD was a predictor of MI (p=0.04) but not of TVF (p=0.15) or MACE (p=0.07).
The NOBORI 2 trial enrolled 3,067 consecutive patients treated with the Nobori® (Terumo Corp., Tokyo, Japan) DES in 125 centres. Patients stented in the proximal LAD (834 [27.2%]) were compared with patients in whom stenting in one or more segments other than the proximal LAD was performed (2,203 [71.8%])3. The proximal LAD group had a lower clinical risk but higher angiographic complexity. At one- and two-year follow-up, no difference was found between the groups in the occurrence of the primary composite endpoint (cardiac death, MI or target lesion revascularisation) (6.0% vs. 4.6%, p=0.14, and 7.7% vs. 6.6%, p=0.22, respectively). Multivariate analysis showed that the proximal LAD location did not predict the primary endpoint or MACE. In addition, for both groups, event rates were similar for stent thrombosis and relief from anginal symptoms.
The internal mammary artery (IMA) conduit as bypass to the LAD is a good treatment option for patients with proximal (or mid) LAD lesions. Nevertheless, some issues should be taken into account. The IMA may fail in 2-9%4, and there is no significant difference in five-year mortality or other cardiovascular event rates between patients who receive single versus bilateral IMA grafts5. In addition, bilateral IMA grafting is associated with more sternal wound complications (1.9% versus 0.6%) which is associated with significant morbidity5. Nevertheless, referring patients who are at low surgical risk and are likely to have long-term benefit for bypass surgery represents good clinical practice. However, many patients with proximal LAD lesions can be safely treated by stenting which often leads to excellent long-term outcomes6.
Randomised trials of PCI versus CABG for proximal LAD lesions are unlikely to be performed. In addition, such trials, as all revascularisation trials, carry the risk of selection bias for inclusion in the PCI arm. Although the proximal LAD lesion site is known generally to be a higher-risk location, in all three stent trials discussed above1-3 the demographic characteristics of the proximal LAD subgroup represented a lower risk at patient level while the angiographic risk characteristics were higher than in patients stented in non-proximal LAD segments. While procedures in the proximal LAD are considered to be high risk mainly due to the large amount of myocardium that is dependent on the blood flow in this segment, some of its characteristics actually favour PCI, such as larger diameter stents, higher flow and limited tortuosity.
A general challenge of stent trials is that current technology may have advanced beyond the evaluated devices by the time the trial results are reported. The results presented are only hypothesis-generating. Yet, we feel that it is unlikely that treatment of the proximal LAD with latest-generation DES would result in worse outcomes. Thus, the findings of SORT OUT II and previous studies suggest that, in the current era of new-generation DES, the proximal LAD segment no longer confers a different prognosis than other target lesion sites. These data may be seen as a strong argument in favour of removing the apparently outdated barrier to PCI for lesions in the proximal LAD segment.
Conflict of interest statement