Case description
Incomplete stent apposition (ISA) is under reported and although previously considered benign1, a recent report has confirmed an association with stent thrombosis2.
We report a case of ISA occurring in a patient enrolled into a prospective registry of long sirolimus drug-eluting stent (DES) deployment (>23 mm). Repeat angiography with intravascular ultrasound (IVUS) was undertaken at 10 and 28 months; (Figure 1, Panels A-F). Further assessment at 59 months, precipitated by troponin-positive chest-pain, revealed angiographic evidence of ISA, and IVUS confirmed ISA (Figure 1, Panels G-I), which had markedly progressed from the IVUS images obtained at 10 and 28 months. The patient has been prescribed lifelong dual antiplatelet therapy and remains well.
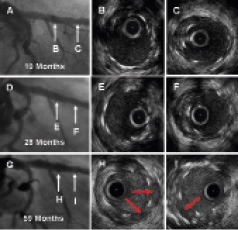
Figure 1. Serial angiographic and intravascular ultrasound images demonstrating progressive incomplete stent apposition. Panels A, D, and G allow angiographic comparison of the stented left anterior descending artery at 10 months, 28 months and 59 months (annotated white arrows correspond with the intravascular ultrasound cross-sections). Panels B & C are representative cross-sectional IVUS images from the mid- and distal-segments of the stented LAD, at 10 month follow-up. Panels E and F are equivalent cross-sectional images acquired at 28 month follow-up. Panels H and I represent comparative images at 59 months, with clear-cut evidence of incomplete stent apposition highlighted by the red arrows.
We report very-late ISA utilising sequential angiographic and IVUS assessment clearly demonstrating the progressive nature of ISA. Although the aetiology of ISA remains uncertain, recent data has added support to the concept of late positive remodelling secondary to an arterial inflammatory response; more specifically linking sirolimus DES with a type IVb delayed hypersensitivity reaction3.
This case confirms that patients with first generation DES are at threat of negative sequelae related to their intervention, long after stent deployment, highlighting the potential need for long-term surveillance of patients treated with DES.
Online data supplement
Video 1. Angiogram of late ISA.
Video 2. An intravascular ultrasound pullback, acquired more than four years post deployment of two overlapping sirolimus-eluting stents, demonstrating significant stent malapposition.

