Abstract
Background: Despite transcatheter aortic valve implantation (TAVI) having become a routine procedure, access site bleeding and vascular complications are still a concern which contribute to procedure-related morbidity and mortality.
Aims: The TAVI-MultiCLOSE study aimed to assess the safety and efficacy of a new vascular closure algorithm for percutaneous large-bore arterial access closure following transfemoral (TF)-TAVI.
Methods: All consecutive TF-TAVI cases in which the MultiCLOSE vascular closure algorithm was used were prospectively included in a multicentre, observational study. This stepwise algorithm entails the reinsertion of a 6-8 Fr sheath (primary access) following the initial preclosure with one or two suture-based vascular closure devices (VCDs). This provides the operator with the opportunity to perform a quick and easy angiographic control and tailor the final vascular closure with either an additional suture- or plug-based VCD, or neither of these.
Results: Among 630 patients who underwent TF-TAVI utilising the MultiCLOSE algorithm, complete arterial haemostasis was achieved in 616 patients (98%). VCD failure occurred in 14 patients (2%), treated with either balloon inflation (N=1), covered stent (N=12) or surgical repair (N=1). Overall, this vascular closure approach resulted in a minor and major vascular complication rate of 2.2% and 0.6%, respectively. At 30 days, only one new minor vascular complication (0.2%) was noted. In-hospital and 30-day all-cause mortality rates were 0.2% and 1.0%, respectively.
Conclusions: Use of the MultiCLOSE vascular closure algorithm was demonstrated to contribute to an easy, safe, efficacious and durable vascular closure after TF-TAVI, resulting in a major vascular complication rate of less than 1%.
Introduction
Transcatheter aortic valve implantation (TAVI) has become the first-choice treatment for elderly patients with severe, symptomatic aortic stenosis123456. Over the past years, there has been a large focus on the simplification and optimisation of the TAVI procedure, along with early patient discharge. One of the key conditions to implement such a practice is having complete control of the large-bore arterial access closure after TAVI.
Despite TAVI having become a routine procedure, access site bleeding and vascular complications related to the primary access are still a concern, as these are associated with procedure-related morbidity and mortality78. Meticulous computed tomography (CT) preprocedural planning and ultrasound-guided vascular puncture have contributed to a decrease in vascular complications related to TAVI. In addition, the availability of dedicated vascular closure devices (VCDs) has enabled the successful percutaneous closure of large-bore arteriotomies910. However, different closure techniques are used worldwide, with different success and failure rates1112131415.
In this prospective, multicentre, observational study, we aimed to investigate the safety and efficacy of a systematic, stepwise approach for percutaneous large-bore arterial access closure following TAVI – referred to as the MultiCLOSE algorithm – which integrates a cascade of possible safety nets.
Methods
STUDY DESIGN AND PATIENT POPULATION
The TAVI-MultiCLOSE study is a prospective, multicentre, observational study which was conducted in three TAVI centres: one in Denmark and two in Belgium. All consecutive patients that underwent standard transfemoral (TF)-TAVI between May 2022 and June 2023 (Denmark) and September 2022 and June 2023 (Belgium) were included in the study. The only TF-TAVI patients that were excluded from the study were patients who had undergone intravascular lithotripsy-assisted TF-TAVI with a contralateral angiographic vascular closure control (N=18 in this study period). The study was approved by the local ethics committees and complied with the Declaration of Helsinki.
MULTICLOSE VASCULAR CLOSURE ALGORITH
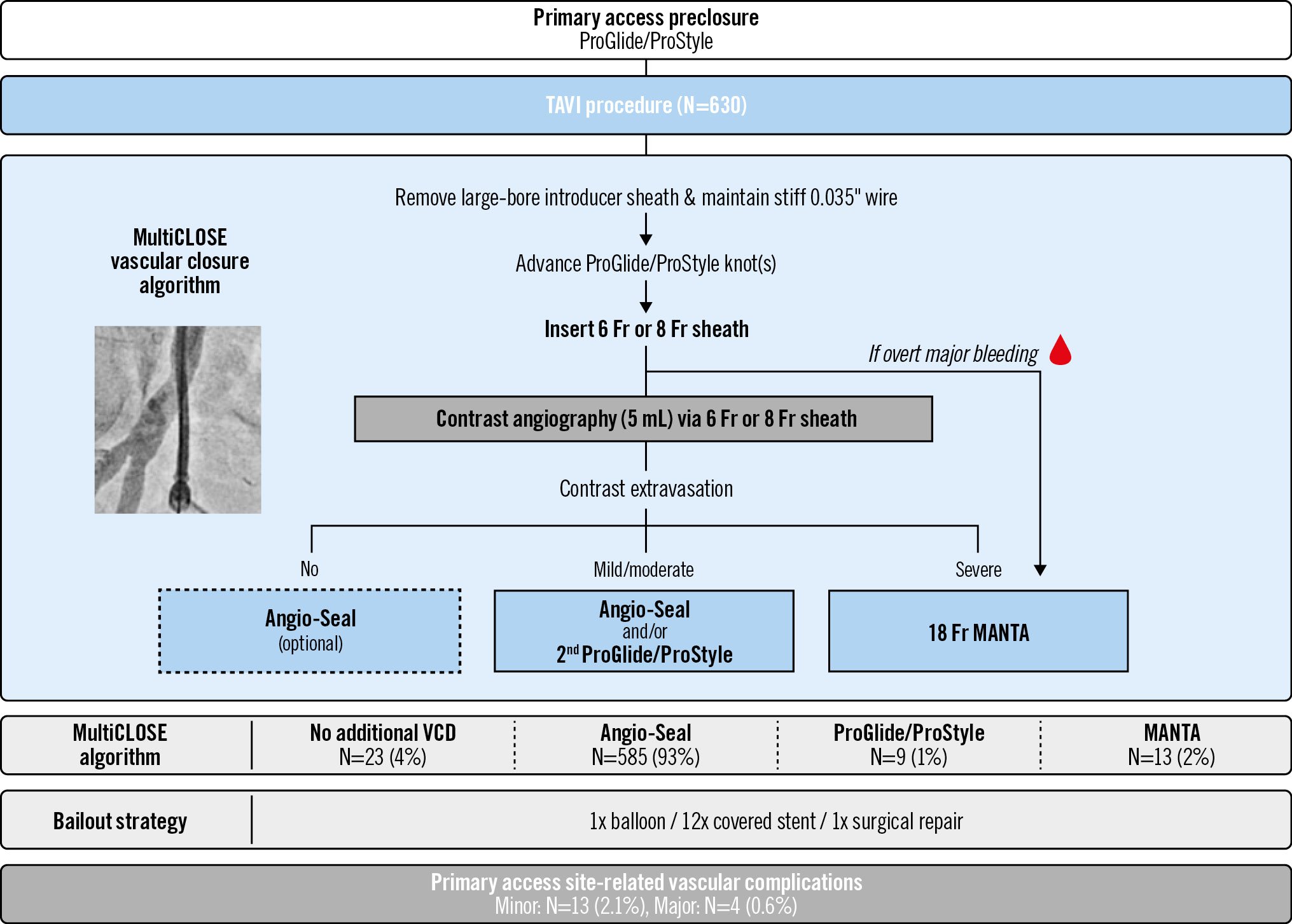
All three TAVI centres implemented the same MultiCLOSE vascular closure algorithm (Figure 1) in order to verify and obtain vascular closure following TF-TAVI. After ultrasound-guided arterial puncture of the primary access, a fluoroscopic image of the needle position at the arteriotomy site was stored. This stored fluoroscopic image is used as a reference image for the possible future deployment of a MANTA VCD (Teleflex) or positioning of a balloon or covered stent, if needed. Alternatively, one can premeasure the skin-to-arteriotomy distance at this stage by introducing the sheath of the Angio-Seal VCD (Terumo) (Figure 2). Next, preclosure with a single or double ProGlide or ProStyle (Abbott) was performed. After transcatheter aortic valve (TAV) deployment and removal of the delivery system, the large-bore introducer sheath was removed, keeping a 0.035” stiff guidewire in situ, while the suture knot(s) of the ProGlide/ProStyle were advanced a first time. Next, a short 6 Fr or 8 Fr sheath was introduced over the 0.035” stiff guidewire and the suture knot(s) were further tightened. The selection of a 6 Fr or 8 Fr sheath was left to the discretion of the TAVI operator and was guided by the degree of externally visible “oozing” or bleeding following initial vascular closure with the ProGlide/ProStyle. If no overt external bleeding was observed after introduction of the 6-8 Fr sheath, an angiography (approx. 5 ml contrast) through this short sheath was performed in order to detect residual extravasation beside the sheath or any other vascular complication. If no extravasation was observed (Moving image 1), either no additional VCD was used or a plug-based Angio-Seal (6 Fr or 8 Fr) was deployed after removal of the 6-8 Fr sheath, followed by a final tightening of the suture knot(s). In case of mild or moderate contrast extravasation at angiography (Moving image 2, Moving image 3), an Angio-Seal (mild) or additional ProGlide/ProStyle (moderate) was recommended, again followed by tightening of the suture knot(s) as the final step. The decision to use a 6 Fr or 8 Fr Angio-Seal was at the operator’s discretion and was guided by the Fr size of the short sheath utilised and/or degree of residual contrast extravasation beside the sheath.
In case of overt major bleeding or major contrast extravasation following tightening of the ProGlide/ProStyle(s) (Moving image 4), the larger plug-based 18 Fr MANTA VCD could be instantly introduced on the stiff guidewire and deployed. In order to expose the anchor of the MANTA VCD at the correct depth, the operator can use one or both of the proposed methods in Figure 2. They could use either the initially stored fluoroscopic image of the needle’s arteriotomy site position or the depth measurement of the skin-to-arteriotomy distance, by means of the Angio-Seal sheath, in order to deploy the MANTA VCD at the correct depth.
Postprocedural protamine administration was left to the discretion of the operator, and a control vascular ultrasound was only performed when clinically indicated.
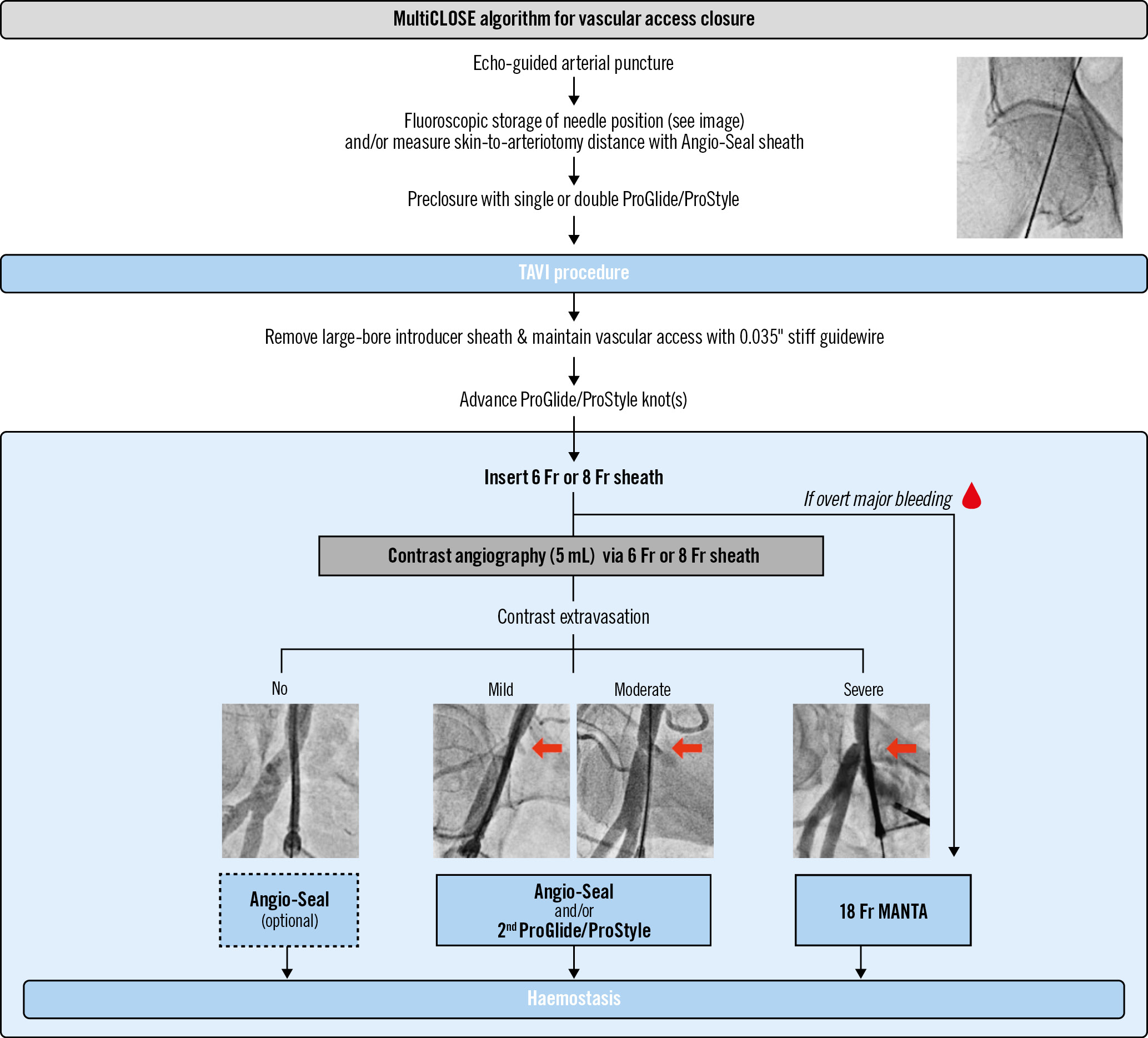
Figure 1. MultiCLOSE algorithm for vascular access closure. Novel and central to this vascular closure algorithm is the insertion of a 6 Fr or 8 Fr sheath following initial closure with one or two suture-based ProGlide/ProStyle(s). This provides the opportunity to perform a quick and easy angiographic control without the need to crossover from the contralateral femoral side or advance a catheter via the radial access, thereby saving time, contrast dye and radiation. A detailed description of this vascular closure algorithm can be read in the Methods section. TAVI: transcatheter aortic valve implantation
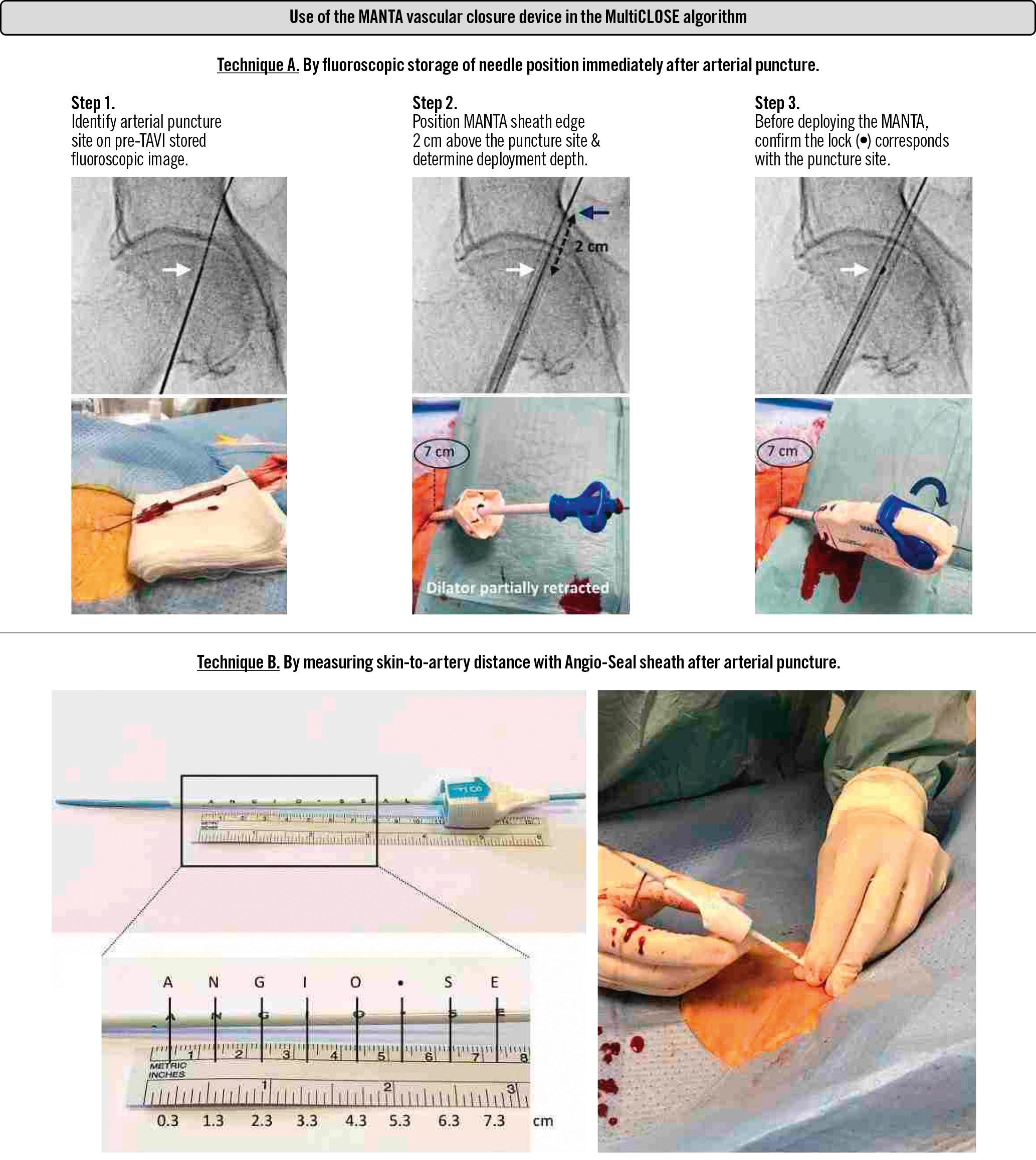
Figure 2. Use of the MANTA vascular closure device in the MultiCLOSE algorithm. Technique A: This methodology should be used in case the skin-to-artery distance is unknown. Step 1: review the fluoroscopically stored image of the needle puncture site in relation to the femur head at the start of the TAVI procedure. Step 2: insert the MANTA sheath over the stiff guidewire and partially retract the dilator to permit fluoroscopic visualisation of the distal edge of the MANTA sheath. Position the distal edge of the MANTA sheath 2 cm cranial to the puncture site. Note the MANTA deployment depth in centimetres at the skin level. Fully reinsert the dilator and advance the MANTA sheath. Step 3: remove the dilator, introduce the collagen plug, retract the MANTA device to the deployment depth determined in Step 2, expose the anchor by rotating the deployment lever, and deploy the MANTA device as usual. Technique B: This methodology can be used when the operator is almost certain of using an Angio-Seal device for final vascular closure. Using the letters on the Angio-Seal sheath, the operator can measure the skin-to-artery distance. The MANTA deployment depth is between +1.5 and +2.0 cm in comparison to the measured skin-to-artery distance. TAVI: transcatheter aortic valve implantation
DATA COLLECTION
Baseline patient and procedural characteristics were prospectively collected in a dedicated electronic case report form. Procedural data encompassed the type and size of TAV and introducer sheath and the site of the primary and secondary access for TAVI. For the purpose of this study, the type and number of VCDs utilised were meticulously documented, including the Perclose ProGlide/ProStyle system, the Angio-Seal and MANTA VCDs. In addition, bailout strategies and any material (balloon, covered stent, surgical repair) used in case of unsatisfactory vascular closure were also documented.
ENDPOINTS AND DEFINITION
The primary endpoint was defined as in-hospital major vascular complications. Secondary endpoints included in-hospital minor vascular complications, 30-day minor and major vascular complications, VCD failure, and the need for endovascular (balloon and/or covered stent) or surgical intervention. All outcomes were defined according to the Valve Academic Research Consortium (VARC)-3 criteria16.
STATISTICAL ANALYSIS
Descriptive statistics were used to present baseline variables and primary and secondary endpoints. Continuous variables are reported as mean and standard deviation (±SD) in normal number distribution and as median and interquartile range (IQR) for skewed number distribution. Categorical variables are presented as counts and percentages.
Results
STUDY POPULATION
During the study period, a total of 630 patients underwent standard TF-TAVI: 489 patients were included from one high-volume Danish centre and another 70 and 71 patients were included from two Belgian centres. Baseline patient and procedural characteristics are summarised in Table 1. Of the total study cohort, 553 (88%) had TAVI performed via a right-sided transfemoral approach, and the radial artery was used as secondary access in 72 cases (12%). The relatively low use of the radial artery for introduction of the pigtail catheter was mainly due to the frequent use of a cerebral embolic protection device in this patient cohort.
Table 1. Baseline characteristics.
| N=630 | |
|---|---|
| Patient characteristics | |
| Age, years | 79±7 |
| Female | 263 (42) |
| Arterial hypertension | 462 (73) |
| Diabetes mellitus | 132 (21) |
| Body mass index, kg/m2 | 26 [23.5-29.5] |
| Atrial fibrillation | 222 (35) |
| Previous stroke | 74 (12) |
| Coronary artery disease | 255 (40) |
| Peripheral arterial disease | 56 (9) |
| Chronic renal failure§ | 19 (3) |
| Oral anticoagulation | 213 (34) |
| EuroSCORE II, % | 2.2 [1.3-3.7] |
| Procedural characteristics | |
| Transcatheter aortic valve | |
| Navitor (Abbott) | 239 (38) |
| Evolut R/PRO(+) (Medtronic) | 215 (34) |
| ACURATE neo2 (Boston Scientific) | 145 (23) |
| SAPIEN 3/Ultra (Edwards Lifesciences) | 31 (5) |
| Introducer sheath type/size | |
| 14 Fr expandable sheath | 326 (52) |
| 14 Fr sheath+exchanged for integrated sheath | 192 (30) |
| 16 Fr expandable sheath | 13 (2) |
| 16 Fr sheath+exchanged for integrated sheath | 35 (6) |
| 18 Fr sheath±exchanged for integrated sheath | 44 (7) |
| 20 Fr sheath±exchanged for integrated sheath | 20 (3) |
| Secondary access | |
| Contralateral femoral artery | 558 (89) |
| Radial artery | 72 (11) |
| Data are presented as mean±standard deviation, n (%) or median [interquartile range]. § estimated glomerular filtration rate <30 mL/min/1.73 m2. EuroSCORE: European System for Cardiac Operative Risk Evaluation | |
VASCULAR CLOSURE MANAGEMENT OF TAVI PRIMARY ACCESS SITE
In all 630 study patients, ultrasound-guided arterial puncture and preclosure with one (N=152; 24%) or two (N=478; 76%) suture-based ProGlide/ProStyle(s) was undertaken. Following removal of the large-bore introducer sheath, a 6 Fr or 8 Fr sheath was inserted in 623 patients (99%) in order to perform a control angiography. In 7 patients (1%), the ProGlide/ProStyle system failed resulting in overt major bleeding, for which the operator immediately switched to using a MANTA VCD. Following control angiography, no additional VCD, an additional Angio-Seal, an additional ProGlide/ProStyle, or MANTA VCD were used in 23 (4%), 585 (93%), 9 (1%) and 6 (1%) patients, respectively (Figure 3).
In 14 patients (2.2%), there was incomplete vascular closure following the MultiCLOSE algorithm. An endovascular bailout was successful in 13 of these patients (balloon: N=1; covered stent: N=12). In one patient, surgical vascular repair was needed; this was due to unsatisfactory vascular closure with 2 ProGlides and 1 Angio-Seal (Figure 3). In nearly all patients (N=628), protamine was administered at the end of the procedure.
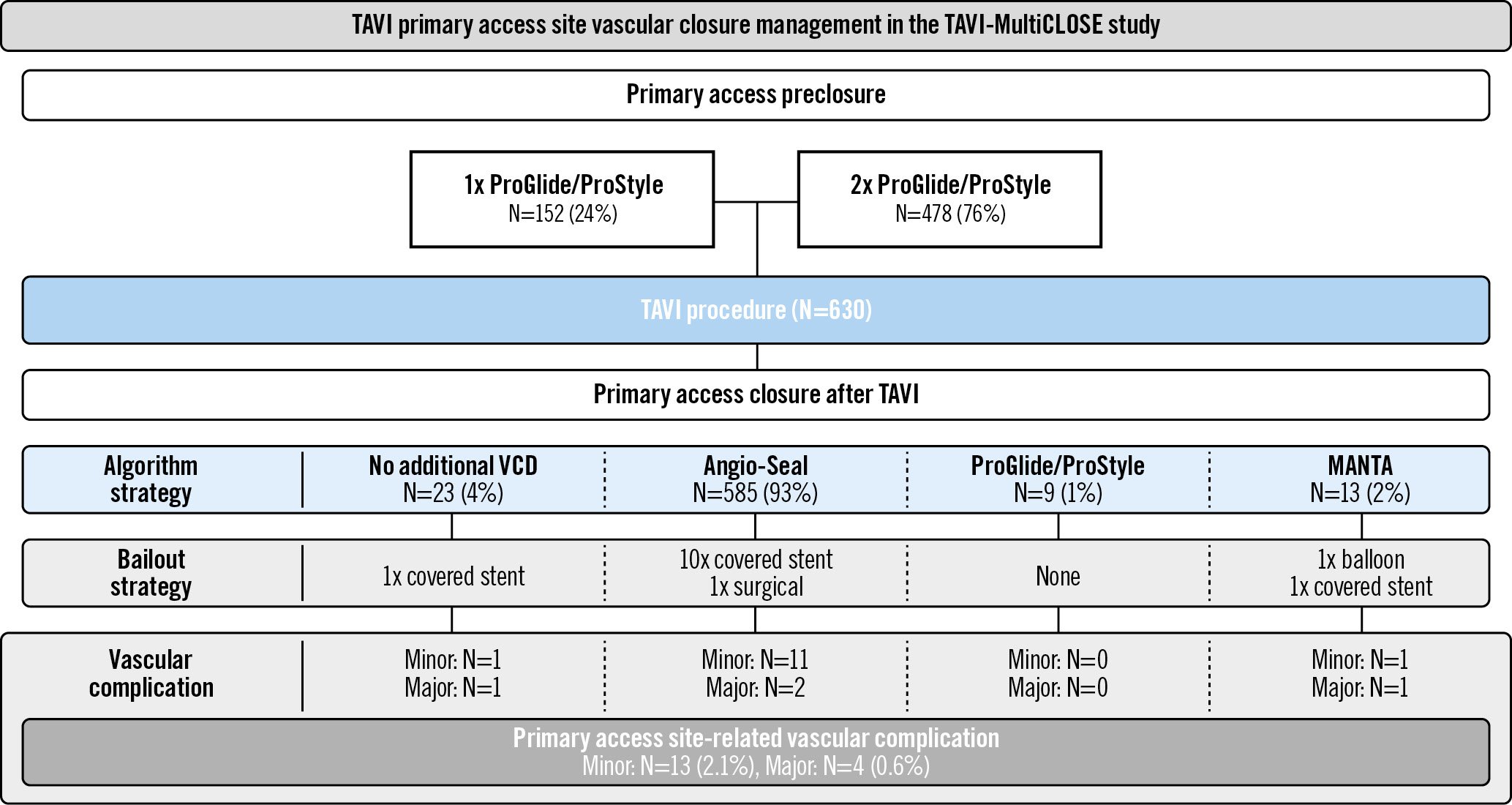
Figure 3. TAVI primary access site vascular closure management in the TAVI-MultiCLOSE study. The vascular closure strategies and outcomes in the TAVI-MultiCLOSE study, including 630 TAVI patients treated by a percutaneous transfemoral approach and resulting in a major primary access site-related vascular complication rate of 0.6%. TAVI: transcatheter aortic valve implantation; VCD: vascular closure device
PRIMARY AND SECONDARY ENDPOINTS
The primary endpoint occurred in 4 patients (0.6%); these patients had a VARC-3-defined in-hospital major vascular complication (Table 2). Major vascular complications occurred because of VCD failure leading to VARC type ≥2 bleeding, and final haemostasis was achieved by means of prolonged balloon inflation (N=1), covered stent placement (N=2) or surgical repair (N=1) (Supplementary Table 1).
An additional 14 patients (2.2%) had minor vascular complications: 13 complications were at the primary access site and one pseudoaneurysm was at the secondary femoral access site (Supplementary Table 1). Only one patient presented with a new minor vascular complication at 30-day follow-up.
In-hospital and 30-day all-cause mortality rates were 0.2% (N=1) and 1.0% (N=6), respectively. In-hospital mortality occurred as a result of coronary obstruction during a valve-in-valve procedure. None of the mortalities were attributed to an access site-related complication.
Table 2. Clinical outcomes according to VARC-3 criteria.
| N=630 | |
|---|---|
| Overall vascular complications | |
| Minor vascular complication | 14 (2.2) |
| Major vascular complication | 4 (0.6) |
| Primary access site | |
| Minor vascular complication | 13 (2.1) |
| Major vascular complication | 4 (0.6) |
| Secondary access site | |
| Minor vascular complication | 1 (0.2) |
| Major vascular complication | 0 |
| Access-related non-vascular complication | |
| Minor vascular complication | 0 |
| Major vascular complication | 0 |
| New-onset vascular complication – discharge to 30 days | |
| Minor vascular complication | 1 (0.2) |
| Major vascular complication | 0 |
| Data are presented as n (%). VARC: Valve Academic Research Consortium | |
Discussion
In this prospective, multicentre study, an easy-to-implement algorithm for percutaneous closure of large-bore arterial access after TAVI was investigated. The MultiCLOSE algorithm consists of preclosure with 1 or 2 suture-based VCDs and angiographic control via the primary access site with a 6-8 Fr sheath to determine a tailored final vascular closure strategy. Final vascular closure can be obtained by the use of one additional suture- and/or plug-based VCD (Central illustration) or neither. Implementation of the MultiCLOSE algorithm was demonstrated to contribute to a safe and efficacious vascular closure after TAVI, resulting in a major vascular complication rate of less than 1%.
Due to the decreasing insertion profiles of TAV delivery systems, meticulous preprocedural CT-based planning of the TAVI vascular access and ultrasound-guided arterial puncture, TAVI-related vascular complication rates have markedly decreased in the last decade1718. A fully percutaneous TAVI approach has become the first-choice strategy due to superior results as compared to surgical approaches1920. At the same time, patients with extensive calcific iliofemoral disease are nowadays also often treated by percutaneous TF-TAVI, as calcium modification techniques such as intravascular lithotripsy or orbital atherectomy have become available2122. In any scenario, it is important to have a well-considered vascular access and closure strategy with adequate bailout options in order to limit vascular complications, which are associated with significant morbidity and mortality.
The MultiCLOSE vascular closure algorithm was quickly and easily adopted in the 3 centres treating a large, nearly all-comers TF-TAVI cohort and demonstrated high efficacy with low vascular complication rates (minor 2.2%, major 0.6%). This is comparable to and even better than the findings reported in the low-risk TAVI landmark trials56. In the PARTNER 3 Trial, the VARC-2 defined minor and major vascular complication rates were reported to be 4.2% and 2.0%, respectively; whereas in the Evolut Low Risk trial, the major vascular complication rate was 3.8% (minor vascular complications were not reported) – importantly, these outcomes were obtained in highly selected low-risk TAVI populations56. With the implementation of the MultiCLOSE algorithm, the goal was to reduce the incidence of major vascular complications to less than 1% in an all-comers TF-TAVI cohort. This goal was achieved in our study cohort.
The novelty and high efficacy of the MultiCLOSE algorithm is not due to the use of a novel (and often more expensive) VCD, but is due, rather, to the design of a stepwise and versatile algorithm for the percutaneous closure of the primary TAVI access, which can be tailored to the ad hoc requirements of each situation and which integrates a cascade of possible safety nets. The MultiCLOSE algorithm has several important components.
Firstly, a one-frame fluoroscopic image of the needle puncture site is stored immediately after ultrasound-guided arterial puncture. This fluoroscopic image, showing the exact location of the arteriotomy site in relation to the femur head, can be used as a reference image for the possible future deployment of a MANTA device (Figure 2) or for the positioning of a balloon or covered stent, if needed.
Next, a short 6-8 Fr sheath is reinserted over a stiff guidewire following removal of the large-bore sheath and advancement of the initially deployed ProGlide/ProStyle(s). This particular approach confers several advantages. 1) It allows a safe and easy ipsilateral angiographic control through the 6-8 Fr sheath. In comparison to a more traditional approach with control angiography from a contralateral femoral or radial secondary access, this strategy is easier and helps to save time, contrast and radiation exposure. 2) The operator has better tactile feedback when advancing and pushing the ProGlide/Prostyle knot(s) towards the arterial vessel wall thereby touching the small-calibre sheath; this prevents unintentional vascular damage and is particularly useful in the challenging subset of obese patients. 3) Based on the angiography, the MultiCLOSE algorithm enables a tailored final vascular closure strategy depending on the degree of contrast extravasation beside the 6-8 Fr sheath. In a majority of cases (93%), an additional Angio-Seal was used in order to achieve instant, complete haemostasis. The efficacy of such a combined suture- and plug-based vascular closure after TAVI has been shown previously by Costa et al (2021), who reported minor and major vascular complication rates of 2.4% and 1.6%, respectively, in a propensity score-matched population14. However, instead of an upfront combined strategy of both a suture- and plug-based VCD, the MultiCLOSE algorithm allows for a more versatile and situation-tailored approach in which either no additional VCD (in case of “pinching” or stenosis of the artery) or an additional Angio-Seal, ProGlide/ProStyle, or MANTA VCD can be used, thus adjusting to the degree of residual contrast extravasation at control angiography. In case of a challenging vascular closure, the MultiCLOSE algorithm also offers a cascade of safety nets: the operator can first opt to deploy an additional ProGlide/ProStyle in case of moderate contrast extravasation, followed by a new ipsilateral control angiography and final vascular closure with a plug-based VCD. 4) Finally, by reinserting a 6-8 Fr sheath, the stiff guidewire can be kept in place without interference with the sutures. This guarantees vascular access in case of complete VCD failure and the subsequent need for MANTA or reinsertion of a large-bore sheath.
Using the MultiCLOSE algorithm, successful vascular closure with complete haemostasis was achieved in 616 patients (98%). In the remaining 14 patients (2%), there was need for an additional bailout strategy due to ongoing bleeding, which mostly consisted of placement of a covered stent (N=12) at the level of the TAVI primary access site. Only one patient required surgical vascular repair; vascular access via the primary access site was not possible, and the lesion could not be crossed via a secondary contra- or ipsilateral approach.
Taken together, we can conclude that the MultiCLOSE vascular closure algorithm is easy to implement and that it contributes to a safe and efficacious percutaneous vascular closure after TAVI, resulting in a low major vascular complication rate (<1%). The use of percutaneous bailout strategies is relatively rare; however, it is strongly recommended to be prepared for this eventuality by measuring the arterial puncture site’s dimensions at the preprocedural CT analysis and having the correctly sized balloons and stents available in the intervention room. It is of critical importance to have zero tolerance for residual bleeding or “oozing” at completion of the procedure, especially when seeking to adopt an early discharge policy after TAVI. In this study, we demonstrate that the implementation of the MultiCLOSE vascular closure algorithm helps to obtain instant, reliable and durable complete haemostasis following percutaneous TF-TAVI.
Finally, this study does not provide an answer to the question of whether vascular preclosure is more efficient when using one or two ProGlide/ProStyle(s). However, we did observe an increased use of only one preclosure device over the time period of this study. The decision to use one or two ProGlide/ProStyle(s) was left to the discretion of the operator and is a rather subjective decision. In patients with a straightforward vascular access (non-obese, single puncture, ≤mild artery calcifications) and good tactile feedback during deployment of a first ProGlide/ProStyle, most operators nowadays will not use a second preclosure device. In Supplementary Figure 1, we demonstrated similar vascular complication rates when using single versus double ProGlide/ProStyle preclosure. However, patient selection bias cannot be excluded, and therefore, future studies will be needed to shed light on this topic.
Central illustration. MultiCLOSE algorithm for closure of large-bore transfemoral access in TAVI. The findings in the TAVI-MultiCLOSE study demonstrate the safety and efficacy of a new and easy-to-implement algorithm for the percutaneous closure of large-bore arterial access after TAVI, offering the TAVI operator a multitude of safety nets, resulting in a low vascular complication rate. TAVI: transcatheter aortic valve implantation; VCD: vascular closure device
Limitations
This was a single-arm, observational study conducted in three hospitals; to determine the true clinical benefit of the MultiCLOSE algorithm for the reduction of TAVI-related vascular complications, a randomised controlled study is needed. Patients with severe peripheral arterial disease undergoing TF-TAVI were excluded from this study, as these patients were treated by intravascular lithotripsy-assisted TF-TAVI with use of a contra- or ipsilateral safety wire. However, this study did include all other consecutively treated TF-TAVI patients (95-100% of all-comers) in whom this MultiCLOSE vascular closure algorithm was used, and there were no missing data at follow-up.
Conclusions
The findings in this real-world TAVI-MultiCLOSE study demonstrate the safety and efficacy of a new and easy-to-implement algorithm for percutaneous closure of large-bore arterial access after TF-TAVI, offering the TAVI operator multiple levels of safety nets, resulting in a major vascular complication rate of less than 1%.
Impact on daily practice
Vascular complications after large-bore transfemoral (TF) access in transcatheter aortic valve implantation (TAVI) are associated with significant morbidity and mortality. The novel, stepwise MultiCLOSE vascular closure algorithm involves the reinsertion of a 6-8 Fr sheath following an initial closure with one or two suture-based vascular closure devices (VCDs). This provides the opportunity to perform a quick and easy angiographic control and tailor the final vascular closure with either an additional suture- or plug-based VCD, or neither of these. Use of the MultiCLOSE algorithm was demonstrated to contribute to an easy, safe, efficacious and durable vascular closure after TF-TAVI with multiple levels of safety nets, resulting in a major vascular complication rate <1%.
Conflict of interest statement
G. Bieliauskas, L. Sondergaard, and O. De Backer received institutional research grants and consulting fees from Abbott. G. Tirado-Conte holds a research-training contract with ‘Rio Hortega’ (CM21/00091) from the Spanish Ministry of Science and Innovation (Instituto de Salud Carlos III). The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. No contrast extravasation with direct right femoral angiography through a 6 Fr sheath over a 0.035” stiff guidewire after removal of the large-bore introducer sheath.
Moving image 2. Mild contrast extravasation with direct left femoral angiography through a 6 Fr sheath over a 0.035” stiff guidewire after removal of the large-bore introducer sheath.
Moving image 3. Moderate contrast extravasation and mild narrowing of the right common femoral artery with direct angiography through a 6 Fr sheath over a 0.035” stiff guidewire after removal of the large-bore introducer sheath.
Moving image 4. Severe contrast extravasation and mild narrowing of the left common femoral artery with direct angiography through a 6 Fr sheath over a 0.035” stiff guidewire after removal of the large-bore introducer sheath.