Abstract
Aims: Although ischaemia-induced QRS complex changes have been described previously, their relation with reperfusion status is not clear. We aimed to investigate the relation of QRS duration with reperfusion at tissue level compared to myocardial blush in patients with acute myocardial infarction who underwent successful primary percutaneous coronary angioplasty.
Methods and results: One hundred and forty-eight patients were enrolled. Based on the post-angioplasty myocardial blush grade (MBG), patients were divided into reperfusion (grades 2 and 3) and impaired reperfusion (grades 0 and 1) groups. Although the two groups did not differ in terms of admission QRS duration (81±17 vs. 79±15 msec, p=0.473), the patients in the impaired reperfusion group had a significantly longer QRS duration both at immediate post-angioplasty (78±18 vs. 68±17 msec, p=0.001) and at the 60th minute ECG (77±17 vs. 60±17 msec, p<0.001). Patients in the impaired reperfusion group revealed significantly less narrowing of QRS duration in the post-angioplasty 60th minute ECG (6±5 vs. 20±5 msec, p<0.001) when compared to the patients in the reperfusion group. After adjusting all variables, QRS narrowing in the 60th minute ECG was determined as an independent electrocardiographic predictor of reperfusion (OR:1.39, 95% CI: 1.25-1.54, p<0.001).
Conclusions: We demonstrated that QRS duration is a strong indicator of myocardial reperfusion status.
Introduction
Primary percutaneous coronary intervention (PCI) is an effective method in restoration of the flow in the infarct-related artery (IRA) in the great majority of patients with acute ST-segment elevation myocardial infarction (STEMI). Nevertheless, the patency of the IRA does not guarantee the salvage of the myocardium under risk of ischaemia. Microvascular no-reflow is defined as inadequate myocardial perfusion through a given segment of the coronary circulation without angiographic evidence of mechanical vessel obstruction1. It is observed in more than 30% of patients with acute myocardial infarction treated with fibrinolysis or catheter-based PCI2,3.
The changes in the QRS complex during ischaemia have been described in animals as well as in humans4,5. Moreover, it was shown that QRS prolongation after STEMI was associated with higher mortality in acute and chronic phases6,7. In patients with STEMI, QRS prolongation, in the absence of bundle branch blocks, was considered mainly a dynamic phenomenon likely to be improved by successful reperfusion7. However, there are no data regarding whether the change in QRS duration following angioplasty may reflect reperfusion status at tissue level.
Although ST-segment elevation resolution for assessment of reperfusion status is in widespread use in patients with acute STEMI, there are few reports evaluating the relation of QRS duration with myocardial reperfusion. Thus, our objective in this study was primarily to evaluate if there is any change in QRS duration signifying successful myocardial reperfusion following successful primary angioplasty.
As a surrogate to tissue level reperfusion, we used the angiographic myocardial blush grade, which was shown in previous reports to be a reliable index of microvascular integrity8-10.
Methods
One hundred and sixty-one patients (mean age 58±12 years, 82% male) of any age who presented with STEMI within 12 hours (h) from the onset of symptoms, and were admitted to our emergency department between December 2008 and September 2010 and underwent successful primary angioplasty with achievement of TIMI-3 flow in IRA, were enrolled in the study. STEMI was defined as typical chest pain of more than 30 minutes duration with ST-segment elevation >1 mm in at least two consecutive precordial or inferior leads. Patients who were in shock, who had electrolyte abnormalities, needed a pacemaker, had left ventricular hypertrophy, bundle branch blocks and severe ST-segment elevation obscuring J point identification were excluded from the study. Data from 13 patients who fulfilled one of the above-mentioned exclusion criteria were not taken into account. This report was based upon the data obtained from the remaining 148 patients.
All patients received 300 mg acetylsalicylic acid at the emergency department if they had not already received it during transport to the hospital. Following coronary angiography, if the coronary anatomy was found suitable for angioplasty, 600 mg of clopidogrel loading was administered and primary PCI was performed using conventional methods. Written informed consent was obtained from all patients by a physician before cardiac catheterisation. Decision-making on adjuvant tirofiban administration and PCI strategy, including the use of stents, was left to the discretion of the individual operator. A bolus dose, adjusted according to body weight, of heparin was administered before coronary intervention.
There are various methods for assessment of myocardial reperfusion. ST-segment resolution and myocardial blush score are the best known and most reliable methods11,12. In our study, we evaluated the myocardial perfusion status using myocardial blush score or perfusion grade. The main reason in choosing the blush score was to detect the role of QRS duration change, a new method, in evaluation of myocardial perfusion status. Furthermore, the blush score is a more useful method of assessing reperfusion status in patients undergoing percutaneous coronary intervention. Two experienced cardiologists blinded to the clinical history and laboratory measurements of the patients graded pre- and post-angioplasty flow in IRA using the Thrombolysis In Myocardial Infarction (TIMI) flow classification13. Primary PCI was considered successful when TIMI-3 flow without significant residual stenosis (>20%) in the IRA was achieved. TIMI myocardial perfusion (TMP) grade was determined by post-angioplasty angiogram by two blinded experienced interventional cardiologists based on the visual assessment of contrast opacification of the myocardial territory subtended by the IRA, as previously described9. A third reader’s opinion was asked in the case of discordance between the two. All operators took the necessary requirements, such as giving enough contrast agent and long angiographic runs (until the opacification disappeared on the angiogram), to assess the blush score accurately. TMP grade was defined as follows: 0=no myocardial blush or contrast density; 1=minimal myocardial blush or contrast density; 2=moderate myocardial blush or contrast density but less than that obtained during angiography of a contralateral or ipsilateral non-IRA; and 3=normal myocardial blush comparable with that obtained during angiography of a contralateral or ipsilateral non-IRA. TMP grades 0 and 1 were taken as indicators of injured microvasculature (impaired reperfusion) and TMP grades 2 and 3 as indicators of preserved microvasculature (reperfusion) as previously described9.
Electrocardiography
On admission, for each patient, a 12-lead ECG with a paper speed of 50 mm/sec and amplification of 10 mm/mV was recorded by using the Cardiofax ECG-9132K (Nihon Kohden, Tokyo, Japan) machine; it was noted immediately after successful angioplasty and 60 minutes later. In the present study, all measurements were obtained from infarct-related artery leads. For each patient, QRS duration was measured manually with the help of a calliper and a magnifying lens (to diminish the effect of the ST deviation on the measurement of accurate QRS duration) by two of the investigators who were unaware of all clinical and angiographic data. The average value of the measurements obtained by the two investigators was taken into account for statistical analysis in each patient. Change in QRS duration was calculated by subtracting post-angioplasty QRS duration from pre-angioplasty QRS duration.
Statistical analysis
Categorical variables were expressed as percentages and evaluated with a Chi square test or Fisher’s exact test. Continuous variables were presented as mean±SD and were compared by Student’s t-test or Mann-Whitney U test. The Spearman correlation coefficient was calculated to evaluate the association between two continuous variables. For factors which were found to be related to reperfusion status in univariate analysis, regression analyses were performed to determine their impact independently. In order to determine the predictive impact of post-angioplasty QRS duration narrowing on assessment of reperfusion status, receiver operating characteristics (ROC) analyses was performed. Best cutoff value was determined and at that point sensitivity and specificity were determined. The p<0.05 values were accepted as statistically significant. All analyses were performed using SPSS 11.5 (SPSS Inc., Chicago, IL, USA).
Results
Grade 2/3 TMP was detected in 102 (69%) patients (25 patients with grade 2 and 77 patients with grade 3) and these patients constituted the reperfusion group. The remaining 46 (31%) patients, who had grade 1/2 TMP (14 patients with grade 1 and 32 patients with grade 0), formed the impaired reperfusion group. The baseline clinical and angiographic characteristics of the two groups were presented in Table 1.
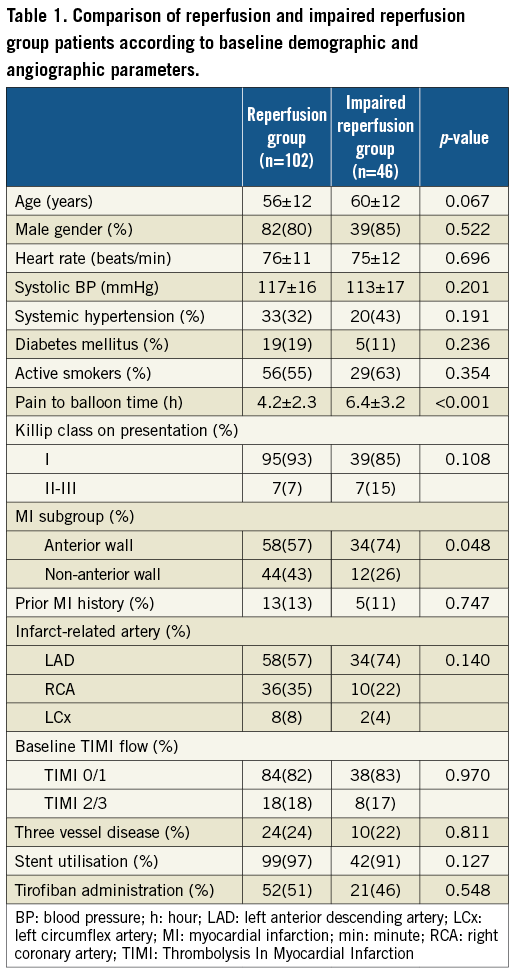
At least one stent was placed in 95% of patients during PCI. At the operator’s discretion, tirofiban was administered periprocedurally in 49% of all patients.
The two groups were similar in terms of age, gender, smoking habits, history of hypertension and diabetes mellitus (p>0.05). Heart rate, blood pressure and Killip class of patients on admission also did not differ between the groups. In the impaired reperfusion group, patients were more likely to have anterior myocardial infarction (MI) (74% vs. 57%, p=0.048). We detected significant differences between the groups in terms of pain to balloon time. The patients in the impaired reperfusion group had longer pain to balloon interval (6.4±3.2 vs. 4.2±2.3 h, p<0.001) compared to patients in the reperfusion group.
Electrocardiographic findings
The intra- and interobserver variability was very low (<2% and <4%, respectively). When we compared the groups in terms of electrocardiographic parameters (Table 2), we did not detect significant differences between the groups regarding the total amount of ST-elevation and the sum of ST depressions on admission. The two groups also had similar QRS duration on admission (81±17 vs. 79±15 msec, p=0.473, in the impaired reperfusion and reperfusion groups, respectively). On correlation analysis, pre-angioplasty QRS duration was found to be correlated positively with age (r=0.211, p=0.010) and pain to balloon interval (r=0.225, p=0.006). When we compared QRS durations on the post-angioplasty ECG, QRS duration was found to be longer in the impaired reperfusion group compared to the reperfusion group, at both the immediate ECG (78±18 vs. 68±17 msec, p=0.001) and the 60th minute ECG (77±17 vs. 60±17 msec, p<0.001) post-angioplasty.
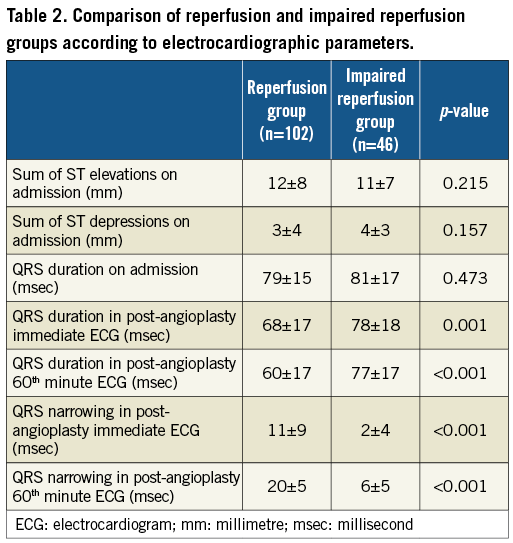
When the amount of change in QRS duration was taken into account, a significant difference was detected between the two groups post-angioplasty at both the immediate (11±9 vs. 2±4 msec, p<0.001) and the 60th minute (20±5 vs. 6±5 msec, p<0.001) ECG. The mean change in QRS duration was more prominent in the 60th minute ECG compared to the immediate post-angioplasty ECG (15±9 vs. 8±9 msec, p<0.001). The distribution of the amount of change in the post-angioplasty 60th minute QRS duration according to the reperfusion status of patients is presented in Figure 1. On correlation analysis, age (r=-0.167, p=0.042) and pain to balloon time (r=-0.341, p<0.001) appeared to be significantly correlated with QRS narrowing at the post-angioplasty 60th minute ECG.
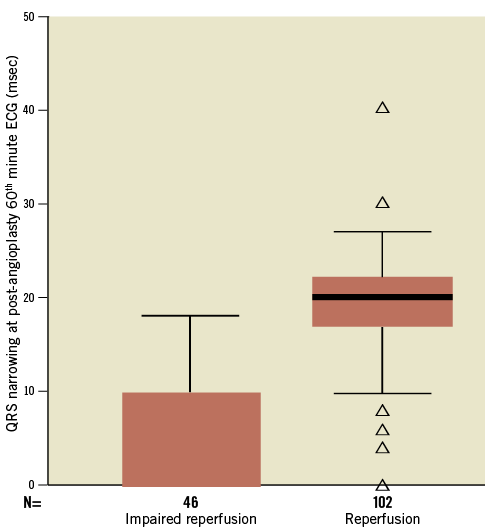
Figure 1. Box plot graph illustrating the distribution of amount of change in QRS duration at post-angioplasty 60th minute ECG according to reperfusion status of patients.
We performed correlation analysis utilising the individual myocardial blush grades as a variable to delineate the association of the 60th minute QRS narrowing with reperfusion at the tissue level better, and detected a strong positive correlation between the 60th minute QRS narrowing and TMP (r=0.815, p<0.001) while there was no correlation between admission QRS duration and MBG (r=–0.073, p=0.376). The distribution of QRS narrowing at the 60th minute ECG among subgroups according to TMP grades is shown in Figure 2.

Figure 2. Box plot graph illustrating the distribution of QRS narrowing at 60th minute ECG among subgroups according to TMP grade.
The regression analysis including age, pain to balloon interval, MI subgroup, QRS duration on admission, change in the QRS duration variables at the immediate and the 60th minute ECG post-angioplasty was performed to understand the independent impact of individual variables that were found to be related to myocardial reperfusion in univariate analysis and the change in QRS duration at the post-angioplasty 60th minute ECG (ß: 0.326, OR:1.39, 95% confidence interval [CI], 1.25-1.54, p<0.001) as an independent predictor of myocardial reperfusion.
ROC analyses were performed to determine the best cutoff value of the post-angioplasty 60th minute QRS duration narrowing for predicting reperfusion. The area under the ROC curve with the post-angioplasty 60th minute QRS duration narrowing was used to detect reperfusion and an area of 0.96 was found (95% CI: 0.93-0.99, p<0.001). In other words, a QRS duration narrowing of 11 msec at the post-angioplasty 60th minute was determined to be the best discriminating value for reperfusion assessment. A post-angioplasty 60th minute QRS duration narrowing of an 11 msec value had a sensitivity of 92% and specificity of 89% in predicting reperfusion after primary angioplasty.
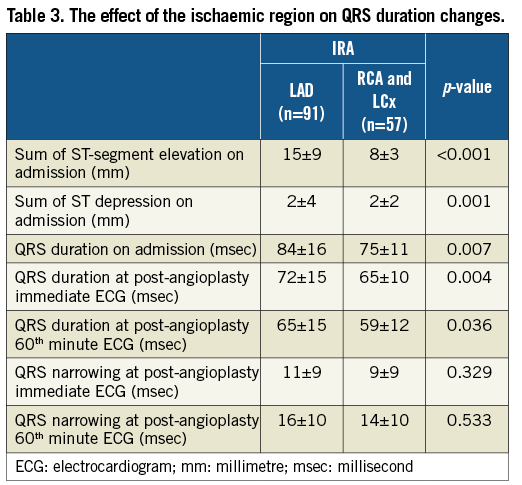
In the subgroup analysis, patients were divided into two subgroups according to infarct-related artery (IRA) to assess the effect of the region under ischaemia. The sum of the ST-segment elevation in patients in whom the left anterior descending artery (LAD) was the IRA was higher than in patients in whom the left circumflex (LCx) or right coronary artery (RCA) was the IRA (15±9mm vs. 8±3 mm, p<0.001). QRS duration on admission was higher in the LAD group when compared to the RCA and LCx groups (84±16 msec vs. 75±11 msec, p=0.007). Similarly, QRS duration just after angioplasty (72±15 msec vs. 65±10 msec, p=0.004 ) and at the 60th minute post-angioplasty was higher in the LAD group (65±15 msec vs. 59±12, p=0.036). However, the amounts of QRS narrowing just after angioplasty (p=0.329) and the 60th minute post-angioplasty (p=0.533) were similar in both groups. The effect of the ischaemic region on QRS duration changes is shown in Table 3.
Discussion
With this report, the first in the literature to our knowledge, we showed the association of QRS narrowing on post-angioplasty 60th minute ECG with adequate myocardial reperfusion in patients with acute STEMI treated with primary angioplasty.
Several mechanisms for intermediate QRS prolongation have been proposed during coronary occlusion. Experimental studies have reported that QRS prolongation is associated with Purkinje-ventricular conduction delay caused by myocardial ischaemia14-17. In our study the correlation between admission QRS duration and ischaemia duration further supports the idea of ischaemia as a mechanism of QRS prolongation.
Impaired myocardial perfusion has been shown to be a major predictor of adverse outcomes in patients undergoing reperfusion therapy and several modalities have been suggested to assess myocardial reperfusion3,8,18-20 in patients with acute MI. In our study, reperfusion was evaluated by means of TMP grade, myocardial blush (which was previously shown to be related to enzymatic infarct size), the extent of ST-segment elevation resolution, left ventricular function, long-term mortality8,9, and degree of myocardial salvage assessed by scintigraphy21.
In the present study, longer ischaemia duration was detected as a predictor of impaired reperfusion, as previously described. The association of late reperfusion with impaired reperfusion, larger infarct size and higher one-year mortality even after optimal primary angioplasty has been reported previously22. The fact underlying this association is believed to be the result of extensive microvascular damage, which is proportional to ischaemia duration8,23. Furthermore, with delay in reperfusion, thrombus gets older and more organised resulting in a higher incidence of distal microembolisation and poor myocardial perfusion24.
Interpretation of ECG findings
Our findings of significantly longer QRS duration after angioplasty and lesser narrowing detected on post-angioplasty 60th minute ECG, in the impaired reperfusion group compared to the normal reperfusion group, might have resulted from the dynamic nature of changes in QRS duration during ischaemia and reperfusion, suggesting prolongation of QRS duration during ischaemia and resolution of this prolongation following successful reperfusion at cellular level. In accordance with our findings, there are many reports showing the association of ischaemia with QRS duration changes. In a recent report by Weston et al5, conducted on dogs undergoing experimental coronary occlusion, QRS prolongation following coronary occlusion and its adverse effect on myocardial salvage has been shown. Similar findings were described in humans as well. In the study conducted by Cantor et al25 QRS prolongation of ≥3 msec developed in 42 of 51 patients undergoing percutaneous transluminal coronary angioplasty and was greater with occlusion of proximal and middle segments of major arteries. It was reported that exercise caused intermediate QRS prolongation proportional to the number of diseased vessels in patients with coronary artery disease while QRS duration decreased with exercise in patients with normal coronary arteries26. Furthermore, transient QRS prolongation measured by the signal-averaged electrocardiogram during typical angina was demonstrated in a majority of patients with documented coronary artery disease27.
The alterations in the morphology of the QRS complex typically have been considered indicative of necrosis among patients with acute ischaemic syndromes5. However, recent data suggest that ischaemia-related QRS prolongation on admission ECG may be a reflection of extensive ischaemia and a poor metabolic state rather than of myocardial fibrosis, which is associated with persistent QRS prolongation7. It is therefore logical to think that ischaemia-related QRS prolongation can be reversed by restoration of flow. Our finding of more significant narrowing in QRS duration in the reperfusion group is consistent with the dynamic nature of change in QRS duration showing resolution after successful reperfusion. The correlation we observed between QRS narrowing and ischaemia duration is also supported by the dynamic nature of QRS changes. Furthermore, in subgroup analysis, having higher QRS duration on admission in patients in whom the LAD was the IRA, rather than patients in which the LCx or RCA was the IRA, also demonstrates the effect of the amount of region under ischaemia. Patients with anterior wall myocardial infarction had higher QRS duration at both –just after and at the 60th minute ECGs– than other walls. The finding of a strong positive correlation between the 60th minute QRS narrowing and TMP grade suggests a closer association of QRS duration changes with the degree of cellular reperfusion. Similar to our findings Tsukahara et al7 reported QRS duration normalisation within 24 hours following successful angioplasty in 79% of patients having intermediately prolonged QRS duration (≥120 msec) on admission. However, they defined successful reperfusion based on TIMI flow at the end of angioplasty and they did not have an impaired reperfusion. In a recent study, we evaluated the role of QRS duration in prediction of reperfusion in patients with acute STEMI treated by fibrinolytic therapy and found greater resolution of QRS duration in reperfused patients assessed by TMP28. Unlike the present study, baseline QRS duration was found to be another determinant of reperfusion.
Study limitations
This was a small-sized study and there was not a clear standardised method for the measurement of QRS duration, which has a normal range of 60-80 msec. In the presence of abnormalities of both waveforms, it is often difficult to determine precisely the junction between the end of the QRS complex and the beginning of the ST-segment. Another drawback of the current study comes from the manual measurement of QRS duration. The use of automated or computerised ECG measurement techniques might help in the standardisation of QRS duration measurements in future studies. We used TMP grade as a surrogate of tissue reperfusion. Using another modality to define reperfusion could change the distribution of patients among the reperfusion or impaired reperfusion groups. In addition, this study included patients reperfused by percutaneous coronary intervention. Whether our findings can be extrapolated to a fibrinolytic treatment group remains unexplored.
Conclusion
In the present study, we demonstrated that longer QRS duration and less narrowing of QRS duration at post-angioplasty in the impaired reperfusion group were reflections of the dynamic nature of ischaemia and the reperfusion process in acute myocardial infarction.
Conflict of interest statement
The authors have no conflict of interest to declare.