Bleeding is a challenging conundrum in cardiovascular medicine, especially in interventional cardiology, as it can arise from 2 different mechanisms: the local disruption of vascular or adjacent tissues at the access site during any invasive intravascular procedure, and the administration of antithrombotic drugs. The prognostic impact of major bleeding events is detrimental1, and the cardiology community has long strived to find strategies to minimise this risk, e.g., by recommending transradial over transfemoral access for percutaneous coronary interventions (PCI), avoiding routine pretreatment before invasive procedures, and tailoring long-term antithrombotic therapies based on individual risk profiles2. The latter aspect is critical because bleeding in an out-of-hospital setting eludes close clinical monitoring, and interventions to stop or control the bleeding may be significantly delayed. Hence, to provide patients undergoing interventional procedures with an optimal antithrombotic regimen, risk stratification becomes pivotal. The Academic Research Consortium (ARC) has proposed a set of clinical and laboratory parameters, subdivided into major and minor criteria, to effectively identify patients at high bleeding risk (HBR) after PCI3. Several validation studies have demonstrated a good predictive ability of these criteria in PCI cohorts, but similar evidence in those undergoing transcatheter aortic valve replacement (TAVR) is lacking45. Notably, risk stratification in a TAVR setting is increasingly important given its expanding indications, growing adoption of minimalistic approaches (e.g., same-day discharge), and ongoing controversies regarding optimal antithrombotic management.
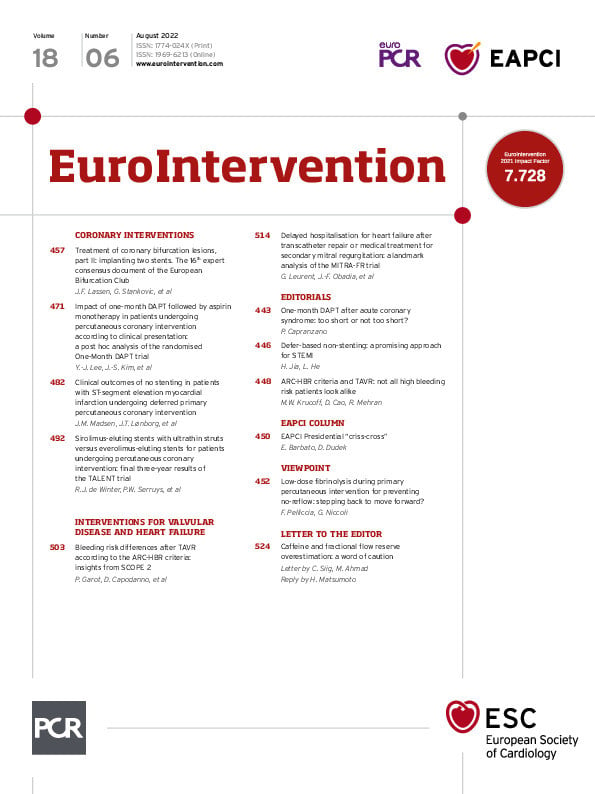
In this issue of EuroIntervention, Garot et al6 highlight the results of a validation study of the ARC-HBR criteria among 796 high-risk patients undergoing transfemoral TAVR from the SCOPE 2 trial, which was a randomised comparison of 2 self-expanding, supra-annular bioprostheses (ACURATE neo [Boston Scientific] versus CoreValve Evolut R [Medtronic]). The trial included only patients who were ≥75 years old and deemed to be at an increased risk for surgical mortality. This translated into a very high prevalence (80.4%) of subjects satisfying the ARC-HBR definition (i.e., presence of at least 1 major or 2 minor criteria) which is approximately double of that reported in all-comer PCI cohorts45. Unsurprisingly, HBR patients presented with a higher burden of comorbidities and estimated Society of Thoracic Surgeons perioperative risk of mortality (STS-PROM: 4.9% vs 3.3%) than their non-HBR counterparts. At 1-year follow-up, mortality was nearly 3 times as high among HBR versus non-HBR patients (12.4% vs 4.3%; p=0.0002), with an increase in both cardiac and non-cardiac fatalities. Hospitalisation for valve-related symptoms or worsened congestive heart failure was also increased, with nonsignificant, yet consistent numerical trends for other secondary ischaemic endpoints. These differences notwithstanding, the 1-year incidence of Bleeding Academic Research Consortium (BARC) type 3 or 5 bleeding was comparable in patients with and without HBR (7.7% vs 6.1%; p=0.46), regardless of concomitant oral anticoagulant therapy. Only access site-related bleeding was higher in HBR patients, likely due to more vascular complications consequent to a higher degree of iliofemoral calcifications and tortuosity, and more frequent use of anticoagulant therapy.
Altogether, the present study suggested that the ARC-HBR criteria developed for a PCI population are not useful to stratify the bleeding risk after TAVR. A substudy from the POPular TAVI trial has yielded similar results, with 78.5% of patients meeting the ARC-HBR definition and no significant differences in major or life-threatening bleeding (10.8% vs 6.6%; p=0.08)7. The apparent lack of predictive value of the ARC-HBR criteria in a TAVR setting may have different explanations. Firstly, the average TAVR population is much older and sicker than the one undergoing PCI, such that even patients formally classified as non-HBR still exhibit a residual bleeding risk. In fact, both the HBR and non-HBR groups exceeded the conventional 4% cut-off for 1-year BARC 3 or 5 bleeding. Secondly, owing to the SCOPE 2 trial design, nearly all patients were aged 75 years or more and 4 out of 5 fulfilled the ARC-HBR definition. Therefore, a ceiling effect, due to a large proportion of subjects receiving a high score, is plausible, rendering a binary definition of HBR unable to discriminate between subjects at either end of the scale8. Supporting this observation, the POPular TAVI substudy showed a significant trend towards increased bleeding by progressively adding multiple criteria7. Thirdly, determinants of bleeding risk may be different in an elderly and frail population, such as the TAVR one. The recently developed PREDICT-TAVR bleeding risk score identified 6 variables collected as part of the pre-TAVR workup9. Among those, only 3 (i.e., oral anticoagulation, haemoglobin levels, and creatinine clearance) overlapped with the ARC-HBR criteria. Moreover, PREDICT-TAVR, being an integer point-based risk score, may be able to better discriminate across a broad spectrum of high-risk patients. Lastly, both the SCOPE 2 and POPular TAVI substudies attempted to validate the ARC-HBR criteria in relatively small cohorts (<1,000 patients) with an inherent risk of a type II error.
In conclusion, the analysis by Garot et al reminds us that, as we move towards individualised medicine, one risk score does not fit all. While simplicity and usability remain cornerstones for promoting uptake in clinical practice, these features should not be mistaken for a simplistic approach to patient risk assessment and management. Larger investigations evaluating the contribution of individual ARC-HBR criteria and other bleeding risk parameters in a TAVR setting are needed as valve technologies and procedures evolve and indications broaden to include lower-risk subgroups.
Conflict of interest statement
R. Mehran reports institutional research grants from Abbott, Abiomed, Applied Therapeutics, Arena, AstraZeneca, Bayer, Biosensors, Boston Scientific, Bristol Myers Squibb, CardiaWave, CellAegis, CERC, Chiesi, Concept Medical, CSL Behring, DSI, Insel Gruppe AG, Medtronic, Novartis Pharmaceuticals, OrbusNeich, Philips, Transverse Medical, and Zoll; personal fees from ACC, Boston Scientific, California Institute for Regenerative Medicine (CIRM), Cine-Med Research, Janssen, WebMD, and SCAI; consulting fees paid to the institution from Abbott, Abiomed, AM-Pharma, Alleviant Medical, Bayer, Beth Israel Deaconess, CardiaWave, CeloNova, Chiesi, Concept Medical, DSI, Duke University, Idorsia Pharmaceuticals, Medtronic, Novartis, and Philips; holding equity <1% in Applied Therapeutics, Elixir Medical, STEL, and CONTROLRAD (spouse); and being a member of the Scientific Advisory Board for AMA, and Biosensors (spouse). The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.