Transcatheter aortic valve implantation (TAVI) for pure aortic valve regurgitation (AR) with off-label devices is challenging because of the increased risk for transcatheter heart valve (THV) embolisation or migration and paravalvular leak in the absence of aortic valve calcification1. The Trilogy transfemoral TAVI system (JenaValve) recently received a CE (European Conformity) mark for the treatment of aortic regurgitation and aortic stenosis. It features unique locators that align the THV with the native cusps of the valve and enables anchoring in pure AR patients. Early data on the Trilogy valve in AR patients have shown promising results (Tamm AR, et al. JenaValve Trilogy for treatment of aortic regurgitation: worldwide first results. EuroPCR 2022. Paris, France).
Our patient, a 69-year-old female with worsening symptoms of heart failure (NYHA Class III) was referred to our institution because of severe AR. She had a history of surgical mitral valve repair five years earlier and persistent atrial fibrillation. Echocardiography showed a severely reduced left ventricular ejection fraction, dilation of the left ventricle and severe AR due to a left coronary cusp (LCC) perforation (Figure 1A, arrow, Figure 1B, Moving image 1). This finding was also demonstrated on cardiac computed tomography (Figure 1C, arrow) and was possibly the result of an iatrogenic injury of the cusp during mitral surgery. Our interdisciplinary Heart Team decided on an interventional approach due to the high risk for redo surgery (EuroSCORE II 9.14%). Because of the anatomical pathology of pure AR and the limitations of the other available devices, we chose the Trilogy transfemoral TAVI system. Unlike other prostheses, this THV does not need sclerosis or calcification for anchoring in the annulus; it utilises dedicated “locators” which are placed in each of the cusp sinuses to “clip” the THV to the native leaflets, thus anchoring the valve in place (Figure 1G). Prior to deployment, the THV is rotated and anatomically aligned using an integrated mechanism on the delivery system handle (Figure 1H). We chose a 27 mm prosthesis and the procedure was performed under conscious sedation using fluoroscopic guidance. The THV locators were directed into each coronary cusp and correct positioning was confirmed using multipurpose (MP) and Amplatz left (AL-1) catheters. The locator in the LCC protruded through the cusp perforation into the left ventricular outflow tract (Figure 1D, asterisk). Since the other two locators were safely placed in the nadirs of the right coronary cusp and the non-coronary cusp, the valve could be implanted successfully. Post-implant aortography showed no signs of AR (Figure 1E, Moving image 2), which was confirmed in the post-procedural echocardiography (Figure 1F, Moving image 3). The patient was discharged early without any complications.
The standard treatment for symptomatic severe AR is surgical aortic valve replacement. However, according to the guidelines, TAVI may be considered in experienced centres for selected patients2. At present, the JenaValve Trilogy is the only THV with CE mark approval for patients with severe AR at high surgical risk. In this special case, there was an elevated risk of implantation failure due to rupture of the perforated left coronary cusp. Therefore, an exact positioning of the THV using extended fluoroscopy guidance was mandatory. The data on the efficacy and safety of the JenaValve Trilogy TAVI system are still limited (idem Tamm AR et al), so further studies are needed to show outcomes in patients with severe AR and challenging anatomy.
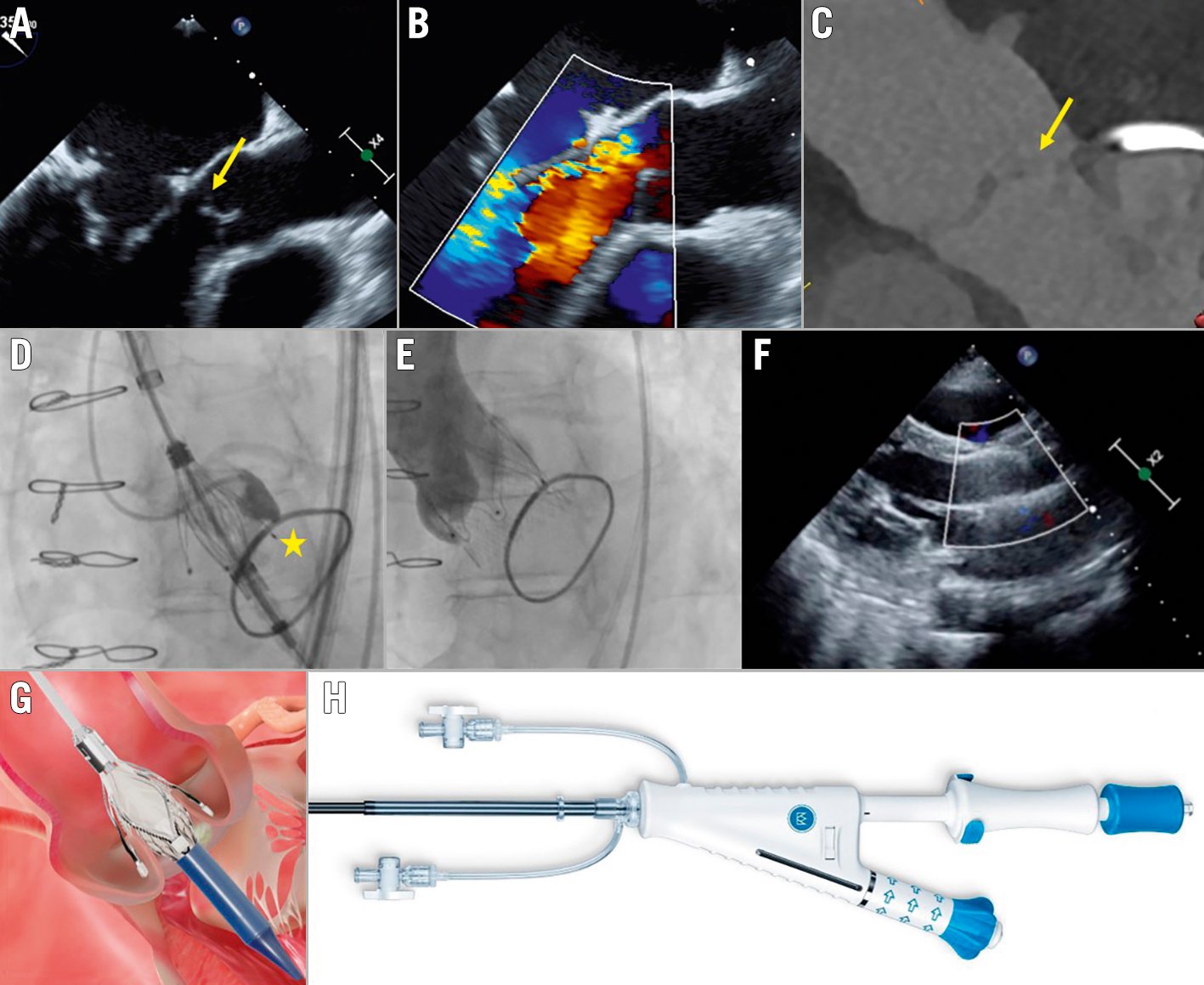
Figure 1. Trilogy TAVI system for severe aortic regurgitation. A-B) Transoesophageal echocardiography at baseline showing LCC perforation (arrow). C) Cardiac computed tomography multiplanar reconstruction showing LCC perforation (arrow). D) The position of the THV and every coronary cusp was confirmed with contrast in fluoroscopy, THV locator protruding through perforated LCC (asterisk). E) Post-implant aortography showing no AR. F) Post-procedural transthoracic echocardiography demonstrating no AR. G) The locators of the THV are placed in the cusp sinuses to ensure anchoring when the valve is deployed. H) The integrated rotation on the delivery system handle allows for alignment of the THV. Panels G and H: reproduced with permission from JenaValve Technology. AR: aortic regurgitation; LCC: left coronary cusp; TAVI: transcatheter aortic valve implantation; THV: transcatheter heart valve.
Conflict of interest statement
A.R. Tamm reports proctoring and lecture honoraria from JenaValve Technology, Edwards Lifesciences and Medtronic. H. Treede is a proctor and consultant for JenaValve Technology. R.S. von Bardeleben has received consultancy and lecture honoraria from Abbott Structural Heart and Edwards Lifesciences. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Transoesophageal echocardiography at baseline showing cusp perforation and severe aortic regurgitation.
Moving image 2. Aortography after Trilogy THV implantation showing no paravalvular regurgitation.
Moving image 3. Transthoracic echocardiography before discharge showing no paravalvular regurgitation.