Bleeding events impact negatively on prognosis in patients with acute coronary syndrome (ACS) whether they are undergoing percutaneous coronary intervention (PCI) or not1,2. Identifying high bleeding risk (HBR) patients has crucial implications for clinical and pharmacological management and for prognosis. Some trials assessing different stent platforms and dual antiplatelet therapy (DAPT) have been conducted or are ongoing in these delicate patients; however, the lack of standardisation in defining HBR patients inevitably limits trial design, data interpretation, and clinical decision making. The Academic Research Consortium for HBR (ARC-HBR) recently proposed criteria to standardise the definition of HBR for use in clinical trial recruitment3. After reaching consensus on an arbitrary HBR definition for Bleeding Academic Research Consortium (BARC) 3 or 5 bleeding of ≥4% or intracranial haemorrhage (ICH) of ≥1% at one year, and identifying risk factors for bleeding, the ARC-HBR classified these factors as major or minor criteria and proposed finally to define as having an HBR those patients with ≥1 major or ≥2 minor criteria3. Hence, these criteria represent an expert consensus based on the published literature; however, their acceptance and routine use unavoidably go through validation studies and, as a consequence, some studies have tested this definition and bleeding events in PCI patients (Figure 1),4,5,6,7,8,9,10,11, including the study by Nakamura et al9 presented in this issue of EuroIntervention.
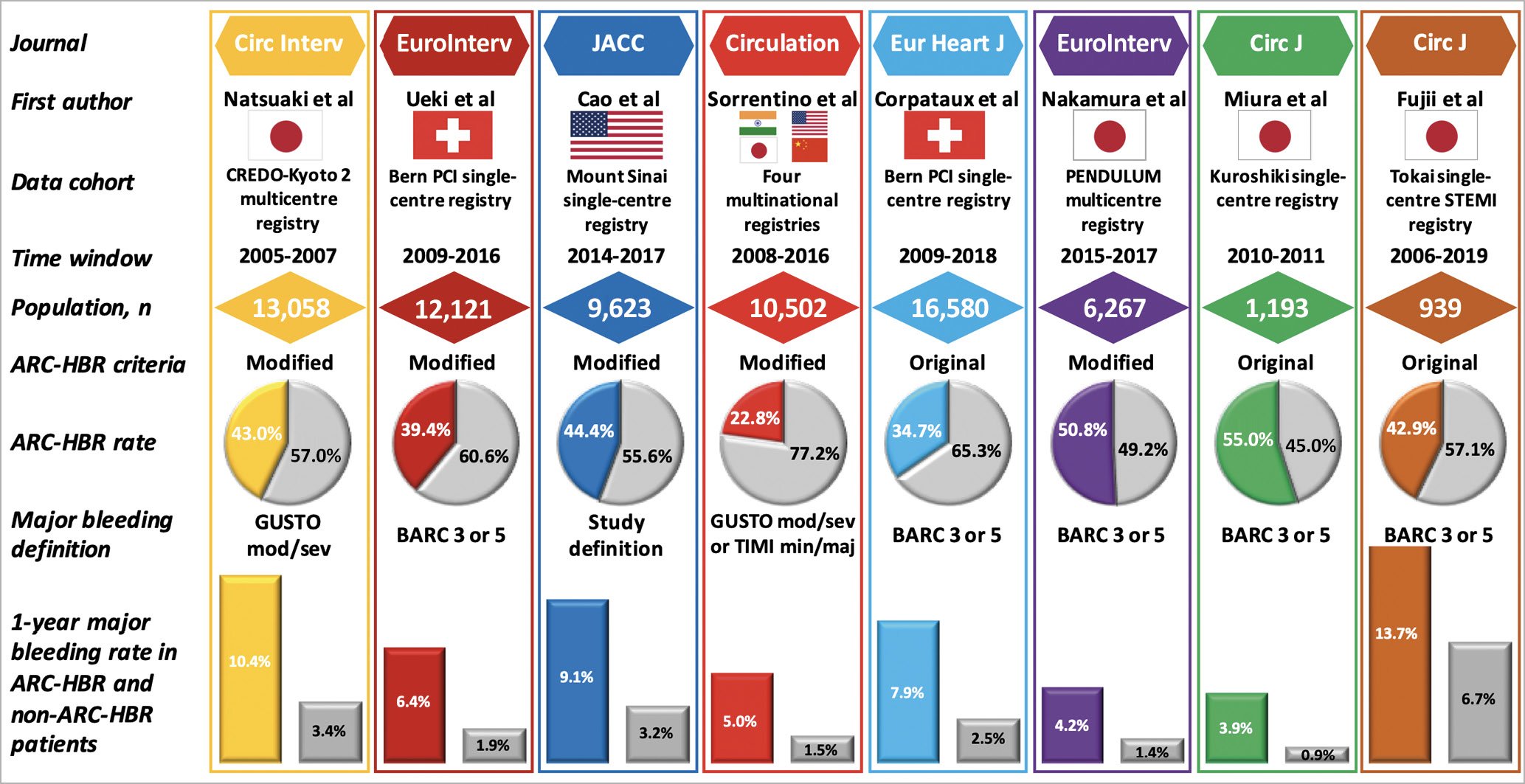
Figure 1. Studies of ARC-HBR criteria application. Notes: in Cao et al, study bleeding definition was a composite of periprocedural in-hospital bleeding (according to the data definitions of the National Cardiovascular Data Registry CathPCI Registry version 4.4) or post-discharge bleeding (any bleeding requiring either hospitalisation or blood transfusion). In Miura et al, the one-year bleeding rate was approximated by Kaplan-Meier curve.
PENDULUM is a prospective nationwide multicentre Japanese registry of PCI with contemporary PCI practice (radial access, new drug-eluting stents [DES], etc.) and pharmacologic treatments (DAPT type and duration, proton pump inhibitor [PPI] use, non-vitamin K antagonist oral anticoagulation [NOAC] use, no ticlopidine prescription). This analysis leverages a high-quality data set applying appropriate methodologies and reporting ischaemic and bleeding endpoints adjudicated with standard definitions by independent assessment committees. At 67 Japanese institutions, 6,267 patients undergoing PCI (from December 2015 to June 2017) were included. Mean age was 70 years, 78.3% were male and 32.2% presented with ACS. Among them, 3,185 (50.8%) were classified as ARC-HBR and were associated with a significant increase of BARC 3 or 5 bleeding events at one year (4.2% vs 1.4%; p<0.001) and a borderline increase of ICH (0.8% vs 0.5%; p=0.08).
Importantly, the majority of patients had overlapping criteria. Although the ARC-HBR definition was conceived as a binary definition and not as a score or quantitative tool, the authors calculated scores providing the insightful perspective that increasing scores determined increased bleeding risks, which is consistent with previous studies7,8. Also, interestingly, they found that the bleeding rate was 4.2% for one major criterion but 2.1% for two minor criteria, thus suggesting that the original categorisation into major/minor and the ARC-HBR definition might require further investigation.
This study represents a new important piece of evidence for several reasons. First, it expands the knowledge and evidence for ARC-HBR criteria in the delicate setting of Japanese people by providing nationwide, more generalisable and more contemporary data compared with other Japanese series (Figure 1). Compared with Western countries, East Asian patients are at greater bleeding risk, and dedicated data are of great clinical relevance. Second, this study consolidates the clinical value of the ARC-HBR criteria. In Japanese patients, ARC-HBR criteria well identified patients at high risk of bleeding. Despite the fact that overall bleeding rates were slightly lower than in other studies, which can be explained by different patient ethnicity, baseline characteristics, time period and clinical management, there was an almost threefold higher bleeding rate in HBR patients, consistently with other series (Figure 1). Yet, these criteria identified a large population of HBR patients, greater compared with almost all previous validation studies, most with multiple risk factors, which was associated with even greater bleeding risk, thus having important clinical implications. Third, this study provides new insights into the bleeding risk evaluation. The authors found that low body weight and heart failure could be of additional interest for the HBR definition, at least in Japanese patients, although when added to ARC-HBR criteria the bleeding prediction did not improve significantly. They also observed that ACS was an independent predictor of bleeding. This could represent an important hypothesis-generating finding. ACS patients are always considered to be at greater ischaemic risk needing more aggressive antithrombotic therapies, but the role of specific clinical presentations in bleeding risk is still debated12 and might require future clarification.
The results should be interpreted in the light of some study limitations that were properly acknowledged9. Like all other validation studies, this is a retrospective analysis; however, it applies to a prospective high-quality registry, limiting the bias related to its design. Like most of the other studies, it used modified criteria (among 11 major criteria, 3 were identical, 4 were modified and 4 not applicable; among 6 minor criteria, 2 were modified) compared with the original ones, because the authors used the prospectively collected available data without a retrospective implementation. This limits the availability of complete data, but prevents inaccuracy and underestimation related to retrospective collection/adjudication. The contribution of individual criteria on bleeding might be underestimated by the low number of patients with a single risk factor and the overall lower rate of bleeding compared with other series. Thus, the lower than 4% rate of BARC 3 or 5 bleeding for some factors should be interpreted with caution. Finally, bleeding risk is dynamic and affected by several aspects including antithrombotic therapy and modification of risk factors over time (i.e., renal dysfunction or anaemia). Although the authors provided data on DAPT, which is of additional value compared with some of the previous studies, this was not accounted for in the analysis, and the HBR status was only defined at baseline.
Doubtless, the ARC-HBR criteria will be fundamental for standardising definitions in clinical trials and helping data interpretation. Nakamura et al should be congratulated for providing key data consolidating the utility of the ARC-HBR definition even in daily practice, thus corroborating the intriguing perspective of its application to guide decision making. Future prospective validation studies accounting for contemporary alternative antithrombotic strategies (one-month DAPT, de-escalation, monotherapy, short triple therapy, etc.) or testing bleeding prevention strategies would represent a crucial step forward in this field.
Conflict of interest statement
G. Gargiulo reports consulting fees from Daiichi Sankyo, outside the submitted work. The other author has no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.