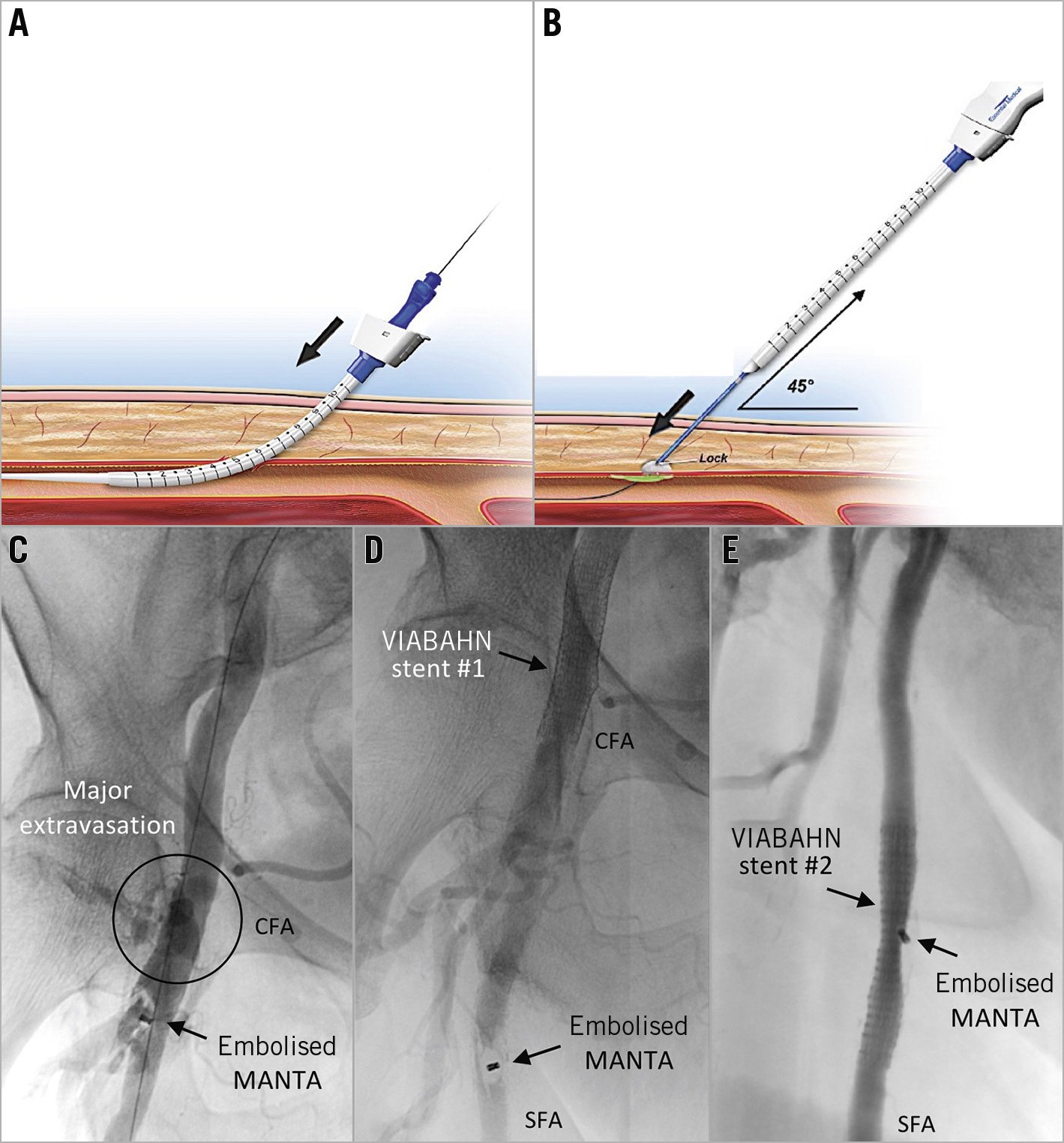
Figure 1. Percutaneous management of an embolised MANTA. A) & B) Working mechanism of the MANTA closure device. C) The embolised device and the active contrast extravasation from the arteriotomy wound. D) The further embolised device and successful haemostasis. E) The stabilised device with minimal residual stenosis.
A 74-year-old female with severe aortic valve stenosis was offered transfemoral transcatheter aortic valve implantation (TAVI) due to comorbidities and surgical risks. After an uneventful TAVI, closure of the right femoral arteriotomy was attempted with an 18 Fr MANTA™ vascular closure device (Essential Medical Inc., Exton, PA, USA). This novel closure device consists of a resorbable intravascular toggle and an extravascular haemostatic collagen pad. During application, the collagen pad is gently pushed towards the vessel wall with a pusher and kept in place by a stainless steel suture lock – the only radiopaque component (Figure 1A, Figure 1B).
Initially, vascular closure seemed successful; however, major bleeding occurred approximately 10 seconds after releasing the MANTA device, indicating closure failure. Angiography showed embolisation of the MANTA device distal to the femoral bifurcation, with active contrast extravasation from the arteriotomy wound (Figure 1C). Because of major bleeding, obtaining immediate haemostasis was considered a priority. A 0.018’’ Platinum Plus™ guidewire (Boston Scientific, Marlborough, MA, USA) was introduced via the contralateral side into the superficial femoral artery (SFA). A self-expanding VIABAHN® stent graft (W.L. Gore & Associates, Flagstaff, AZ, USA) was deployed across the arteriotomy. Haemostasis was obtained and confirmed by angiography. Following these interventions, the MANTA device embolised further distally into the SFA (Figure 1D). Different options (percutaneous intervention vs. vascular surgery) were discussed. Considering the patient’s high surgical risk profile, the consensus was to attempt endovascular repair. A second VIABAHN stent was deployed across the MANTA device, catching and pressing it between the endothelium of the SFA and the covered stent. After optimising stent expansion by post-dilatation, angiography confirmed restoration of flow with minimal residual stenosis (Figure 1E). The patient remained asymptomatic and free from limb ischaemia.
Clearly, compared with surgical repair plus embolectomy, the two covered stent grafts came with an additional cost of approximately 4,000 euros. However, this percutaneous, transcatheter bail-out approach resulted in prevention of a major vascular complication, a vascular surgery under general anaesthesia and a prolonged hospitalisation. The patient was already mobile six hours after the procedure and was discharged uneventfully two days after TAVI. At three-month control, duplex ultrasound showed two patent covered stents and a functionally insignificant residual stenosis.
Retrospectively, excessive manual compression (for “track oozing”) after cutting the MANTA connecting suture could have been the root cause of this complication. Retaining the suture until achieving complete haemostasis would have prevented the MANTA device from embolising. Moreover, if distal embolisation of the MANTA device does occur, endovascular bail-out management of this complication is safe and efficient.
Guest Editor
This paper was guest edited by Alec Vahanian, MD, PhD; Department of Cardiology, Hôpital Bichat-Claude Bernard, and University Paris VII, Paris, France.
Conflict of interest statement
The authors have no conflicts of interest to declare. The Guest Editor is a consultant for Edwards Lifesciences.