Abstract
Aims: The aim of this study was to evaluate the prevalence of triple antithrombotic therapy (TT) (warfarin, aspirin and clopidogrel) in patients following an acute coronary syndrome (ACS), the bleeding risk compared to double antiplatelet therapy (DAPT) (aspirin and clopidogrel) and evaluate the accuracy of the HAS-BLED risk score in predicting serious bleeding events in TT patients.
Methods and results: We retrospectively identified all ACS patients on TT upon discharge from the Coronary Care Unit at Skane University Hospital between 2005 and 2010. TT patients were compared to age- and sex-matched control patients discharged with DAPT. Major bleeding was defined in accordance with the HAS-BLED derivation study. A total of 2,423 patients were screened, of whom 159 (6.6%) were on TT. The mean age was 67.2 (±0.9) years. The most common indication for TT was atrial fibrillation (n=63, 39.6%) followed by apical akinesia (n=60, 37.8%), and the mean duration of TT was 3.7 (±0.3) months. Upon termination of TT, warfarin was discontinued in 82 (52.2%) patients and clopidogrel in 57 (36.3%) patients. The cumulative incidence of spontaneous bleeding events was significantly higher with TT compared to DAPT at one year (10.2% vs. 3.2%; p=0.01). The HAS-BLED score significantly predicted spontaneous bleeding events in TT patients (area under the receiver operating characteristic [ROC] curve 0.67; 95% CI=0.54-0.79; p=0.048).
Conclusions: TT was relatively common following acute coronary syndrome and was associated with a threefold increase in major bleeding compared to DAPT at one year. The HAS-BLED risk score predicted bleeding events with moderate accuracy.
Introduction
Warfarin monotherapy has been the mainstay of oral anticoagulant treatment for patients with cardiac conditions such as atrial fibrillation, prosthetic heart valves and reduced left ventricular function with and without left ventricular thrombus formation. Moreover, it has been a cornerstone in the treatment of non-cardiac conditions such as deep vein thrombosis and pulmonary embolism.1 The efficacy in preventing thromboembolic complications is well established in a wide range of clinical settings. The same observation is true concerning the the risk of bleeding complications.2
A major clinical problem that is currently unresolved concerns patients with an indication for warfarin treatment but who also have an indication for antiplatelet treatment due to intercurrent coronary disease.1 Aspirin has been widely used since the 1980s for secondary prevention in coronary disease patients, and has received a class 1 indication in clinical practice guidelines.3-5 The major risk with aspirin is bleeding,6 and bleeding risks have become even more prominent with the advent of dual antiplatelet therapy (DAPT) (aspirin in combination with clopidogrel).7,8 Concurrent medication with warfarin, aspirin and clopidogrel is termed triple antithrombotic therapy (TT). Bleeding risk with TT is likely to be substantially higher than with DAPT. However, patients with DAPT and prolonged warfarin interruption in this setting have a threefold increase in stroke or thromboembolic events,1 and DAPT is associated with lower rates of death and myocardial infarction compared to aspirin and warfarin alone.8 Therefore, current European and American guidelines recommend TT,9,10 and a recent survey showed common TT use throughout Europe.11
One strategy to avoid serious bleeding events in TT is the identification of individuals at increased bleeding risk, i.e., in whom TT use may be inappropriate. A working group of the European Society of Cardiology recommends the use of the HAS-BLED score to identify patients at high risk of bleeding.12,13 However, this bleeding risk score has not been evaluated in patients with TT after an acute coronary syndrome (ACS).
The aim of this study was to evaluate the prevalence of TT in patients following an ACS, the bleeding risk compared to DAPT and evaluate the prognostic accuracy of the HAS-BLED risk score in predicting bleeding events in TT patients.
Methods
STUDY SAMPLE
All patients over 18 years of age from the Lund municipality treated at the Coronary Care Unit at Skane University Hospital between 2005 and 2010 for an acute coronary syndrome were retrospectively screened for TT at discharge. For each identified patient, an age- and sex-matched control patient with DAPT at discharge was identified in a randomised and blinded manner. Eligible patients were identified from the RIKS-HIA registry (Register of Information and Knowledge About Swedish Heart Intensive Care Admissions), which includes detailed information on all patients treated at Swedish coronary care units as described previously.14
STUDY DEFINITIONS
Mortality data was extracted from the Swedish National Registry. All other data was gathered from the patients’ hospital medical records, including baseline characteristics and follow-up data. Patients were followed for 12 months by retrospective review of records, for bleeding events, thromboembolic events and medication changes. Major bleeding during follow-up was defined according to the HAS-BLED derivation study, i.e., any bleeding requiring hospital care and/or causing a decrease in haemoglobin level of more than 20 g/L and/or requiring blood transfusion and/or with intracranial location.12 Thromboembolic events were defined as a physician’s diagnosis of stroke, transient ischaemic attack (TIA), ACS or peripheral arterial embolism.
The HAS-BLED score was calculated for each individual. One point was assigned for each of the following: hypertension, abnormal hepatic or renal function (maximum two points), stroke, bleeding history or predisposition, labile international normalisation ration (INR), elderly (>65) and drugs/alcohol concomitantly (antiplatelet agents or non-steroidal anti-inflammatory drugs; 1 point for drugs plus 1 point for alcohol excess, maximum 2 points).12 CHADS2VA2Sc was used for thromboembolic risk stratification in atrial fibrillation patients.15
STATISTICAL ANALYSIS
Data analysis was performed with SPSS Statistics (Version 19; SPSS Inc., Chicago, IL, USA) software. Treatment groups were compared for differences in baseline characteristics by the chi-square test for categorical variables and by the Student’s t-test for continuous variables. The incidence of major bleeding was calculated using the Kaplan-Meier estimator, and differences between treatment groups examined with the log-rank test. The prognostic accuracy of the HAS-BLED score was evaluated by the area under the receiver operating characteristic (ROC) curve. Statistical significance was accepted at p<0.05 (two-sided).
Results
A total of 2,423 patients were screened for eligibility from January 2005 until December 2009. Of those, 159 (6.6%) patients with TT upon discharge were identified, along with 159 age- and sex-matched control patients with DAPT upon discharge.
BASELINE CHARACTERISTICS
The baseline characteristics of the patients are presented in Table 1. All characteristics except the number of individuals with ST-elevation myocardial infarction (STEMI) and heart failure were similar between the groups.
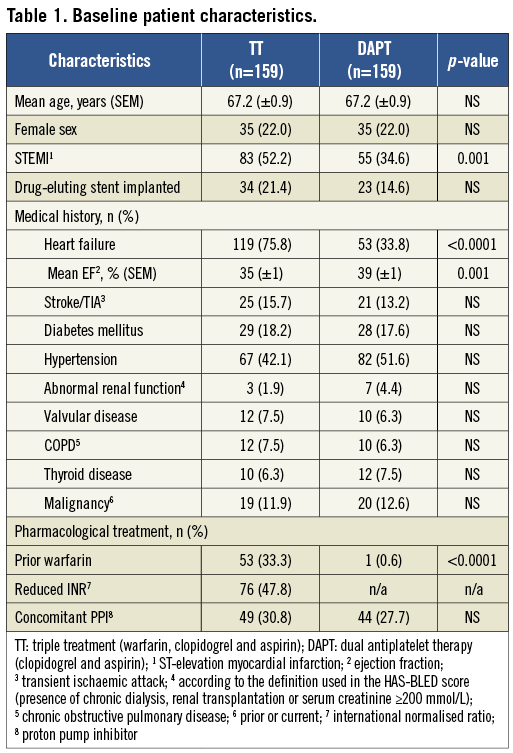
All patients were treated with 75 mg of aspirin and 75 mg of clopidogrel once daily. For patients on warfarin treatment, target international normalised ratio (INR) was between 2.0 and 3.0 unless otherwise specified (Table 1). The duration of TT was decided by the attending physician, after which the drug considered least important was discontinued. All patients on DAPT were planned for 12 months of continuous treatment, after which clopidogrel or aspirin was discontinued at the discretion of the attending physician.
The most common indication for TT was atrial fibrillation (n=63, 39.6%) followed by apical akinesia (n=60, 37.8%), left ventricular thrombus (n=17, 10.7%), presence of a mechanical valve (n=6, 3.8%), venous thromboembolism (n=11, 6.9%) and other causes (n=2, 1.3%).
OUTCOMES
The outcomes at one year are presented in Table 2 and Figure 1. The cumulative incidence of spontaneous major bleedings was significantly higher in the TT group at one year (10.2% vs. 3.2%; p=0.01). The median exposure time to TT was three months. Therefore, the bleeding risk associated with TT was further evaluated at that time-point and a significantly higher incidence of spontaneous bleedings in patients on TT was observed (6.6±0.2% vs. 1.9±0.1%; p=0.02).


Figure 1. Spontaneous bleeding. Closed circles in the TT group represent bleeding in patients subsequent to discontinuation of triple antithrombotic therapy (n=2). Both patients were on dual antiplatelet therapy at the time of bleeding and were censored in the analysis of bleeding while on TT.
Four TT patients and one DAPT patient were examined by a physician at the emergency ward because of bleeding that was limited in nature and did not result in further investigation or treatment. These events were adjudicated as minor bleeding and disregarded in the analysis.
Three patients in the DAPT group were prescribed warfarin during the follow-up period. They were censored from the statistical analysis at the initiation of treatment.
Site-specific time in therapeutic INR range (TTR) was 75.8% for the studied time period. Fourteen percent of the patients (2/14) with spontaneous bleeding on TT were above the therapeutic range at the time of bleeding.
Analyses of the thromboembolic endpoints (peripheral embolism, stroke/TIA and acute coronary syndrome) revealed no differences between the groups (Table 2). A composite of all thromboembolic endpoints was also similar between the groups (5.7% vs. 3.2%; p=0.27; TT vs. DAPT).
PREDICTION OF OUTCOMES
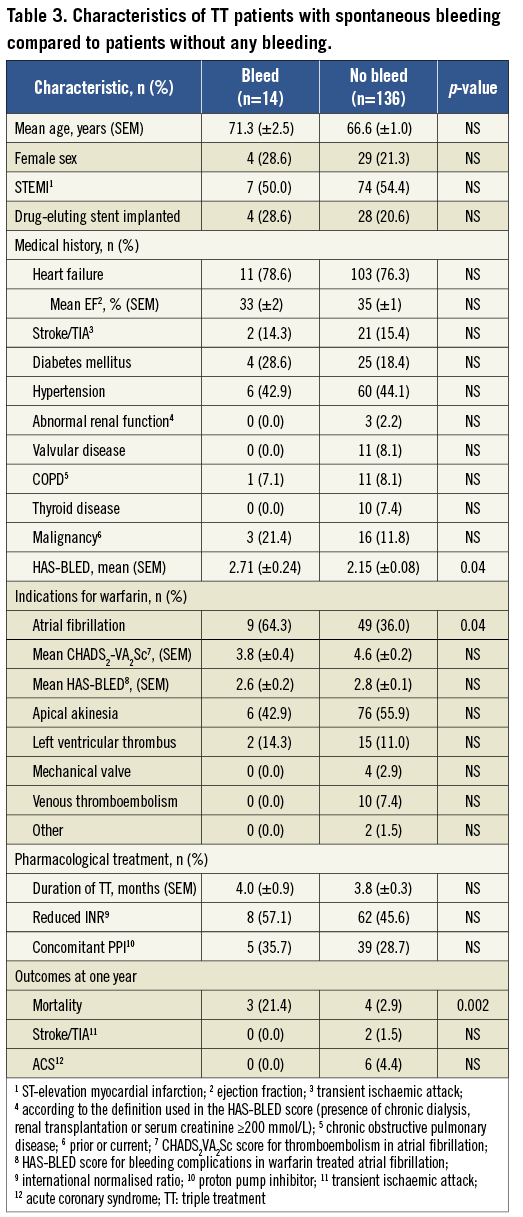
A comparison between patients with spontaneous major bleeding and those without any bleeding while on TT is presented in Table 3. All baseline characteristics were similar between the groups apart from the presence of atrial fibrillation, which was more common among patients with spontaneous bleedings (9 [64.3%] vs. 49 [36.0%]; p=0.04). Mean HAS-BLED score was higher among TT patients with spontaneous bleeding (2.71±0.24 vs. 2.15±0.08; p=0.04), as was the mortality at one year (3 [21.4%] vs. 4 [2.9%]; p=0.002). The predictive accuracy of the HAS-BLED score was modest, with an area under the ROC curve of 0.67 (95% CI 0.54-0.79; p=0.048).
Discussion
In this study, we found that 7% of patients treated for an ACS were discharged with TT during a five-year period. Upon termination of TT, warfarin was discontinued in about half of the patients, reflecting that a common indication for TT was apical ventricular akinesia. The incidence of all major bleeding was threefold higher in TT patients compared to age- and sex-matched control patients on DAPT, driven mainly by gastrointestinal bleeding. All-cause mortality during follow-up was higher in patients with major bleeding. The HAS-BLED score was significantly higher in patients with major bleeding during one year of follow-up and predicted bleeding events with modest accuracy. Our results have several implications:
OUTCOMES
The proportion of patients on TT in the current study may appear high, but was in line with recent estimations that 5-7% of patients undergoing percutaneous coronary interventions have indications for chronic oral anticoagulant therapy.9 This number is expected to increase with the aging population and an increasing prevalence of atrial fibrillation.16
A small number of studies have examined bleeding rates in TT patients. Although bleeding rates are consistently greater compared to that in DAPT patients, risk estimates vary in magnitude.1,17-20 We observed a threefold increase at one year, similar to a previous Danish study,21 but slightly higher compared to a meta-analysis of the literature.22 The difference could be explained by a wider definition of major bleeding in the current study, as well as an increased sensitivity using a method based on medical records compared to methods based on medical diagnosis registries. The increase in spontaneous major bleeding events was driven mainly by gastrointestinal bleeding in the current study, consistent with results from previous investigations. However, we also observed a numerically higher incidence of intracranial and fatal bleedings. The incidence of major bleeding in DAPT patients was in line with the CURE study and other trials on dual antiplatelet therapy.7,8
The increased mortality observed in patients with bleeding was expected, since multiple trials have demonstrated a correlation between bleeding and mortality in patients with coronary disease.9,23,24 The time in therapeutic INR range was high compared to prospective randomised trials of warfarin treatment,25 and only two patients were over the therapeutic limit at the time of bleeding.
From previously published studies, it seems that patients with indications for TT who only receive DAPT, have a threefold increase in thromboembolic events.1 This observation is in contrast to the equal rates of thromboembolism in TT and DAPT patients in the current study, indicating a firm preventive effect of such events by TT.
PREDICTION OF OUTCOMES
The predictive accuracy of the HAS-BLED risk schema was initially investigated in a cohort from the Euro Heart survey on atrial fibrillation, where a subgroup of patients was medicated with warfarin and an antiplatelet agent.12 The area under the ROC curve was found to be 0.78 (95% CI 0.65-0.91) in this subgroup. The HAS-BLED score was subsequently validated in the warfarin-treated control group from the SPORTIF III and V trials of ximelagatran in atrial fibrillation.26 In participants on warfarin plus aspirin concurrently in the validation study, a lower area under the ROC curve of 0.60 (95% CI 0.53-0.68) was noted.26 Thus, the ROC value of 0.67 observed in TT patients in the current study was similar to other settings with warfarin.
Short TT treatment duration in combination with low dose aspirin and clopidogrel, a reduced INR target and proton pump inhibitor (PPI) therapy have been proposed as measures aimed at reducing bleeding complications in TT patients.1,9 Although this advice appears well founded, the current study mainly underlines the importance of careful patient selection and keeping treatment duration as short as possible.
The novel oral anticoagulants that are currently being introduced into clinical practice generally demonstrate a similar efficacy in preventing thromboembolism compared to warfarin at a reduced rate of major bleeding,27-29 and thus appear attractive in a TT setting. However, the lack of commercially available reversal agents may limit the usability. Moreover, the increase in gastrointestinal bleeding associated with dabigatran in the RE-LY trial raises concerns in a TT context since this type of haemorrhage drove the increase in major bleeding observed in the current study. The third generation of P2Y12 antagonists also increase the incidence of major bleeding compared to clopidogrel,30,31 conceivably limiting their use in TT.
Limitations
This study was designed as a retrospective, monocentric, medical record-based analysis with the limitations inherent to such study designs. However, since no prospective evaluation of the HAS-BLED score has been performed in this context, we believe the results of the current study are important for correct handling of TT patients after an ACS, and for further refinement of bleeding risk stratification tools.
Conclusions
In conclusion, TT was relatively common following an ACS and associated with a threefold increase in the incidence of spontaneous major bleeding at one year compared to DAPT. The HAS-BLED score predicted bleeding events with moderate accuracy, similarly to other settings with warfarin. Careful patient selection, potentially supported by HAS-BLED, and short treatment duration appears warranted.
Acknowledgements
The authors wish to thank Ewa Mattsson, registered nurse, for identifying eligible patients in the RIKS-HIA registry.
Funding
The work was performed at the Coronary Care Unit, Skane University Hospital, Lund, Sweden; and funded by the Department of Clinical Sciences, Faculty of Medicine, Lund University, Lund, Sweden.
Conflict of interest statement
The authors have no conflicts of interest to declare.

