Abstract
Aims: To evaluate the clinical importance of the ST peak phenomenon during primary percutaneous coronary intervention (PCI) in patients with ST-segment elevation myocardial infarction (STEMI).
Methods and results: Continuous ST monitoring was performed in 942 STEMI patients from arrival until 90 minutes after revascularisation. ST peak was defined as ≥1 mm increase in the ST-segment during PCI compared with the ST elevation before intervention. ST peak was observed in 26.9% of patients. During median follow-up of 4.1 years, 20.7% of patients experienced a major adverse cardiac event (MACE). ST peak was associated with higher rates of mortality (13.4% versus 9.3%; p=0.044), admission for heart failure (10.6% versus 5.2%; p=0.002) and MACE (26.9% versus 18.2%; p=0.002), but not reinfarction (7.1% versus 5.2%; p=0.14). In two different Cox regression analyses, adjusting for predictors of MACE and ST peak including ST resolution and epicardial flow, ST peak remained significantly associated with MACE: adjusted hazard ratio (HR) 1.40 (95% confidence interval [CI] 1.01-1.95) and 1.41 (95% CI: 1.02-1.96).
Conclusions: In the largest study hitherto evaluating the ST peak phenomenon during primary PCI, we demonstrated that ST peak is a strong predictor of adverse long-term outcome and provides independent prognostic information beyond that provided by ST resolution and epicardial flow.
Introduction
Patients with ST-segment elevation myocardial infarction (STEMI) treated with primary percutaneous coronary intervention (PCI) may, in spite of optimal treatment, still have impaired microvascular perfusion or reduced epicardial flow and this may lead to adverse outcomes1-5. The myocardial perfusion can be assessed by traditional ST-segment resolution after the procedure, which is widely accepted as a prognostic predictor in patients with STEMI treated with primary PCI6-13. However, this information cannot be used as guidance for the PCI operator. Thus, with the increasing use of primary PCI, early recognition of impaired reperfusion during the procedure is relevant. Despite final ST-segment resolution, patients treated with primary PCI may transiently experience increased ST-segment elevation during reperfusion (ST peak). The pathophysiological explanation for ST peak during primary PCI is unknown, but might be associated with suboptimal myocardial reperfusion caused by distal embolisation, reduced epicardial flow, reperfusion injury and microvascular dysfunction. In the era of thrombolysis, an early increase in the ST segment after medical treatment appeared to be related to improved clinical outcome and was thus considered a marker of successful reperfusion14-17. In contrast, an ST peak in patients treated with primary PCI is associated with larger myocardial damage and impaired left ventricular function18-25. However, in most previous studies, the patients were not pre-treated with clopidogrel18,19,21,23, the ECG acquisition was performed using various and fixed intervals following reperfusion18,19,21,23, the patients were restricted to anterior infarct location or culprit lesion in the left descending artery18,19,21,23, to Thrombolysis In Myocardial Infarction (TIMI) flow 0 or 118 or to those who did not achieve complete ST-segment resolution before PCI20. In addition, clinical data are only available from a small pilot study not powered to make firm conclusions on long-term clinical outcome and mortality20. Therefore, the present study evaluated the clinical importance of the ST peak phenomenon in patients treated with primary PCI in a larger cohort of patients with STEMI. Moreover, we related the ST peak phenomenon to the occurrence of slow coronary blood flow, angiographic visible distal embolisation and microvascular function assessed by residual ST-segment elevation and resolution26.
Methods
The patients in this post hoc study were included in three randomised clinical studies: the first compared the effect of distal protection during primary PCI with conventional PCI (n=626)27, the second evaluated mechanical ischaemic post-conditioning against conventional PCI (n=118)28, and in the third study patients were randomised to adjuvant exenatide treatment or placebo in combination with primary PCI (n=387)29. The present study encompasses a clinical outcome analysis and a supplementary angiographic correlation analysis. In the outcome analysis all patients were included, whereas the angiographic analysis was restricted to patients who had quantitative coronary angiographic data available27.
STUDY POPULATION AND TREATMENT
Patients were eligible if they were ≥18 years and presented to the catheterisation laboratory within 12 hours from the onset of a STEMI. An electrocardiogram (ECG) was obtained either in the ambulance or at the referring hospital. STEMI was defined as significant ST-segment elevation measured at the J-point in at least two contiguous leads. The following ST-segment elevation criteria were used: 1 mm ST-segment elevation in the limb lead (II, III and aVF, I, aVL) and V4-V6, and 2 mm ST-segment elevation in V1-V330. There were small differences in the inclusion and exclusion criteria among the three studies. In one study, patients with a total ST-segment elevation of >4 mm in at least two contiguous electrocardiographic (ECG) leads and without excessive tortuosity or heavy calcification were included27. In the two other studies, patients with ST-segment elevation in two contiguous ECG leads of at least 1 mm in II, III, aVF, I, aVL and V4-V6, or 2 mm in V1-V3 were included28,29. Moreover, in one study only patients with TIMI flow grade 0 or 1 were included28. Mutual exclusion criteria were: a history of previous myocardial infarction, culprit lesions in an unprotected left main coronary artery or a saphenous vein graft, gastrointestinal bleeding within one month, pregnancy, known renal failure, and linguistic problems. Moreover, patients were excluded if cardiac biomarkers did not confirm the diagnosis in spite of the above-mentioned ECG changes (aborted STEMI). All patients eligible for primary PCI were pre-treated with aspirin 300 mg orally or 500 mg intravenously, clopidogrel 300-600 mg orally, and unfractionated heparin 10,000 units intravenously, usually administered in the pre-hospital setting or at the referring hospital. On arrival at the catheterisation laboratory the culprit lesion was identified angiographically, and primary PCI was performed as previously described27-29. Glycoprotein IIb/IIIa receptor antagonists were administered at the discretion of the operator if no contraindications were present, and balloon dilatation before stenting was done in all patients. All patients were treated with clopidogrel 75 mg daily for 12 months and aspirin 75 mg daily indefinitely. All patients were informed orally and in writing, and all gave their written consent before inclusion in the three randomised studies. The study was performed according to the Declaration of Helsinki. The Danish National Committee on Biomedical Research Ethics approved the protocol for all studies.
QUANTITATIVE CORONARY ANGIOGRAPHY ANALYSIS
Angiographic lesion characteristics were evaluated using the MEDIS system (Medis medical imaging systems, Leiden, The Netherlands) by independent core laboratory technicians unaware of the treatment sequence.
ST PEAK AND RESOLUTION
A continuous 12-lead ST monitoring was initiated at admission and continued for a minimum of 90 minutes after the primary PCI (LIFEPAK 12; Medtronic Emergency Response Systems, Redmond, WA, USA). The ECG data were analysed blinded to paraclinical data and clinical outcome using dedicated computer software (CODE-STAT Suite version 6.1; Medtronic Emergency Response Systems). In case of at least 0.1 mm changes in the ST segment for 2.5 minutes the software generated a complete 12-lead ECG. The level of ST elevation was measured automatically by a computer at the J-point + 1/16 of the RR interval (STM), also used by the LIFEPAK 12 to register ST-segment deviations. The lead with maximum ST-segment elevation prior to intervention was used to determine baseline ST-segment elevation (mm). The same lead was used to evaluate absolute ST-segment elevation (mm) and achievement of 70% ST-segment resolution at 30, 60 and 90 minutes after wire crossing of the lesion. In the same lead the maximum ST-segment elevation during the primary PCI procedure (from first wire crossing to the last angiogram) was registered, and the ST-segment change during reperfusion was evaluated as the maximum ST-segment elevation during the procedure minus baseline ST-segment elevation. An ST peak was defined as an increase in ST-segment elevation ≥1 mm lasting ≥2.5 minutes. The patients were stratified into two groups according to the presence of significant ST peak. The ST peak was further analysed for duration and absolute increase as well as the relative increase. Complete ST-segment resolution before intervention was defined as no significant ST-segment elevation (<1 or 2 mm depending on ECG lead) at the time of first wire. Anterior infarction was defined as maximum ST-segment elevation in lead V1-4.
CLINICAL STUDY ENDPOINTS
Clinical outcome was assessed as all-cause mortality, cardiac mortality, admission for heart failure and reinfarction. The primary endpoint of this study was the composite of major adverse cardiac events (MACE), defined as death from any cause, reinfarction or hospital admission for heart failure. Mortality events and reinfarction were registered according to previous definitions31. Reinfarction was defined as acute coronary syndrome with a concomitant increase in creatine kinase myocardial band or troponin T. Admission for heart failure was defined as hospital admission owing to peripheral or pulmonary oedema treated with antidiuretics or admission for implantation of a primary prophylactic implantable cardioverter defibrillator. A reviewer blinded to all data including ECG data, angiographic measurements and randomisation carefully evaluated all readmissions during the follow-up period by evaluating all hospital files. This can easily be done in Denmark owing to all inhabitants having a social security number, which is used to register any hospital admittances. There was no difference in the definition of endpoints among the three studies.
STATISTICAL ANALYSIS
All statistical analyses were performed with SPSS software version 20 (IBM Corp., Armonk, NY, USA). A two-sided p-value <0.05 was considered statistically significant. Categorical variables were compared using chi-square or Fisher’s exact test and continuous variables using the Student’s t-test or the Mann-Whitney test, as appropriate. Continuous variables were tested for normality by histograms. To identify the independent predictors for ST peak, a logistic regression analysis was performed including any baseline or angiographic variable with p≤0.10. To evaluate the prognostic importance of ST peak during primary PCI, univariate Cox regression analyses were performed for all primary and secondary clinical endpoints. To identify the independent predictors for MACE, multivariate Cox regression analyses were performed and two models were constructed: model 1 included all variables with a p<0.05 in the univariate analysis and model 2 included any baseline variable with a p≤0.10 for the difference between patients with and without ST peak (Table 1). Due to expected collinearity between achievement of 70% ST-segment resolution at 30, 60 and 90 minutes, only the time point with the highest χ2 value in the univariate Cox regression analysis was used in the multivariate models. If a patient experienced more than one event, the patient was censored at the time of the first event in the analysis of MACE. The Cox regression assumptions were checked for each variable by interaction, variable*variable (linearity - only continuous variable) and visually for proportionality.
Results
A total of 1,131 patients with STEMI were randomised in the three studies. In 151 patients, data (ECG) were missing or the ECG could not be used for ST peak evaluation (e.g., bundle branch block). In an additional 38 patients the ECG STEMI criteria were not met or a myocardial infarction was not confirmed by biomarkers, leaving a total of 942 patients with STEMI to be included. Of these, a total of 253 patients (26.9%) fulfilled the criteria for ST peak during reperfusion whereas 689 (73.1%) did not.
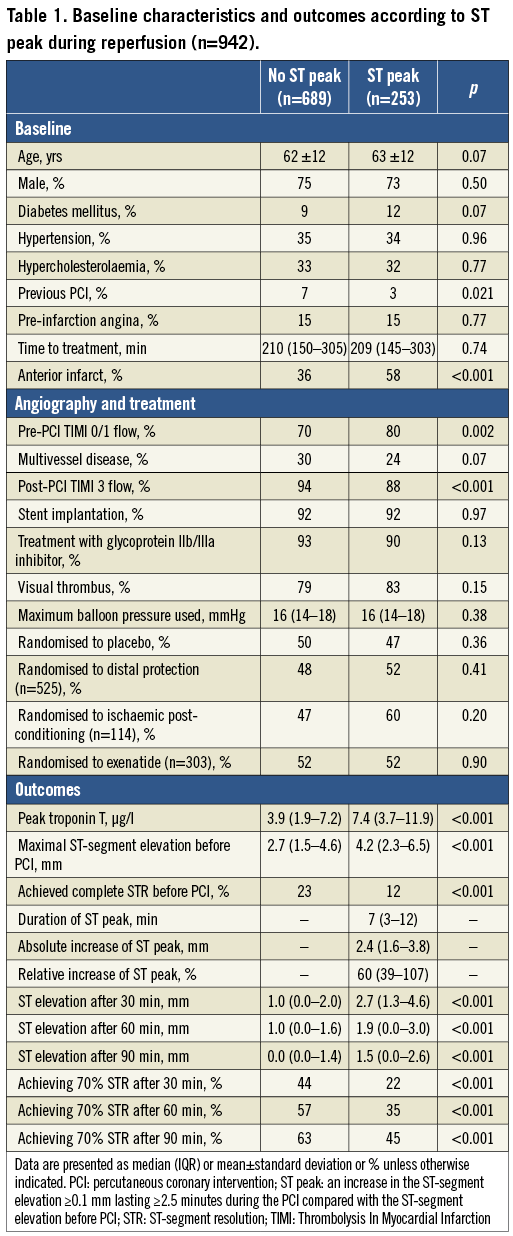
Baseline and angiographic characteristics are shown in Table 1. Diabetes, anterior infarct location and pre-PCI TIMI flow 0/1 were more frequent among patients with an ST peak (Table 1), post-PCI TIMI flow 3 and complete ST-segment resolution before intervention were less frequent, and these patients had a higher baseline and final ST-segment elevation, higher maximal troponin T release and delayed ST-segment resolution (Table 1). On the other hand, a history of previous PCI was rare in patients with an ST peak, and multivessel disease was found less frequently (Table 1).
QUANTITATIVE CORONARY ANGIOGRAPHY
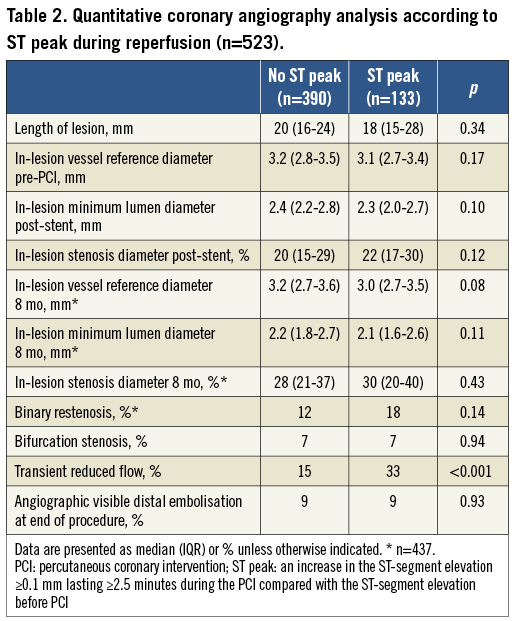
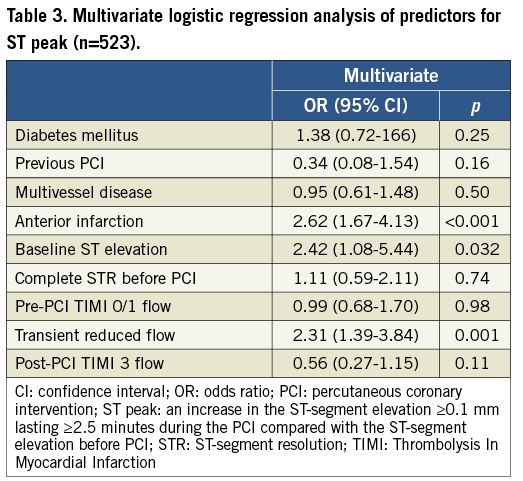
Table 2 shows the quantitative coronary angiography analysis results available in 523 patients (55.4%). Transient reduced flow but not angiographic visible distal embolisation at the end of the procedure differed significantly between the groups (Table 2). In the multivariate logistic analysis only transient reduced flow, anterior infarct location and baseline ST-segment elevation were independent predictors of an ST peak (Table 3).
CLINICAL OUTCOME
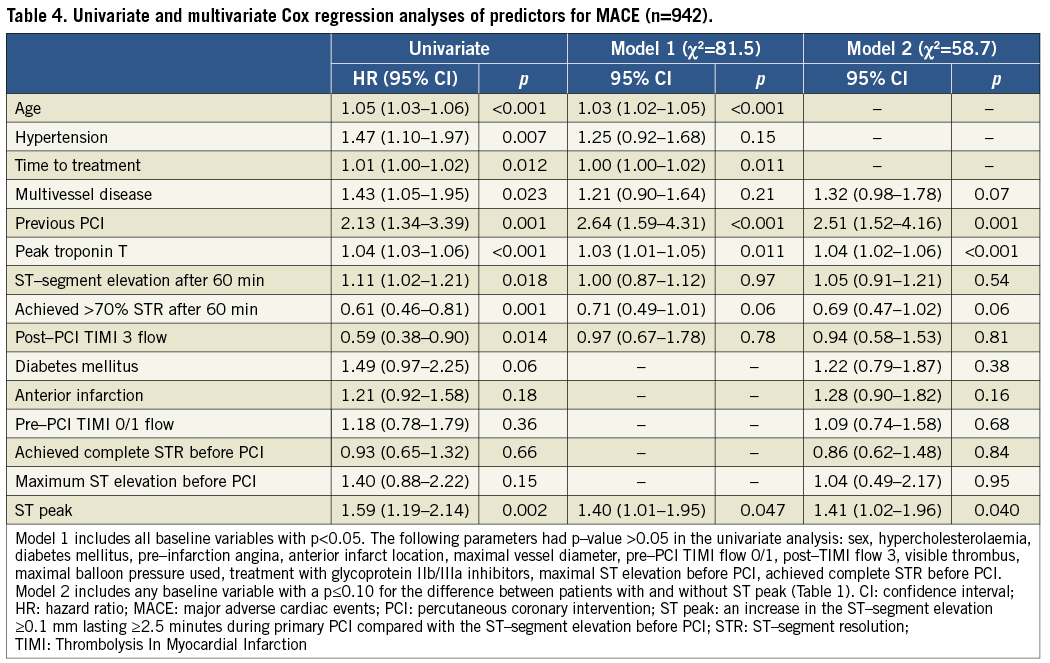
A total of 195 patients (20.7%) experienced a MACE during a median follow-up period of 4.1 years (IQR 2.3-5.8 years). The Kaplan-Meier survival estimates demonstrated a significantly higher MACE rate among patients with ST peak than those without (Figure 1). In the univariate Cox regression analyses, the presence of an ST peak was also significantly associated with higher rates of all-cause mortality, admission for heart failure, and MACE (Figure 2). Insignificant trends were observed for an association between the occurrence of ST peak and rates of cardiac mortality and reinfarction (Figure 2). Adjusting for multiple comparisons by the Bonferroni method, an ST peak remained significantly associated with MACE (p=0.01) and admission for heart failure (p=0.01). In both multivariate Cox regression models, ST peak remained significantly associated with MACE (Table 4). Achievement of 70% (complete) ST-segment resolution at 60 minutes (HR 0.61 [95% CI: 0.46-0.81]; p=0.001; χ2=11.3) was used in the multivariate models since this variable had a higher χ2 value than those at 30 minutes (HR 0.61 [95% CI: 0.44-0.84]; p=0.003; χ2=9.1) and 90 minutes (HR 0.82 [95% CI: 0.61-1.09]; p=0.16; χ2=1.9). Among patients with available quantitative coronary angiography analysis (n=523) an ST peak remained significantly associated with the occurrence of MACE adjusting for transient reduced flow (adjusted HR 1.50 [95% CI: 1.01-2.23]; p=0.044).
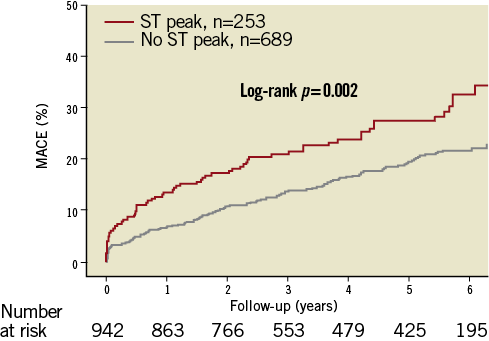
Figure 1. Kaplan-Meier plot showing the difference in MACE between patients with and without ST peak during primary percutaneous coronary intervention for patients with ST-segment elevation myocardial infarction. Statistical comparison by log-rank test. MACE: major adverse cardiac events (all-cause mortality, admission for heart failure, reinfarction); ST peak: an increase in the ST-segment elevation ≥0.1 mm lasting ≥2.5 minutes during the PCI compared with the ST-segment elevation before PCI
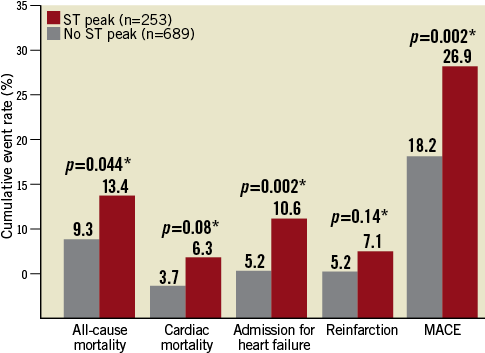
Figure 2. Columns showing the difference in clinical events between patients with and without ST peak during primary percutaneous coronary intervention for patients with ST-segment elevation myocardial infarction. * Statistical comparison by Cox regression proportional hazards analysis. MACE: major adverse cardiac events (all-cause mortality, admission for heart failure, reinfarction); ST peak: an increase in the ST-segment elevation ≥0.1 mm lasting ≥2.5 minutes during the PCI compared with the ST-segment elevation before PCI
SUBGROUP ANALYSIS
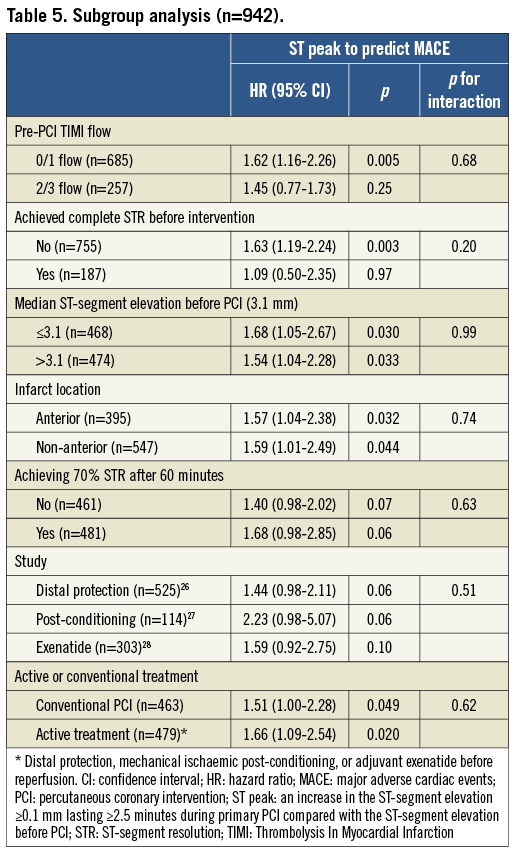
Stratifying patients according to infarct location (anterior and non-anterior), pre-PCI TIMI flow (0/1 and 2/3), final ST-segment resolution or median baseline ST-segment elevation, ST peak and MACE occurrence were significantly associated, and no interactions were observed (Table 5). Among patients without complete ST-segment resolution before intervention, an ST peak was a significant predictor of MACE, whereas ST peak seemed to be a weaker predictor in patients with complete ST-segment resolution before intervention (Table 5). In a separate analysis of patients treated with conventional PCI alone (patients randomised to placebo in all three studies), ST peak was also a predictor for MACE (Table 5) with highly overlapping confidence intervals, and no interaction was observed. Among the 253 patients with an ST peak, neither the absolute ST-segment increase (p=0.51), the relative ST-segment increase (p=0.67) nor the duration of the ST peak (p=0.34) was related to MACE in Cox regression analyses.
Discussion
The ST peak phenomenon was observed in approximately 27% of the STEMI patients treated with primary PCI. The main findings of this retrospective post hoc study were: 1) ST peak is an independent predictor for adverse clinical outcome in STEMI patients; 2) ST peak provides prognostic information beyond that provided by final ST-segment resolution, transient reduced flow, epicardial TIMI flow and infarct territory; 3) the prognostic value of an ST peak seems to rely on the mere presence of an ST-segment increase but not on the duration and the magnitude of the increase; 4) ST peak was associated with delayed ST-segment resolution and suggested impaired microvascular perfusion. Thus, these findings support continuous ECG monitoring during primary PCI as an easy and valuable tool for risk assessment in the acute phase. Moreover, the ST peak phenomenon may be a target for future treatments adjuvant to primary PCI, but whether it is modifiable remains unknown.
ST PEAK AS PROGNOSTIC PREDICTOR
As mentioned, traditional ST-segment resolution is widely accepted as a prognostic predictor in patients with STEMI treated with primary PCI6-13, but it is evaluated after the procedure and is therefore of limited guidance for the PCI operator. There are also other important risk factors in STEMI patients; however, many of these are either present before the onset of infarction (e.g., age, hypertension and previous PCI) or evaluated after the PCI procedure (e.g., peak troponin T, left ventricular volume and function, infarct size and ST-segment resolution). In contrast, assessment of ECG changes during the procedure may help to risk stratify the patients immediately, while still in the catheterisation laboratory, and may serve as an earlier predictor than traditional ST-segment resolution and other more traditional risk factors. Since ST peak is a phenomenon occurring during the procedure, it has the potential to serve as a guide for the PCI operator. Thus, the main advantage of ST peak over other important risk factors in STEMI patients is the timing. In a previous study of 21 patients with anterior STEMI, an ST peak during perfusion with PCI was related to development of in-hospital heart failure18. In that study, patients were pre-treated with aspirin and heparin but no supplementary antiplatelet regimen was administered that has otherwise been shown to improve myocardial perfusion32. The newer antiplatelet drugs do not lead to any further improvement in myocardial perfusion compared with clopidogrel33. A small pilot study performed by our institute indicated that the occurrence of an ST peak during primary PCI was related to an increase in cardiac events in patients pre-treated with aspirin, heparin and clopidogrel20. However, that study was not powered to draw firm conclusions in terms of clinical outcome. Pooling patients from that study with a previously published study with available ST peak data27 led to this cohort probably being the largest hitherto for evaluation of the clinical importance of ST peak. The present study strengthens ST peak as a strong predictor for MACE in patients treated with primary PCI, but also for mortality and for the development of heart failure per se. Moreover, the sample size of the present study allows for evaluation of important subgroups. In this study, several baseline variables were related to either a higher or a lower occurrence of ST peak and may explain its prognostic value. However, even after adjustment for these variables and analyses of subgroups, ST peak occurrence remained significantly associated with the MACE rate, rendering ST peak occurrence an independent prognostic marker. In addition, many of these variables were not per se associated with MACE in this STEMI cohort, and variables such as previous PCI and multivessel disease were related to MACE, but less frequently observed in patients with ST peak.
PATHOPHYSIOLOGY OF ST PEAK
Since ST peak occurs concomitantly with reperfusion it is also referred to as the reperfusion syndrome18. Data from the present study showed that reduced epicardial coronary flow might partly explain this phenomenon, which is in accordance with a previous study showing that ST peak is associated with a transient reduction in the coronary blood flow18. However, ST peak occurs in 67% without transient reduced epicardial blood flow and 88% with final TIMI 3 flow, leaving room for alternative explanations such as reduced microvascular perfusion and reperfusion injury. Whereas ST peak seems to be related to impaired microvascular perfusion as indicated by final ST-resolution data in this study, it seems difficult to evaluate the association between ST peak and reperfusion injury. However, since reperfusion injury occurs during reperfusion, this could indicate that the ST peak phenomenon is also a marker of reperfusion injury. Moreover, the prognostic value of ST peak was not dependent on a reduced epicardial coronary flow, indicating that ST peak is to some extent related to myocardial damage at the cellular level (reperfusion injury). However, more data are necessary to evaluate this hypothesis.
The definition of 1 mm or more of additional ST-segment elevation has inherent bias since the same threshold was applied to all myocardial territories (anterior versus non-anterior). Therefore, it is not surprising that anterior myocardial infarction is an independent predictor of ST peak, but this definition was chosen since 1 mm is considered significant.
Limitations
Patients in the present study were pooled from three randomised studies evaluating different treatments and with small differences in the inclusion and exclusion criteria, which could have affected the results. Still, in both subgroups treated with either conventional PCI or active treatment, ST peak was associated with clinical outcome and no interaction was observed. There was no difference when the patients were stratified according to the three studies with no heterogeneity between studies. Therefore, inclusion of patients randomised to active treatment from three different studies did not affect the overall results and conclusions, and ST peak during primary PCI seems to be a robust predictor independent of reperfusion strategy by PCI. Angiographic lesion characteristics evaluated by independent core laboratory technicians were only available from one of the three studies. However, since these data were acquired from consecutively treated patients, it is unlikely that conclusions based upon these data were affected by selection bias. Myocardial blush grade, a predictor of myocardial perfusion and clinical outcome3,5, was not available, but microvascular dysfunction was assessed by final ST-segment elevation and resolution, which is known to be highly associated with myocardial blush grade3. ST-segment resolution is also considered a stronger predictor of microvascular obstruction than myocardial blush grade34. Thus, since ST-segment resolution was used in the present study, it is questionable whether data regarding myocardial blush would have changed the results and conclusions of the present paper. The association between myocardial blush grade and ST peak needs to be assessed in future studies. A further limitation was the low prognostic value of pre-PCI TIMI 0/1 flow and anterior infarct location in this STEMI cohort. The low prognostic value of pre-TIMI flow might be due to patients with aborted STEMI being excluded, whereas the authors have no explanation for the low prognostic value of anterior infarct location, but this could be the cause of a type I error. The low prognostic value of achievement of 70% ST-segment resolution after 90 minutes in this study is in accordance with previous findings in patients treated with primary PCI11,12. Owing to the many statistical comparisons, some significant differences may have been observed by chance, leading to a risk of type II errors. However, even after adjustment for multiple comparisons, ST peak was still significantly associated with the primary endpoint MACE.
Conclusion
In the largest study hitherto evaluating the ST peak phenomenon during primary PCI, we demonstrated that ST peak is a strong predictor of adverse long-term outcome and provides independent prognostic information beyond that provided by final ST-segment resolution and epicardial flow.
| Impact on daily practice Approximately one-third of STEMI patients treated with primary PCI experience a secondary ST-segment elevation (ST peak) during reperfusion. This phenomenon is related to poorer myocardial reperfusion and is an independent predictor for impaired prognosis. Thus, in daily practice, continuous ECG monitoring during primary PCI and assessment of ST peak is an easy and valuable tool for immediate risk assessment of these patients. |
Funding
Financial support was obtained from the Danish Heart Foundation and Rigshospitalet Research Foundation.
Conflict of interest statement
The authors have no conflicts of interest to declare.