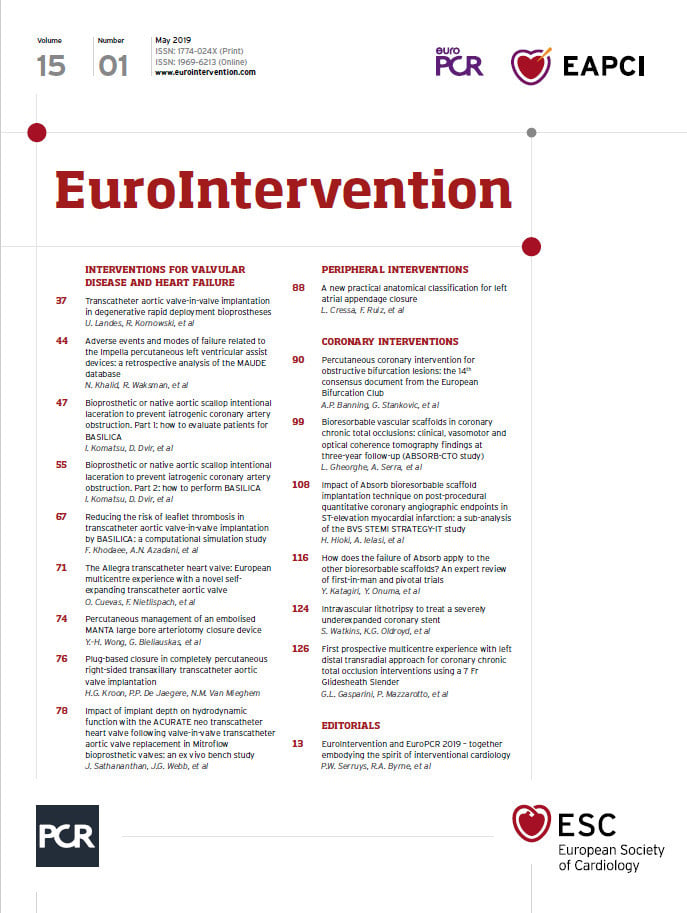
The year 2019 has ushered in new insights concerning transcatheter aortic valve implantation (TAVI). We learnt that this treatment could be equal or even superior to surgery in low-risk patients in terms of mortality, stroke, rehospitalisation and bleeding1,2. This reflects the improvement observed since the first-in-man case in 2002. We have witnessed a constant evolution in the devices utilised with better profiles, repositionability, more stable deployment, sealing features and a wider range of treatable annuli3. Various aspects of the procedure have also evolved during the last decade including (non-exhaustively) the use of cerebral protection devices, radial artery as the accessory access site and pacing through the left ventricle wire4.
TAVI-related complications have improved over time thanks to refinements in technology and the growing experience of operators. One of the aspects of the procedure that has remained immutable is vascular closure devices (VCD) for the main arterial access. Prostar® and ProGlide® (Abbott Vascular, Santa Clara, CA, USA) have been extensively used, despite their inherent limitations, because there was no alternative. Efforts have been made to understand which of them was the most efficient, without clear conclusions5. In the PRAGMATIC initiative, vascular complications were mainly driven by the failure of these closure devices6. We all agreed that improvements were needed in this regard. The MANTA™ vascular closure device (Essential Medical Inc., [now Teleflex], Morrisville, NC, USA) was recently introduced and has rapidly gained interest in a number of European centres. It consists of a bioresorbable toggle and a large collagen plug7. Low rates of vascular complications and bleeding were reported with this novel VCD8. Propensity-matched analyses demonstrated lower major vascular complication rates with MANTA as compared to ProGlide in patients undergoing TAVI9,10. MANTA seems to be an improvement compared with the historical VCD utilised so far. Apart from its efficiency in preventing major vascular complications, what may strike one is its ease of use, with a reasonably short learning curve and reproducible haemostatic and angiographic results.
However, as no device is perfect, we need to improve our understanding about its real performance in large-scale daily practice, its scope of application, limitations and potential complications. Personally, I would use the MANTA as a bail-out tool for torrential bleeding post failure of preclosure with suture-based devices. Ali and colleagues recently reported a similar case11. Echographic guidance could be of tremendous help in such rescue situations, in order to confirm the position of the toggle within the common femoral artery before deployment of the collagen plug (Figure 1).

Figure 1. Echographic identification of the location of the MANTA toggle within the arterial lumen (yellow arrow) before deployment of the collagen plug.
In this issue of EuroIntervention, two reports answer important questions we may have concerning this novel VCD. Kroon et al12 demonstrate for the first time the successful use of MANTA for a fully percutaneous right axillary TAVI.
The transaxillary approach has been explored since the early days of TAVI because of its similarity, in terms of outcomes and recovery, with transfemoral procedures. This access route has even become the first alternative to transfemoral TAVI, as compared to apical or direct aortic techniques13. Right axillary TAVI being technically more challenging than left access, partly because of the vascular tortuosity which has to be overcome, securing the arteriotomy closure is of paramount importance for a fully percutaneous approach. This report from Kroon et al is reassuring in this regard. A stepwise approach has to be applied but the potential superiority of MANTA for haemostasis over the previously available VCD could be an asset for the right axillary technique.
As no VCD is 100% efficient, besides this exciting expansion of the indication for MANTA, Wong et al14 describe a potential complication that may occur and the way to use it as a bail-out tool.
The team discusses the potential reason for the occurrence of this event and its prevention. It reminds us that this closure device can lead to potential complications inherent to plug-based platforms. Given the dreadful impact of vascular complications and bleeding on survival, understanding the optimal use of MANTA and the prevention/rapid treatment of related vascular complications provides important information for the medical community. Both teams should be congratulated for their contributions that clearly improve our knowledge about the MANTA VCD. Have a good read!
Conflict of interest statement
The author has no conflicts of interest to declare.