Abstract
Aims: The Academic Research Consortium for High Bleeding Risk (ARC-HBR) defined consensus-based criteria for patients at high bleeding risk (HBR) undergoing percutaneous coronary intervention (PCI). We aimed to validate the ARC-HBR criteria for the bleeding outcomes using a large cohort of patients undergoing PCI.
Methods and results: Between 2009 and 2016, patients undergoing PCI were prospectively included in the Bern PCI Registry. Patients were considered to be at HBR if at least one major criterion or two minor criteria were met. The primary endpoint was Bleeding Academic Research Consortium (BARC) 3 or 5 bleeding at one year; ischaemic outcomes were assessed using the device-oriented composite endpoints (DOCE) of cardiac death, target vessel myocardial infarction, and target lesion revascularisation. Among 12,121 patients, those at HBR (n=4,781, 39.4%) had an increased risk of BARC 3 or 5 bleeding (6.4% vs 1.9%; p<0.001) and DOCE (12.5% vs 6.1%; p<0.001) compared with those without HBR. The degree of risk and prognostic value were related to the risk factors composing the criteria. The ARC-HBR criteria had higher sensitivity than the PRECISE-DAPT score and the PARIS bleeding risk score (63.8%, 53.1%, 31.9%), but lower specificity (62.7%, 71.3%, 86.5%) for BARC 3 or 5 bleeding.
Conclusions: Patients at HBR defined by the ARC-HBR criteria had a higher risk of BARC 3 or 5 bleeding as well as DOCE. The bleeding risk was related to its individual components. The ARC-HBR criteria were more sensitive for identifying patients with future bleedings than other contemporary risk scores at the cost of specificity. ClinicalTrials.gov Identifier: NCT02241291
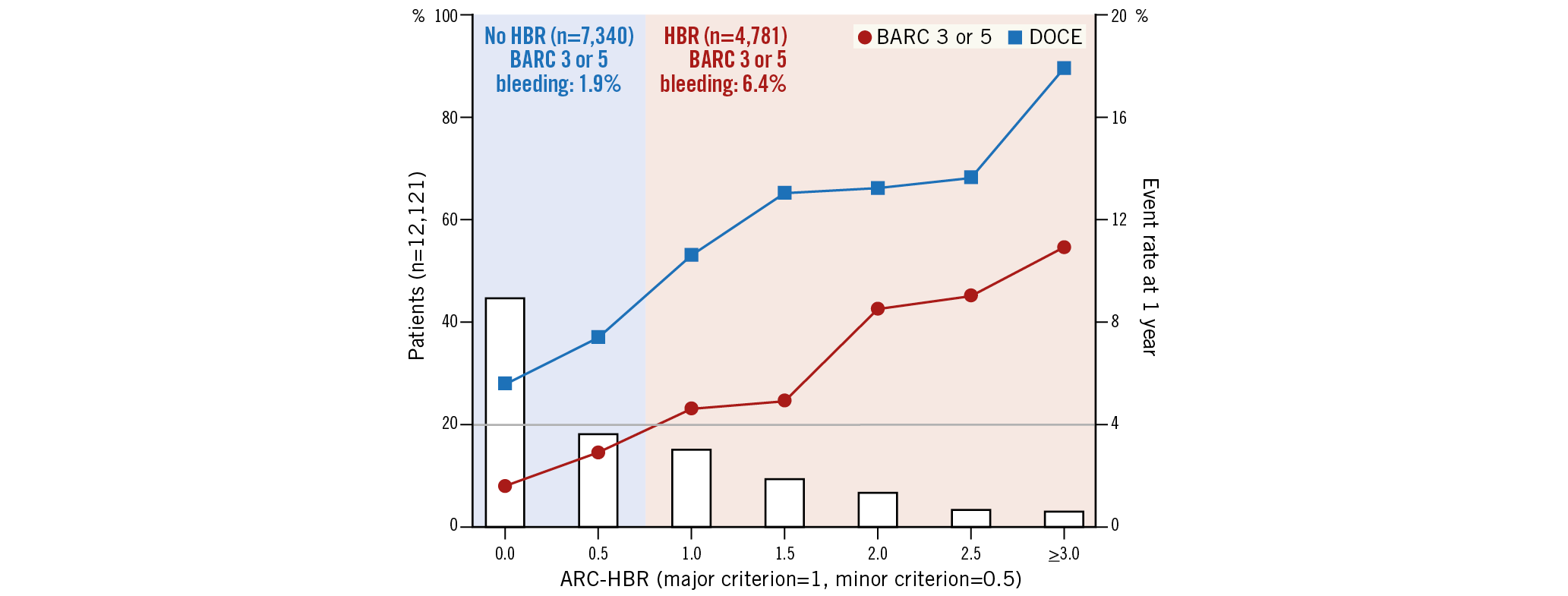
Visual summary. According to the ARC-HBR criteria, 40% of patients undergoing PCI were at HBR. Compared with patients without HBR, those at HBR had an increased risk of BARC 3 or 5 bleeding (6.4% vs 1.9%, p<0.001). There was a gradual risk increase for BARC 3 or 5 bleeding and DOCE as a function of the ARC-HBR score. BARC: Bleeding Academic Research Consortium; DOCE: device-oriented composite endpoints; HBR: high bleeding risk.
Introduction
Following percutaneous coronary intervention (PCI), the impact of major bleeding on prognosis is at least as pronounced as that of myocardial infarction1,2. Dual antiplatelet therapy (DAPT) reduces the risk of stent- and non-stent-related ischaemic adverse events in patients undergoing PCI; however, this benefit is offset (at least in part) in patients at high bleeding risk (HBR) and is directly related to the duration of DAPT. A recent study demonstrated that patients at HBR did not gain benefit from long-term DAPT irrespective of the underlying ischaemic risk, suggesting that the characterisation of bleeding risk outweighs ischaemic risk (i.e., PCI complexity) in terms of optimal DAPT duration3.
Although several bleeding prediction scores are currently available and received a Class IIb (level A) recommendation in the 2017 European Society of Cardiology Focused Update on DAPT to characterise patients undergoing PCI4, they afford a modest discrimination ability with an average C-statistic of approximately 0.7 to predict bleeding5,6. In the clinical trial setting, heterogeneous definitions of HBR have been applied across numerous studies, which may limit the interpretation and generalisability of reported data7,8,9. Against this background, the Academic Research Consortium for High Bleeding Risk (ARC-HBR), a collaboration among leading research organisations, regulatory authorities, and physician-scientists from the USA, Asia, and Europe focusing on PCI-related bleeding, developed a consensus-based definition of patients at HBR in May 201910. HBR was arbitrarily defined as one-year risk of ≥4% for a Bleeding Academic Research Consortium (BARC) 3 or 5 bleeding or ≥1% for intracranial haemorrhage (ICH). To date, data on the applicability of the ARC-HBR criteria in the real-world setting are scarce. Therefore, we validated the ARC-HBR criteria to predict bleeding outcomes using prospective data from a large cohort of unselected, consecutive patients undergoing PCI.
Methods
PATIENT POPULATION
All consecutive patients undergoing PCI at Bern University Hospital, Switzerland, were prospectively enrolled into the Bern PCI Registry (NCT02241291) between January 2009 and December 2016. For the present study, patients undergoing balloon angioplasty alone or implantation of bioresorbable scaffolds and those in whom ARC-HBR criteria could not be completely ascertained were excluded. The registry was approved by the institutional ethics committee. All patients provided written informed consent.
ARC-HBR CRITERIA
Some of the ARC-HBR criteria needed to be modified or were not available due to the data availability in the registry, as summarised in Supplementary Table 1. Major and minor ARC-HBR criteria applied in the current study are as follows: age ≥75 years (minor); oral anticoagulant or novel oral anticoagulant at discharge (major); estimated glomerular filtration rate (eGFR) <30 ml/min (major) and eGFR ≥30, <60 ml/min (minor); baseline haemoglobin <11 g/dL (major), and 11-12.9 g/dL for men and 11-11.9 g/dL for women (minor); spontaneous non-intracranial bleeding requiring hospitalisation or transfusion (major); thrombocytes at index PCI <100×109/L (major); non-steroidal anti-inflammatory drugs (NSAIDS) at discharge (minor); cancer history within one year prior to index PCI and/or ongoing treatment, excluding non-melanoma skin cancer (major); previous intracranial bleeding or previous stroke (major); any ischaemic stroke at any time not meeting the major criterion (minor). Definitions of the ARC-HBR criteria are provided in Supplementary Appendix 1. Patients were considered to be at HBR if at least one major criterion or two minor criteria were met10. The ARC-HBR score was calculated by adding 1 point for any major criterion and 0.5 for any minor criterion.
PROCEDURE
PCI was performed according to current guidelines11. Heparin (at least 5,000 IU or an initial bolus of 100 IU per kg body weight) was used for procedural anticoagulation with the aim of maintaining an activated clotting time >250 msec. The periprocedural use of glycoprotein IIb/IIIa inhibitors was left to the discretion of the operator. DAPT consisting of acetylsalicylic acid and a P2Y12 inhibitor was initiated before, at the time of, or immediately after the procedure. Prasugrel was introduced as of September 2009, and ticagrelor as of November 2011. The majority of patients with chronic coronary syndrome (CCS) received clopidogrel. The routinely recommended DAPT duration was 12 months12.
CLINICAL ENDPOINTS
The primary bleeding endpoint was bleeding defined as Bleeding Academic Research Consortium (BARC) 3 or 513. Secondary endpoints, definitions, and patient follow-up are provided in Supplementary Appendix 2.
STATISTICAL ANALYSIS
Continuous variables were summarised as mean±standard deviation or median and interquartile range, and compared with the Student’s t-test or the Mann-Whitney U test. Binary and categorical variables were calculated as frequencies (percentages) and were compared with the chi-square test or Fisher’s exact test. Kaplan-Meier cumulative event curves were constructed for time-to-event variables and compared using the log-rank test. Subhazard ratio was obtained from a competing risk survival regression based on Fine and Gray’s proportional subhazard model. Discrimination of the bleeding risk score was assessed by the C-statistic. Calibration was assessed by comparing predicted probabilities with the observed frequency of BARC 3 or 5 bleeding. Cox regression analysis was performed to test the prognostic significance of each component of the ARC-HBR criteria for BARC 3 or 5 bleeding and device-oriented composite endpoints (DOCE). Each component of the ARC-HBR criteria was adjusted by all components of the ARC-HBR criteria and clinically important variables reported by previous studies. For BARC 3 or 5 bleeding, female gender, body mass index, current smoker, hypertension, peripheral artery disease, acute coronary syndrome, and potent P2Y12 at discharge, and for DOCE, age, female gender, current smoker, hypertension, peripheral artery disease, previous myocardial infarction, previous revascularisation (PCI and/or coronary artery bypass graft [CABG]), left ventricular ejection fraction, stent type (bare metal stent, first-generation drug-eluting stent), were entered into a multivariate model5,6,14,15. P-values were two-tailed and a value under 0.05 was considered statistically significant in all analyses. Statistical analyses were performed with R, version 3.4.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
PATIENTS
Of 13,748 patients enrolled into the Bern PCI Registry between January 2009 and December 2016, 12,121 patients were analysed for the present study with complete follow-up available in 11,314 (93.3%) patients at one year. Patients were excluded in case of balloon angioplasty without stent implantation (n=496), implantation of bioresorbable scaffolds (n=60), or if not all of the ARC-HBR criteria were assessable (n=1,071: missing haemoglobin [n=437], missing eGFR [n=710], missing thrombocytes [n=564], missing data on NSAIDs [n=152]).
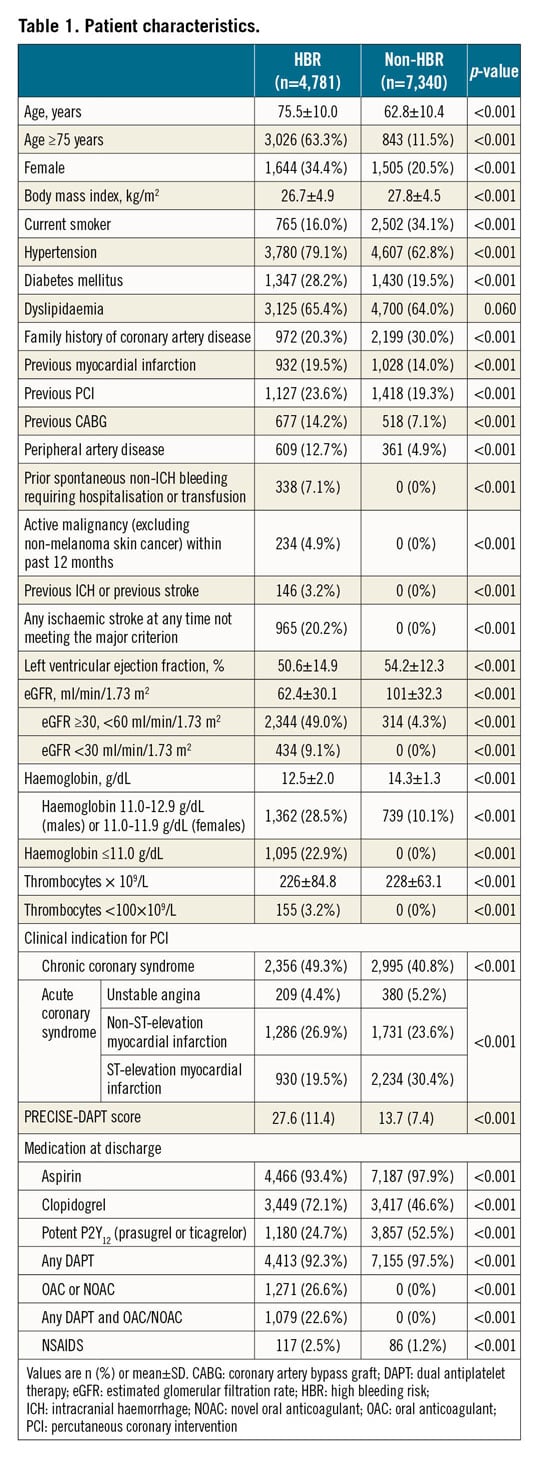
BASELINE CHARACTERISTICS
Clinical and procedural characteristics and medication status are summarised in Table 1, Supplementary Table 2 and Supplementary Table 3. Patients at HBR (n=4,781, 39.4%) were older and more commonly female, had more risk factors for atherosclerotic cardiovascular disease, comorbidities, CCS as an indication for PCI, and had higher PRECISE-DAPT scores compared with those without. Among HBR patients, PCI was more frequently performed in the anatomical setting of the left main and saphenous vein bypass grafts. New-generation drug-eluting stents were used in 93.4% of all patients with a lower frequency in patients at HBR. The use of potent P2Y12 inhibitors was less frequent in patients at HBR.
ARC-HBR CRITERIA
The prevalence of ARC-HBR criteria is summarised in Figure 1. Age ≥75 years (31.9%), anaemia (26.4%), chronic kidney disease (CKD) (25.5%), oral anticoagulation (10.5%), and previous ICH or stroke (8.0%) were the leading ARC-HBR criteria in decreasing order. Prior spontaneous non-ICH bleeding (2.8%), thrombocytopaenia (1.3%), NSAIDS (1.7%), and active malignancy (1.9%) were rarely observed. Major CKD, major anaemia, and spontaneous non-ICH bleeding frequently overlapped with other criteria, as illustrated in Supplementary Figure 1. The ARC-HBR score had a C-statistic of 0.69 (95% CI: 0.66-0.71) for BARC 3 or 5 bleeding and showed accurate calibration (Supplementary Figure 2). Sensitivity, specificity, positive predictive value, negative predictive value, and accuracy of the ARC-HBR score ≥1 (i.e., equivalent to one major or two minor ARC-HBR criteria) for BARC 3 or 5 bleeding at one year were 68.5%, 61.7%, 6.4%, 98.1%, and 61.9%, respectively. As an explanatory analysis, we compared the diagnostic ability and C-statistics among the ARC-HBR score, PRECISE-DAPT score, and PARIS bleeding score in patients in whom all three scores were available (n=10,551) (Figure 2). The ARC-HBR criteria had higher sensitivity compared with other bleeding risk scores at the cost of lower specificity.
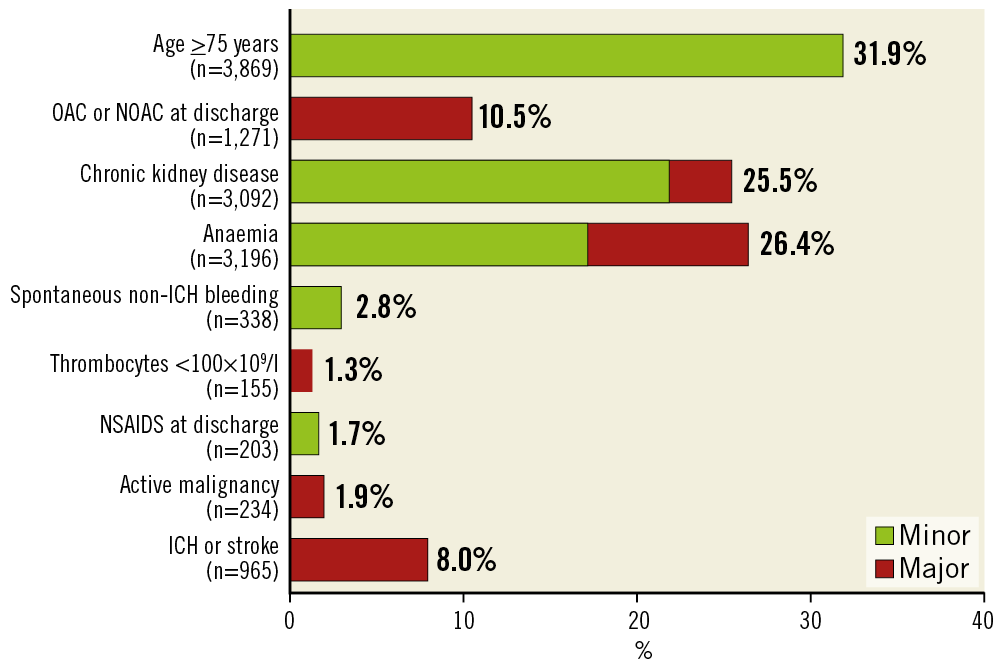
Figure 1. Distribution of the ARC-HBR criteria. DAPT: dual antiplatelet therapy; ICH: intracranial haemorrhage; NOAC: novel oral anticoagulant; OAC: oral anticoagulant; PCI: percutaneous coronary intervention
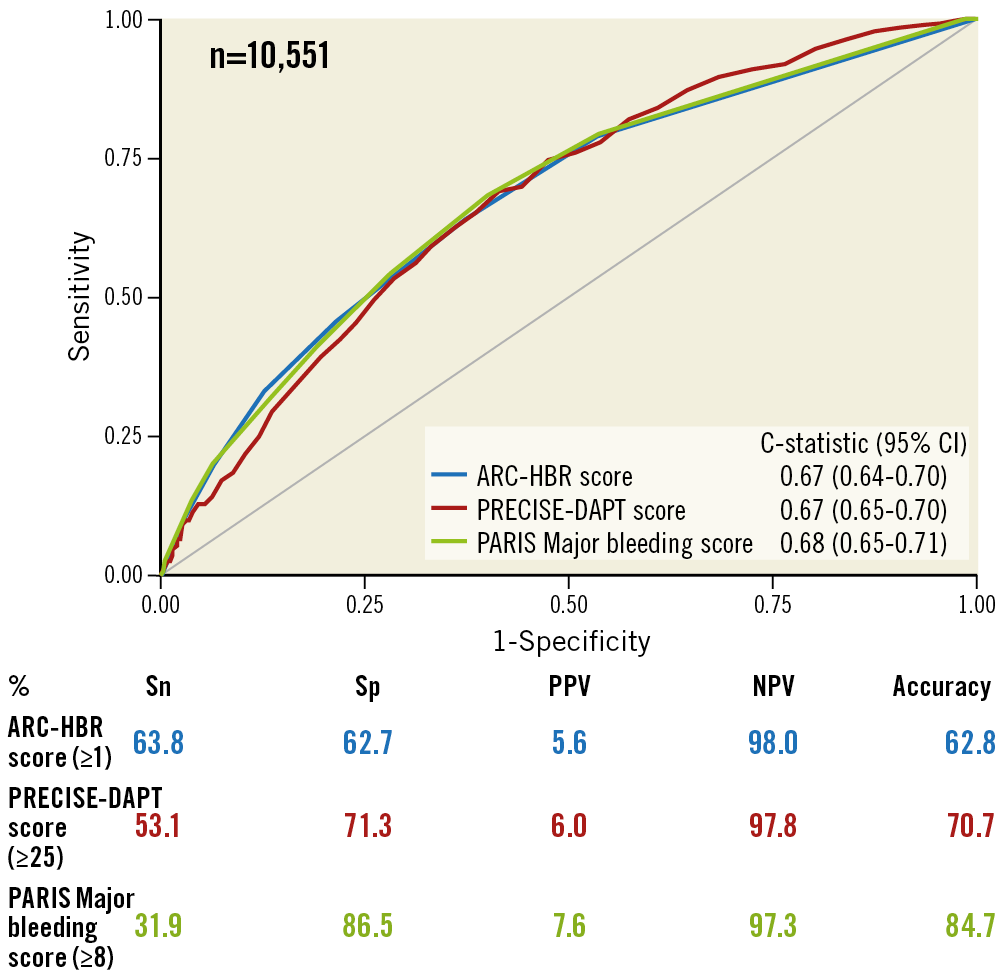
Figure 2. ROC curves and diagnostic ability of bleeding prediction systems for one-year BARC 3 or 5 bleeding. BARC: Bleeding Academic Research Consortium; CI: confidence interval; NPV: negative predictive value; PPV: positive predictive value; ROC: receiver operating characteristic; Sn: sensitivity; Sp: specificity
CLINICAL OUTCOMES
Clinical outcomes at one year are summarised in Table 2. Compared to patients without HBR, those at HBR had an increased risk of BARC 3 or 5 bleeding (6.4% vs 1.9%, p<0.001) and DOCE (12.5% vs 6.1%, p<0.001) as well as other secondary endpoints including net adverse composite endpoints, all-cause death, cardiac death, myocardial infarction, target lesion revascularisation, definite stent thrombosis, stroke, and each BARC component. Patients at HBR had an increased risk of BARC 3 or 5 bleeding after considering all-cause death as a competing risk (hazard ratio 3.44, 95% CI: 2.80 to 4.17; p<0.001). There was a gradual risk increase for BARC 3 or 5 bleeding (0, 0.5: 1.9%, 1: 4.6%, and ≥1.5: 7.6%, p<0.001) and DOCE (0, 0.5: 6.1%, 1: 10.6%, and ≥1.5: 13.9%, p<0.001) as a function of the ARC-HBR score (Figure 3). The frequency of BARC 3 or 5 bleeding and DOCE for each ARC-HBR score was: 0: 1.6% and 5.6%, 0.5: 2.9% and 7.4%, 1: 4.6% and 10.6%, 1.5: 4.9% and 13.0%, 2: 8.5% and 13.2%, 2.5: 9.0% and 13.6%, ≥3: 10.9% and 17.9%, respectively (Figure 4). Each ARC-HBR criterion except for NSAIDS at discharge was associated with a BARC 3 or 5 bleeding risk of ≥4% (Figure 5), while the bleeding risk associated with an ARC-HBR score of 0.5 or 1 was dependent on the individual criteria of the score (Table 3).
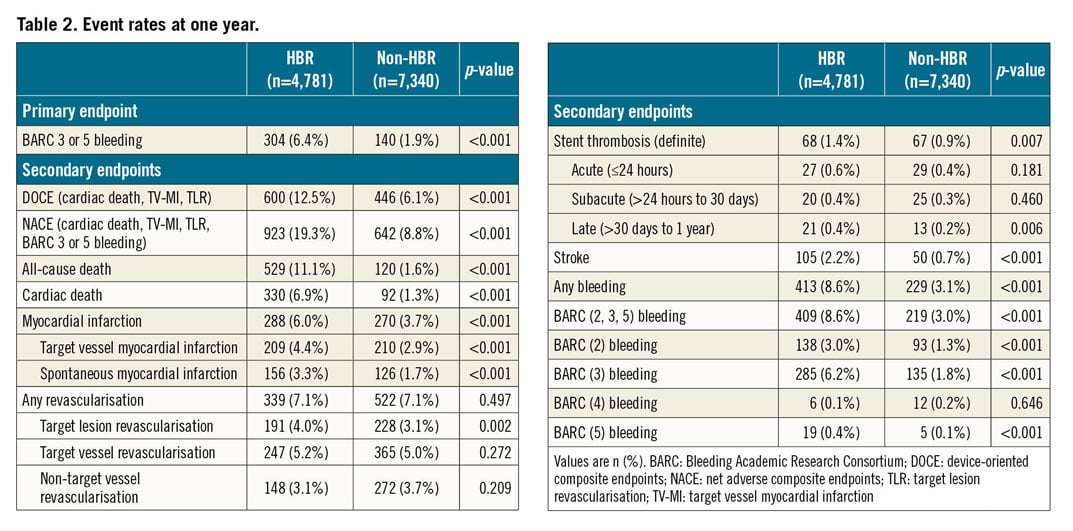
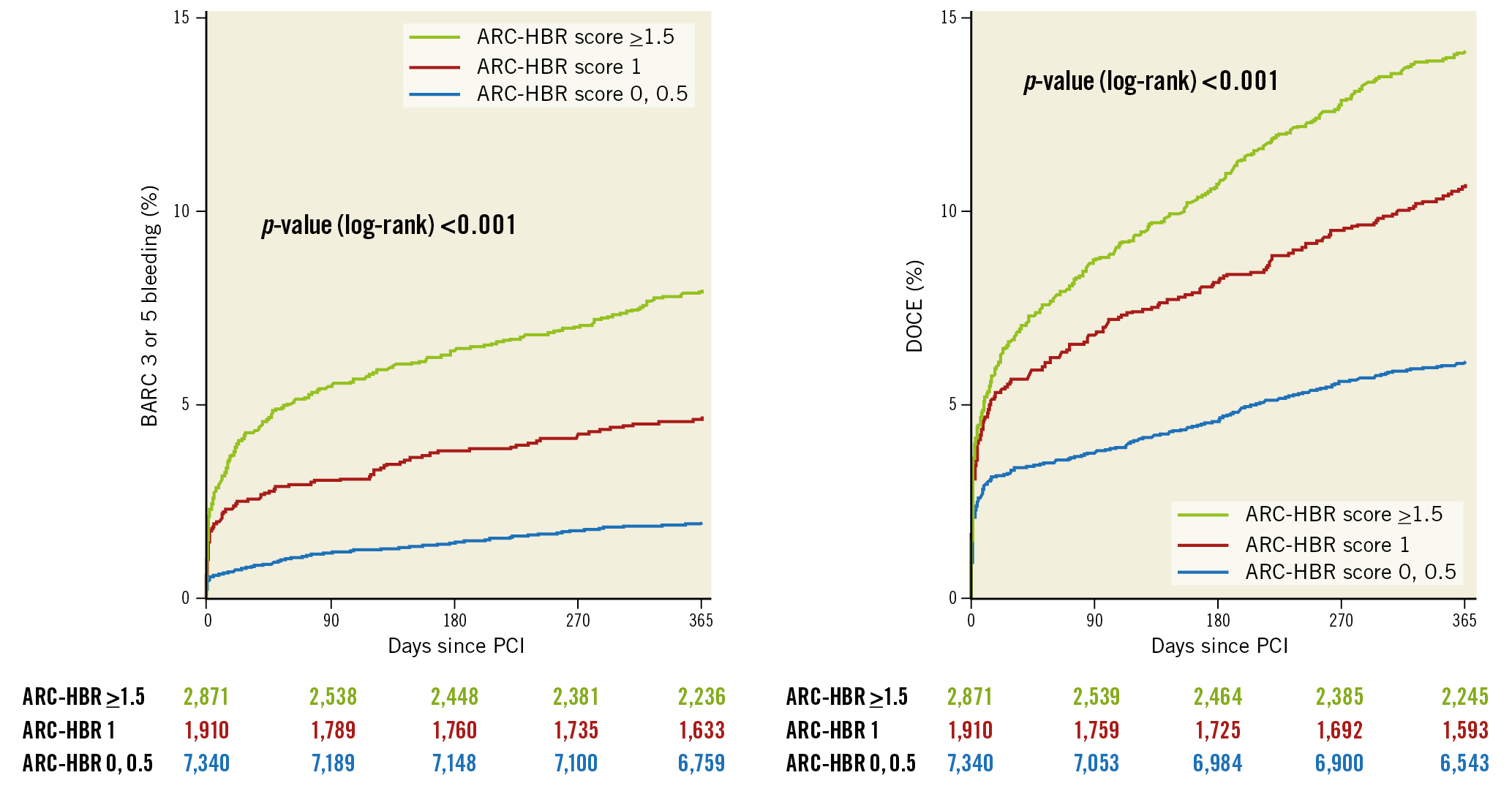
Figure 3. Kaplan-Meier cumulative event curves for BARC 3 or 5 bleeding and DOCE at one year stratified by the ARC-HBR score. BARC: Bleeding Academic Research Consortium; DOCE: device-oriented composite endpoints; PCI: percutaneous coronary intervention
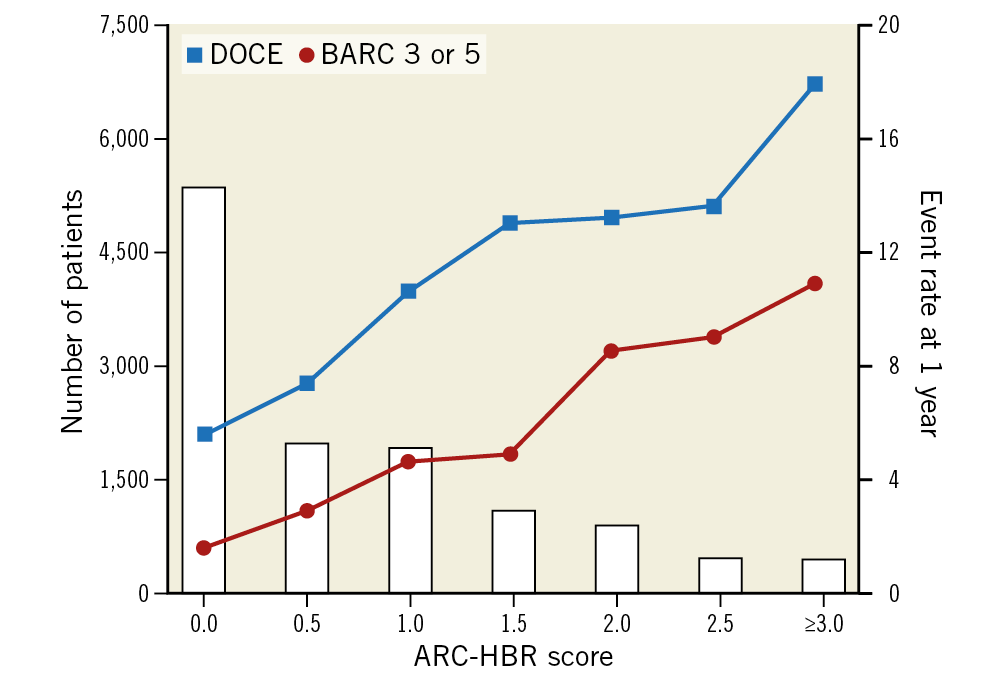
Figure 4. Event rates according to the ARC-HBR score. BARC: Bleeding Academic Research Consortium; DOCE: device-oriented composite endpoints
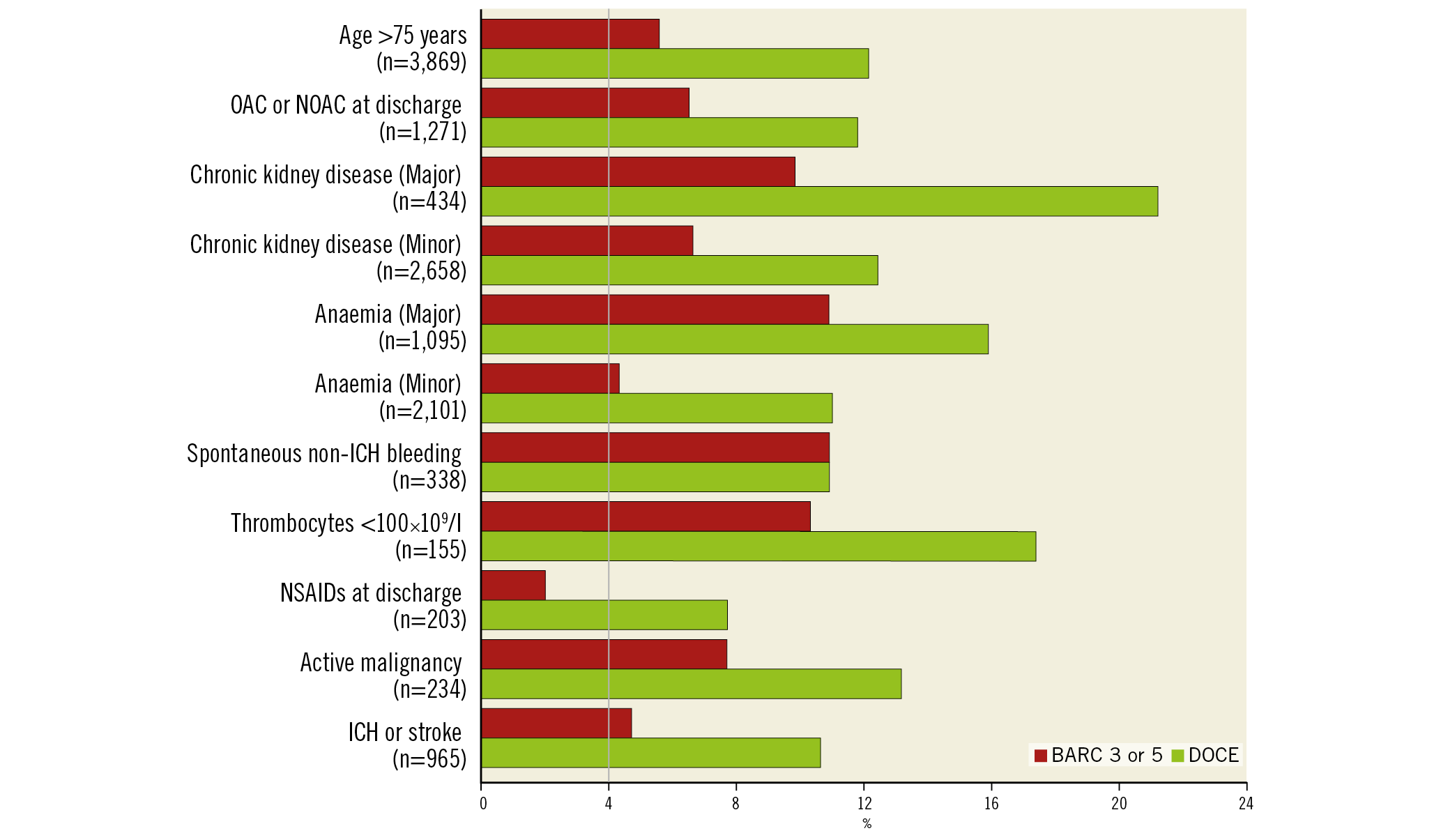
Figure 5. Event rates at one year according to ARC-HBR criteria. BARC: Bleeding Academic Research Consortium; DAPT: dual antiplatelet therapy; DOCE: device-oriented composite endpoints; ICH: intracranial haemorrhage; NOAC: novel oral anticoagulant; OAC: oral anticoagulant; PCI: percutaneous coronary intervention
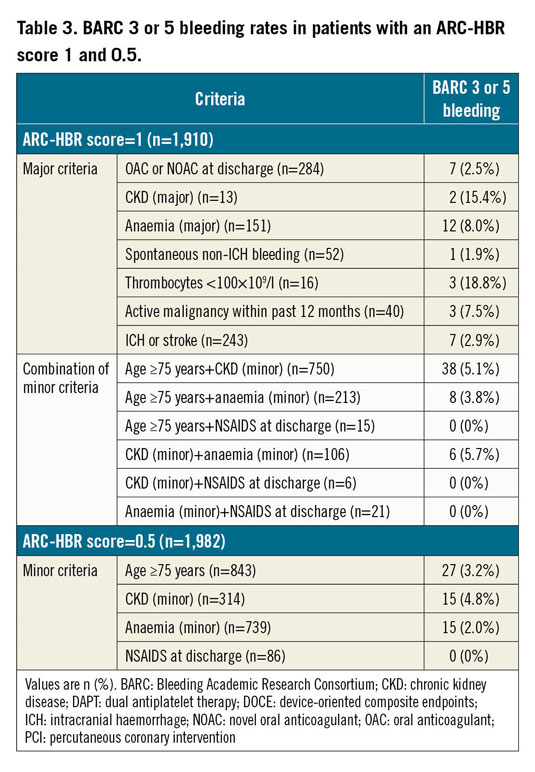
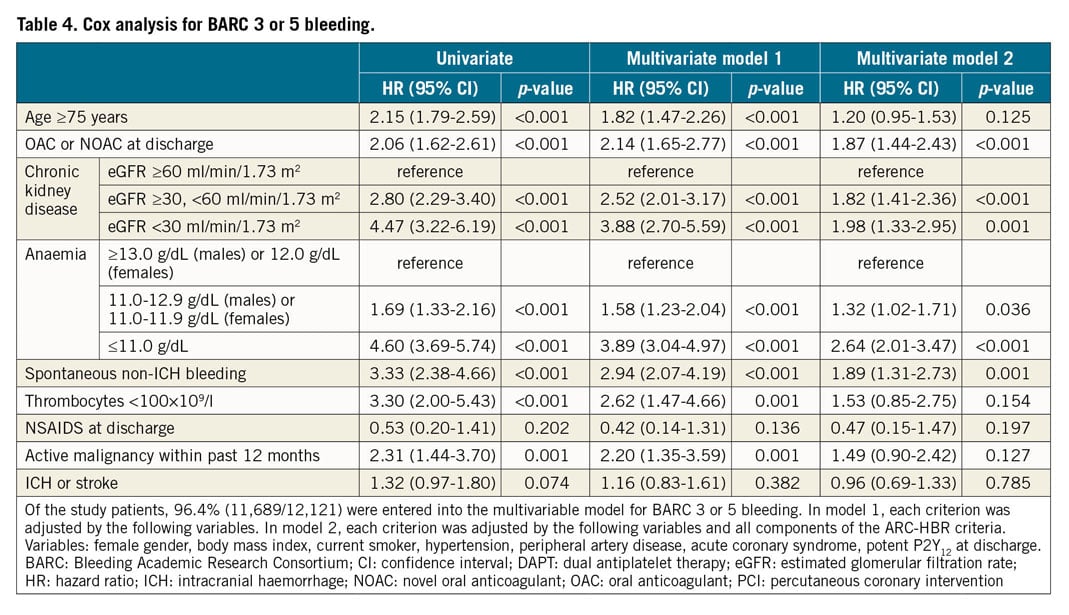
COX REGRESSION ANALYSIS
The unadjusted and adjusted risks of individual components of the ARC-HBR criteria for BARC 3 or 5 bleeding and DOCE at one year are presented in Table 4 and Supplementary Table 4, respectively. An oral anticoagulant (OAC) or novel oral anticoagulant (NOAC) at discharge and prior spontaneous non-ICH bleeding emerged as independent predictors for BARC 3 or 5 bleeding at one year, while CKD and anaemia were associated with both BARC 3 or 5 bleeding and DOCE.
Discussion
The implementation of bleeding avoidance strategies is considered relevant as bleeding contributes substantially to adverse outcomes including mortality1,2. Guidelines support the use of bleeding risk scores (class IIb, level A) to predict bleeding and potentially tailor antithrombotic therapies. However, these scores depend on the characteristics of patients included in the derivation cohort and are not necessarily applicable to routine clinical practice. The ARC-HBR criteria represent a new and pragmatic consensus-based approach to predict bleeding. Our study aimed to evaluate in detail the ARC-HBR criteria using an unselected PCI population consecutively enrolled at a large tertiary care centre.
Patients at HBR according to the ARC-HBR criteria were frequent (≈40%). The criteria including age ≥75 years, CKD, anaemia, oral anticoagulation, and previous ICH or stroke were frequently observed in the real-world PCI population, in line with inclusion criteria applied in previous HBR studies7,9, while prior spontaneous non-ICH bleeding, thrombocytopaenia, NSAIDS, and active malignancy were relatively rare.
Patients at HBR had a higher risk (6.4%) of bleeding at one year as defined by BARC 3 or 5, exceeding the anticipated threshold of 4.0%. The rate of BARC 3 or 5 bleeding of 1.9% at one year in patients without HBR was comparable with results obtained from previous DAPT trials (i.e., <3.0%) with systematic exclusion of HBR patients10. It is noteworthy that patients fulfilling one minor criterion carried a twofold higher bleeding risk as compared with patients without HBR (2.9% vs 1.6%). Further studies should investigate whether “intermediate-risk” patients (i.e., one minor criterion) and “truly low-risk” (i.e., no criterion) should be treated equally in terms of DAPT intensity and duration.
Although the bleeding risk increased proportionally with increasing number of ARC-HBR criteria, importantly the degree of risk and prognostic value varied considerably among the ARC-HBR criteria. In the ARC-HBR consensus document, a major criterion is defined as any criterion that, in isolation, confers a BARC 3 or 5 bleeding risk of ≥4% at one year, and a minor criterion is defined as any criterion that, in isolation, confers increased bleeding risk with a BARC 3 or 5 bleeding rate of <4% at one year10. Although this analysis includes only a limited number of patients with each criterion being present in isolation, not all criteria met the expectation of predicting a BARC 3 or 5 bleeding risk ≥4% (major) or <4% (minor). Patients who fulfilled only “anticipated long-term use of an oral anticoagulant” (major criterion) had a BARC 3 or 5 bleeding rate of 2.5%, while patients with “eGFR ≥30, <60 ml/min/1.73 m2” (minor criterion) had a bleeding risk of 4.8% at one year. Our data suggest that the bleeding risk associated with an ARC-HBR score 0.5 or 1 was dependent on the individual criteria composing the score. Physicians should note that an individualised approach based on the applied criteria may be needed in patients with an ARC-HBR score 0.5 or 1.
Consistent with previous analyses16, HBR patients incurred an increased risk not only of bleeding but also of multiple ischaemic events including cardiac death, myocardial infarction and stent thrombosis. HBR patients had more frequent risk factors correlating with atherosclerotic disease burden such as diabetes mellitus and previous revascularisation, explaining in part the excess in ischaemic events. The dilemmatic dual impact of certain clinical characteristics such as renal failure was consistent with one of our previous analyses on the same cohort16 as well as previous studies6,17. Although many operators are still reluctant to use newer-generation DES in HBR patients, there was only a small difference between groups in this cohort (92.0% vs 94.3%), which may not be applied as an explanation for an increased risk of ischaemic events. Patients categorised as HBR may represent a frailer population, a characteristic that was not specifically assessed in the Bern PCI Registry, i.e., a notion supported by a higher frequency of non-cardiac mortality (4.2% vs 0.3%).
The ARC-HBR criteria categorised approximately 40% of an unselected PCI population as HBR, while fewer patients were identified as HBR by other bleeding risk scores. Specifically, 26.9% of patients fulfilled the PRECISE-DAPT score ≥25 and 14.5% fulfilled the PARIS bleeding score ≥8. Accordingly, the ARC-HBR criteria were more sensitive than others (ARC-HBR score ≥1: 63.8% vs PRECISE-DAPT score ≥25: 53.1% vs PARIS bleeding score ≥8: 31.9%) at the cost of specificity (62.7% vs 71.3% vs 86.5%). The C-statistics were comparable among the three bleeding prediction systems. In contrast to the consistently high negative predictive value, a limited positive predictive value represents a common limitation of clinical bleeding prediction tools, although an impact of a relatively low rate of bleeding events on positive predictive value needs to be considered. In light of a limited performance of bleeding prediction systems and the large overlap with ischaemic events in HBR patients, it remains of the utmost importance to conduct randomised controlled trials (RCTs) investigating the impact of score-based treatment strategies.
To date, only one study has attempted to validate the ARC-HBR criteria: it suggested that patients at HBR had a higher bleeding rate and that each individual ARC-HBR criterion was associated with a major bleeding risk >4% at one year18. However, the analysis did not include BARC bleeding as endpoints and was carried out in an Asian (Japanese) population. In the present study, we confirmed consistent results with the BARC bleeding definition using a large PCI data set of an European population.
Limitations
First, the single-centre design of this study may limit the generalisability of our findings. Second, four ARC-HBR criteria were not applicable and three needed to be substantially modified due to the data availability in the registry, which might hinder a complete review of criteria and precise estimates of the bleeding risk for each HBR criterion in isolation as well as potential cumulative effects, although missing criteria in the present study appear to be rare. Lastly, DAPT duration and intensity cannot be considered due to the nature of the observational study design. The results need to be interpreted against the background of a routine 12-month DAPT duration determined by operator’s discretion in most patients, while bleeding risk associated with oral anticoagulation might be underestimated due to the shortened duration of DAPT in patients with triple therapy (i.e., DAPT and OACs).
Conclusions
Patients at HBR defined by the ARC-HBR criteria were as frequent as 40% and had a higher risk not only of BARC 3 or 5 bleeding but also of ischaemic events. The bleeding risk was proportional to the risk score and related to its individual components. The low positive predictive value of the ARC-HBR criteria for BARC 3 or 5 bleeding remains a notable limitation.
|
Impact on daily practice The application of the ARC-HBR criteria to identify BARC 3 or 5 bleeding at one year in patients undergoing PCI carries a high negative but low positive predictive value. The bleeding risk was related to its individual components. Physicians should note that an individualised approach may be needed based on the applied criteria. |
Conflict of interest statement
Y. Ueki reports personal fees from Infraredex, outside the submitted work. S. Bär reports grants from Medis medical imaging systems, outside the submitted work. S. Stortecky reports grants from Edwards Lifesciences, Medtronic and Abbott Vascular, grants and personal fees from Boston Scientific, and personal fees from BTG, outside the submitted work. T. Pilgrim reports grants and personal fees from Biotronik and Symetis/Boston Scientific, and grants from Edwards Lifesciences, outside the submitted work. M. Valgimigli reports grants and personal fees from Terumo, Abbott and AstraZeneca, grants from Medicure, personal fees from Chiesi, Bayer, Daiichi Sankyo, Amgen, Alvimedica, and Biosensors, outside the submitted work. S. Windecker reports grants from Abbott, Amgen, Bayer, Boston Scientific, Biotronik, BMS, Edwards Lifesciences, Medtronic, Sinomed, and Polares, outside the submitted work. L. Räber reports grants and personal fees from Abbott Vascular, Biotronik, Sanofi and Regeneron, personal fees from Amgen, AstraZeneca, Bayer, CSL Behring and Occlutech, and grants from HeartFlow, outside the submitted work. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.