Abstract
Aims: The Tryton bifurcation stent has been developed to improve clinical outcomes after treatment of bifurcation lesions. Limited data are available on the use of the Absorb bioresorbable vascular scaffold (BVS) in bifurcation lesions with side branches >2 mm. We present here the acute procedural results and midterm clinical follow-up of the first-in-man combined use of the Tryton stent and the Absorb scaffold for the treatment of complex bifurcation lesions.
Methods and results: Ten patients treated with the Tryton stent in combination with Absorb BVS were included in the current report. Offline two- and three-dimensional optical coherence tomography (OCT) analyses were performed to gain more insights into this novel approach. Procedural success was 91%, whereas angiographic success was achieved in 82%. Two TLRs occurred (TLR rate 20%), whereas no deaths, myocardial infarctions or stent thromboses were observed up to six months of follow-up.
Conclusions: We present a new treatment strategy in complex bifurcation lesions using the Tryton stent in combination with the Absorb BVS. This approach potentially offers an opportunity to treat complex bifurcation lesions with the Absorb BVS. Furthermore, three-dimensional OCT reconstructions give valuable insights into PCI of complex bifurcation lesions.
Introduction
Based on multiple randomised trials comparing single with two-stent techniques1, provisional single stenting is considered as the default treatment strategy in coronary bifurcation lesions2. Recently, this current dogma has been criticised, because patients with extensive side branch (SB) involvement, requiring proper revascularisation of the SB, were most likely excluded from these trials, while on the other hand patients without SB involvement were included with a 50% chance of being randomised to an unnecessary complex two-stent treatment strategy3,4.
Therefore, it is still important to improve two-stent treatment strategies for complex bifurcation lesions in which the SB is involved. The Tryton Side Branch Stent (Tryton Medical, Inc., Durham, NC, USA) is a dedicated bifurcation stent which has been developed to improve clinical outcomes after percutaneous coronary intervention (PCI) of bifurcations5. The device is an SB first stent, which is used in combination with a main branch (MB) stent, and thus could be considered as a modified culotte technique. Its specific design offers some potential advantages over other two-stent techniques, such as fewer layers of non-apposed stent struts in the SB ostium opposite to the carina when compared with the crush technique6, or less SB stent distortion and better MB stent apposition compared with the classic culotte technique7. Multiple registries and a patient-level pooled analysis including 900 patients have shown promising results after bifurcation treatment with the Tryton stent5,8-11.
In the vast majority of the patients included in these registries, a regular drug-eluting stent (DES) was used as the MB stent. We have used the Absorb (Abbott Vascular, Santa Clara, CA, USA) bioresorbable vascular scaffold (BVS), which has become commercially available in Europe, as the MB stent. The rationale behind this is that the use of BVS potentially improves clinical outcomes after PCI of bifurcation lesions because, after complete BVS resorption: 1) the potential trigger for late stent thrombosis (ST) is eliminated, and 2) jailed non-apposed SB struts can no longer cause late restenosis at the SB ostium as metallic stents do12. Although the use of two BVS might be ideal, the crush or classic culotte techniques using two BVS are conceptually limited due to the inability to post-dilate the BVS with large balloons, potentially causing strut fractures. Furthermore, they will have the same limitations concerning the number of non-apposed stent struts as with conventional DES mentioned above.
The most obvious limitation of the combined use of Tryton stent/Absorb scaffold is the concern that the proximal MB zone of the Tryton stent will not have enough radial strength, potentially leading to late recoil/in-stent restenosis once the Absorb scaffold is resorbed. However, a previous publication showed the successful treatment of Medina 0,0,1 lesions with the Tryton stent alone13. It could be argued that the BVS covering the Tryton stent in the MB will be endothelialised before its resorption, embedding the Tryton stent in the MB vessel wall.
In the current report we will present the procedural characteristics, including two- and three-dimensional optical coherence tomography (OCT), acute angiographic results and midterm clinical follow-up of ten patients treated with a Tryton stent/Absorb scaffold two-stent approach for the treatment of complex bifurcation lesions.
Methods
DEVICES
The Tryton Side Branch Stent has been described previously5. In short, it is a 5 or 6 Fr compatible balloon-expandable cobalt-chromium bare metal stent consisting of three zones: 1) a distal zone scaffolding the SB; 2) a proximal MB zone with two “wedding bands” and three fronds to anchor the stent in the MB while minimising the amount of metal in the MB; and 3) a transition zone in between with three panels scaffolding the SB ostium. The stent is positioned using four radiopaque markers on the delivery system. After its deployment, an MB stent is placed from the proximal-to-distal MB through the stent and should cover its whole proximal part, including both wedding bands, to provide sufficient radial strength to the proximal MB and to ensure drug elution in the entire stented area of the MB. It is recommended by the IFU to finalise with final kissing balloon inflation (FKBI), although in daily clinical practice FKBI is successfully performed in only 80% of cases11.
The Absorb BVS is laser cut from a tube of the poly (L-lactic) acid (PLLA) polymer and is coated with a thin layer of drug/polymer matrix comprised of an everolimus and poly (D,L-lactic) acid polymer (PDLLA) mixture in a 1:1 fashion. Two platinum radiopaque markers are incorporated in the BVS to facilitate accurate positioning, since the PLLA itself is radiolucent. In the current study, the second-generation BVS was used (Revision 1.1), which is currently commercially available in Europe. This BVS consists of 157 μm thick struts. The struts are aligned in-phase and linked by three bridges, similar to the XIENCE V (Abbott Vascular) design. The PLLA backbone of the BVS degrades slowly over 18 to 24 months, whereas the drug/polymer matrix is completely resorbed in nine months.
SETTING AND PATIENT POPULATION
Our centre, the Academic Medical Center - University of Amsterdam, is a large tertiary referral centre with an annual PCI volume of ~2,000 procedures. The Tryton stent was introduced in our centre in October 2010 and the Absorb BVS became available for commercial use in September 2012. All operators were trained to use both devices according to the IFU. OCT use in our centre was at the discretion of the operator, although at least one final pullback was obtained in all patients treated with the Tryton stent/Absorb scaffold combination. The study cohort consisted of consecutive patients who underwent PCI of a bifurcation lesion in our centre between January and July 2013, in whom an attempt was made to perform a PCI using the Tryton Side Branch Stent in combination with the Absorb BVS in the MB.
DATA ACQUISITION
Offline pre- and post-procedural quantitative coronary angiography (QCA) analyses were performed using dedicated bifurcation software (QAngioXA version 7.3; Medis, Leiden, The Netherlands). All OCT pullbacks were obtained with the C7-XR frequency domain system (St. Jude Medical, St. Paul, MN, USA). The OCT imaging catheters (St. Jude Medical) were advanced over a 0.014-inch conventional guidewire. Pullbacks were performed during a continuous X-ray contrast injection of 4 ml/s at a maximum pressure of 300 psi using an injection pump. Images were acquired at 100 frames/s and the pullback speed used was 10 or 20 mm/s, at the discretion of the operator. After acquisition, the images were calibrated based on the reflection of the imaging catheter. Two-dimensional (2D) OCT analyses were performed offline with the C7 system (St. Jude Medical) by using the final pullbacks made in the MB. Three-dimensional (3D) OCT images were reconstructed using volume-rendering software (Amira software; Visualization Sciences Group, an FEI Company, Burlington, MA, USA). First, every single strut was detected by hand in each OCT cross-section (Absorb and Tryton struts were detected separately). Then, the reflection of the imaging catheter was filtered out in each frame. Finally, the 3D images were reconstructed using the calculated longitudinal resolution (pullback speed divided by frame rate, i.e., 0.2 mm [20 mm/s divided by 100 frames/s] or 0.1 mm [10 mm/s divided by 100 frames/s]). All patients were contacted by phone at six months to obtain clinical follow-up.
DEFINITIONS
Device success was defined as successful deployment of intended stents (both Absorb scaffold and Tryton stent) without device-related complications. Angiographic success was defined as <30% residual stenosis and TIMI 3 flow in both MB and SB post procedure in the lesions in which the Absorb and Tryton devices were placed at the intended site. Procedural success was defined as angiographic success without in-hospital major adverse cardiac events (MACE).
Clinical outcomes were reported as cardiac death, any recurrent myocardial infarction (MI), target lesion revascularisation (TLR), stent/scaffold thrombosis (ST), and target lesion failure (TLF), defined as the composite of cardiac death, recurrent MI and TLR.
Angiograms with matched views before and after the procedure were selected for analysis. In-stent and in-segment (in-stent plus 5 mm edges) minimal lumen diameter (MLD) and diameter stenosis were assessed for the proximal MB, distal MB, and SB separately, as well as for the ostial (first 3 mm from the carina) distal MB and SB. Acute gain was calculated by extracting pre- from post-procedural MLD. Two-dimensional bifurcation angles were also assessed pre- and post-procedure. Bifurcation lesions were classified using the Medina classification14.
The 2D OCT analyses were assessed for the proximal MB, distal MB, and SB region separately. Analyses were performed in 1.0 mm intervals (proximal and distal MB) or 0.2 mm intervals (SB region). The lumen area was drawn following the endoluminal vessel wall contour. The scaffold area was drawn following the endoluminal side of the polymeric struts15. Struts were classified as well-apposed or as incompletely apposed. Well-apposed struts were further divided into protruded and embedded struts. Embedded struts were defined as struts with more than half the thickness of the strut being impacted into the vessel wall. Protruded struts were defined as struts being in contact with the vessel wall but with less than one half of the strut thickness impacted into the vessel wall16. Incompletely apposed struts were further divided into malapposed struts and non-apposed side branch (NASB) struts. Malapposed struts were defined as struts with a clear separation between the abluminal surface of the strut and the vessel wall behind in the absence of a side branch, except in the proximal MB, where the Absorb scaffold and Tryton stent were overlapping, in which strut malapposition was defined as a distance greater than 84 microns (thickness of the Tryton stent struts) from the abluminal surface of the Absorb scaffold struts and the vessel wall behind. NASB struts were defined as free floating struts without a vessel wall behind (i.e., at the take-off of a side branch).
3D OCT reconstructions of the final pullbacks were used to assess the ostia of the SB visually. The number of compartments, as created by the jailed SB struts, was counted and related to MLD of the ostial SB on QCA. Furthermore, the different distributions of the jailed SB struts were categorised according to the previously described classification as subtypes V, T, H, and double T17. Furthermore, we added the “double V” subtype to this classification as a potential pattern. Finally, 3D OCT reconstructions were used to classify the coverage of the proximal Tryton stent by the Absorb BVS of the MB. We classified the Tryton stent coverage as follows: complete (coverage of both wedding bands), partial (coverage of only the distal wedding band), and incomplete (no coverage of any of the wedding bands).
Results
A detailed case-per-case description, including illustrative 3D OCT images of the procedures, can be found in the Online data supplement.
BASELINE AND PROCEDURAL CHARACTERISTICS
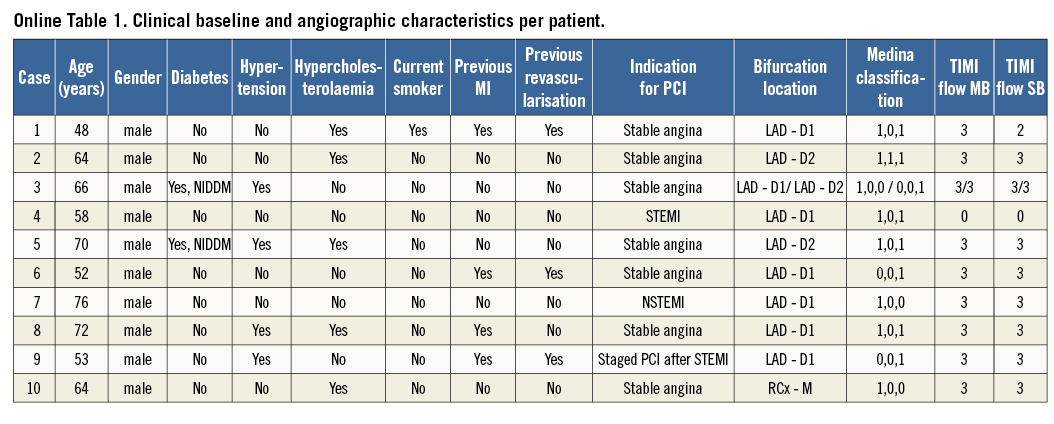
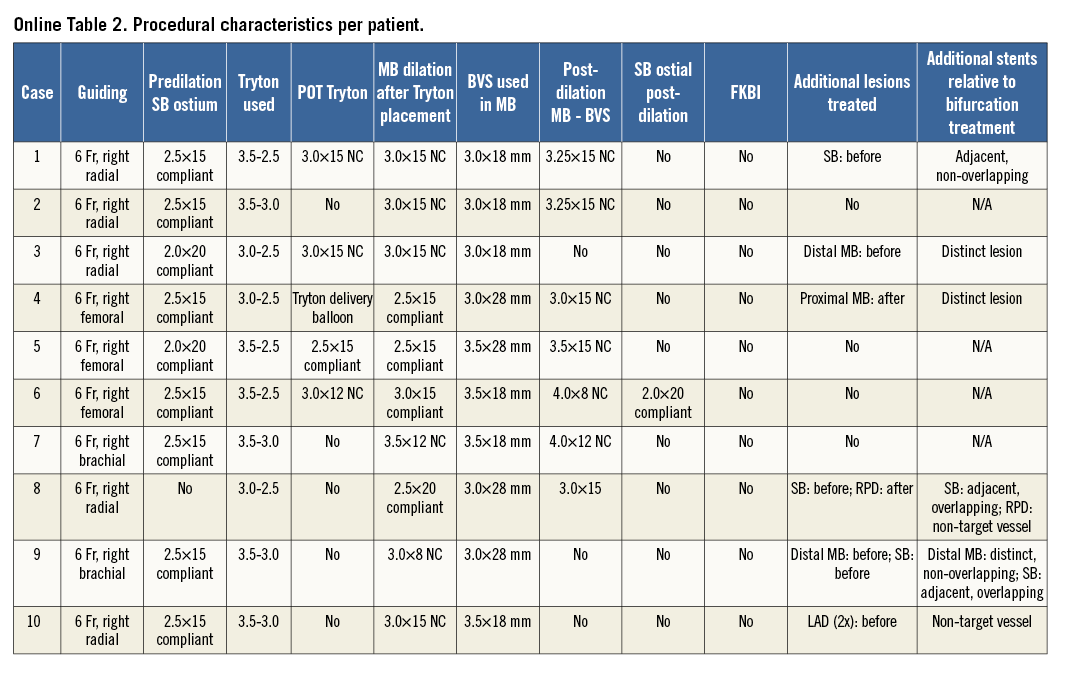
Between January and July 2013, ten patients in our institution were treated with the Tryton stent and Absorb BVS for complex bifurcation disease. Baseline clinical and procedural characteristics are outlined per patient in Online Table 1 and Online Table 2. The mean age was 62 years, and all patients were male. Predilatation of the SB ostium was performed in all except one case. Dilatation of the MB after Tryton stent deployment was performed in all cases. FKBI was not performed in any patient, while in one patient the SB ostium was dilated after MB BVS placement due to severe ostial stenosis of the SB (case 6, Online Figure 6).
In one patient (case 3, Online Figure 3) with two bifurcation lesions, neither Tryton stent nor Absorb scaffold devices could be advanced due to calcifications and sharp angulations in one of the bifurcations. Device success was therefore obtained in 10 of the 11 bifurcation lesions (91%). In two other patients (cases 5 and 6, Online Figure 5 and Online Figure 6), there was >30% residual ostial SB stenosis observed after successful placement of both devices at the intended sites. Angiographic success was therefore 82%. No in-hospital MACE occurred, resulting in a procedural success rate of 82%.
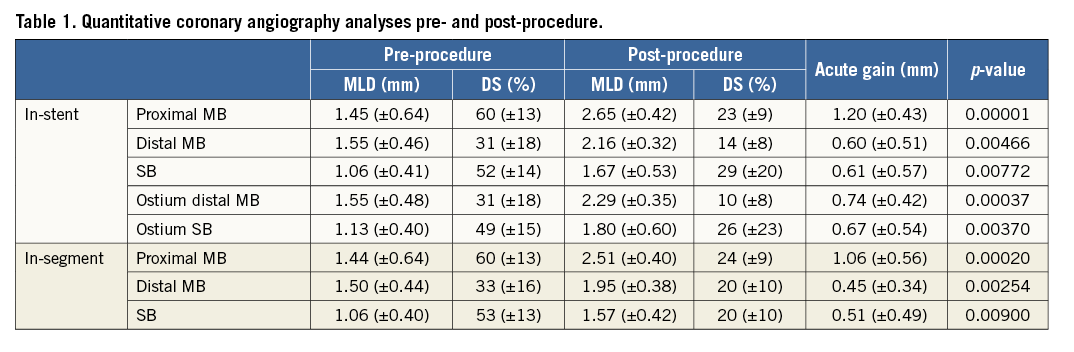
QUANTITATIVE CORONARY ANGIOGRAPHY
QCA results are summarised in Table 1. In-stent acute gains of the proximal MB, distal MB and SB were 1.2 (±0.43) mm, 0.60 (±0.51) mm, and 0.61 (±0.57) mm, respectively. There were no differences in bifurcation angles pre- and post-procedure for the proximal MB to SB angle (154[±20] vs. 159[±17] degrees, p=0.23), for the proximal MB to distal MB angle (152[±16] vs. 150[±12] degrees, p=0.51), and for the distal bifurcation angle (53[±19] vs. 51[±15] degrees, p=0.44).
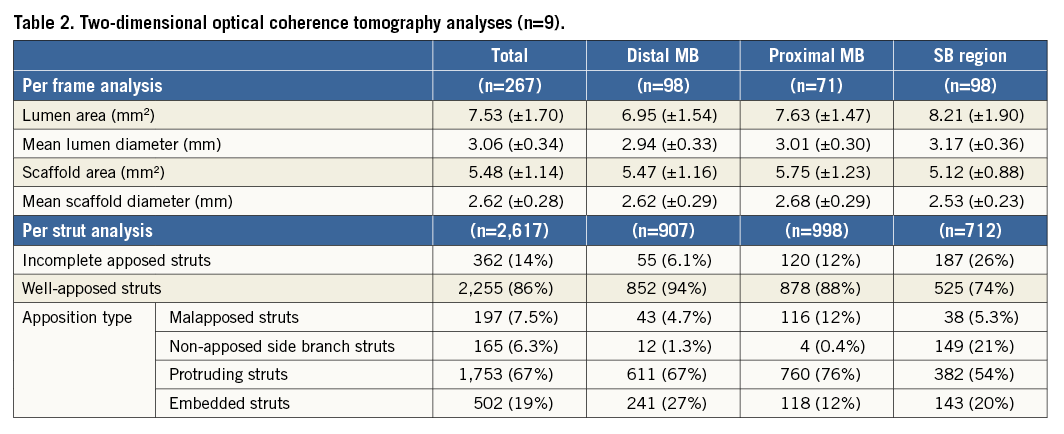
TWO-DIMENSIONAL OPTICAL COHERENCE TOMOGRAPHY MEASUREMENTS
Two-dimensional OCT analysis results are summarised in Table 2. A final OCT pullback could be obtained in all ten patients. However, in one patient 2D OCT analyses were not performed due to insufficient quality of the OCT signal. Overall, 86% of the struts were apposed to the vessel wall, while 14% of the struts were incompletely apposed (7.5% malapposed; 6.3% NASB). As expected, most incompletely apposed struts were located in the bifurcation area (26% of all struts in the bifurcation area), of which the majority were NASB in front of the SB treated with the Tryton stent. In the proximal MB (where the Absorb scaffold overlapped with the Tryton stent), there were more malapposed struts than in the distal MB (12% versus 4.7%), while there were fewer struts embedded in the vessel wall (12% versus 27%).
THREE-DIMENSIONAL OPTICAL COHERENCE TOMOGRAPHY RECONSTRUCTIONS
In three patients, the ostial view could not be assessed due to elongation and repetition cardiac motion artefacts, from an OCT pullback obtained with a pullback speed of 10 mm/s18 (case 5, Figure 1), due to a severely pinched ostium and guidewire shadowing (case 6, Figure 1), or due to insufficient quality of the OCT image (case 7, Figure 1). Proximal Tryton stent coverage could not be assessed in two patients (cases 5 and 7) due to the same above-mentioned reasons.
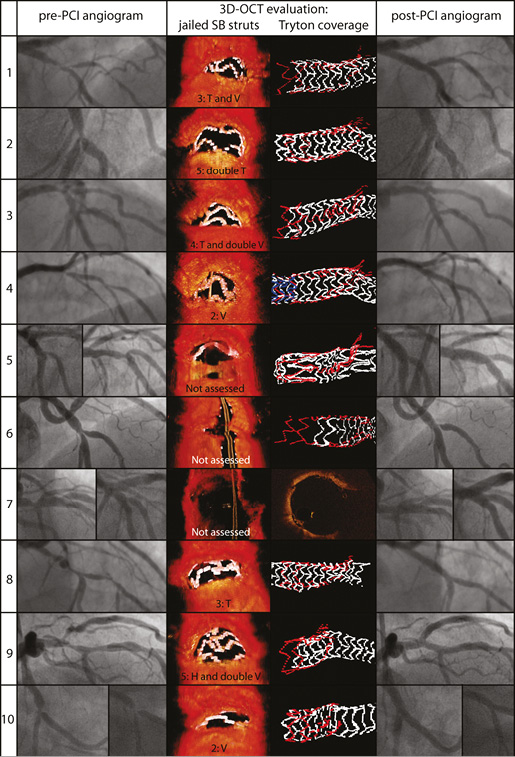
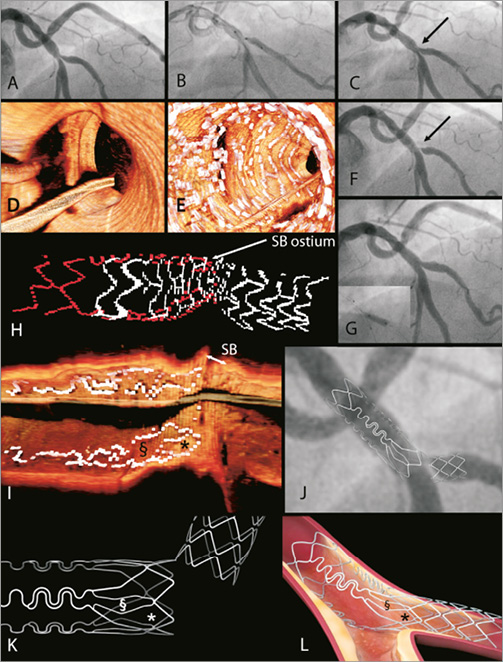
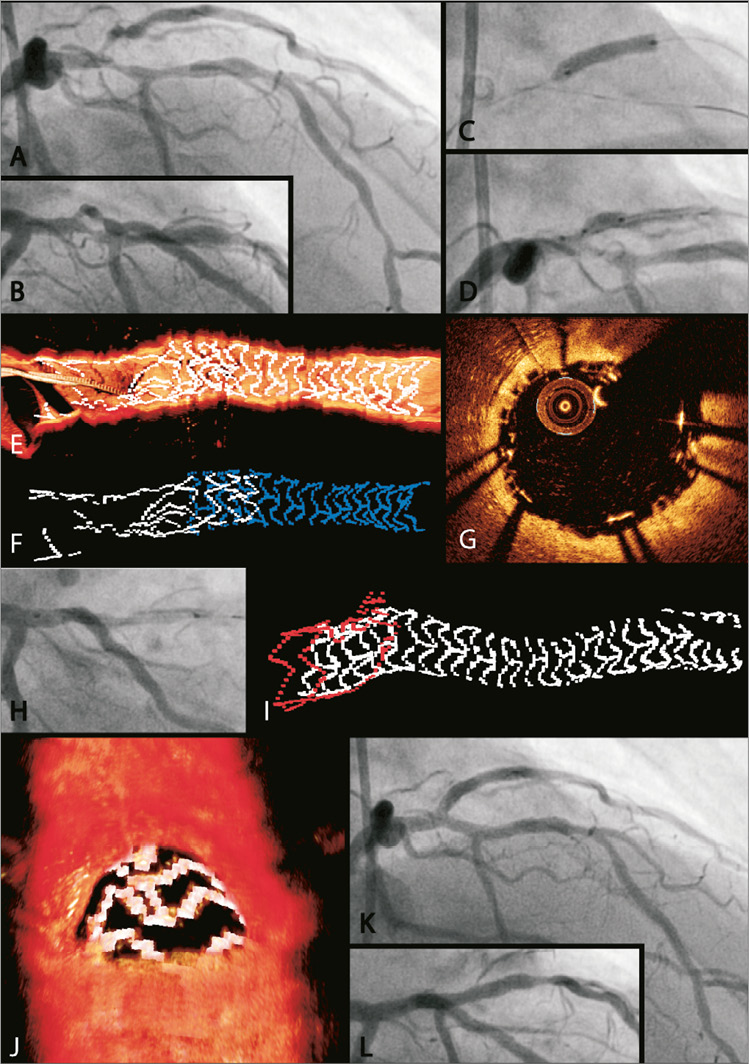
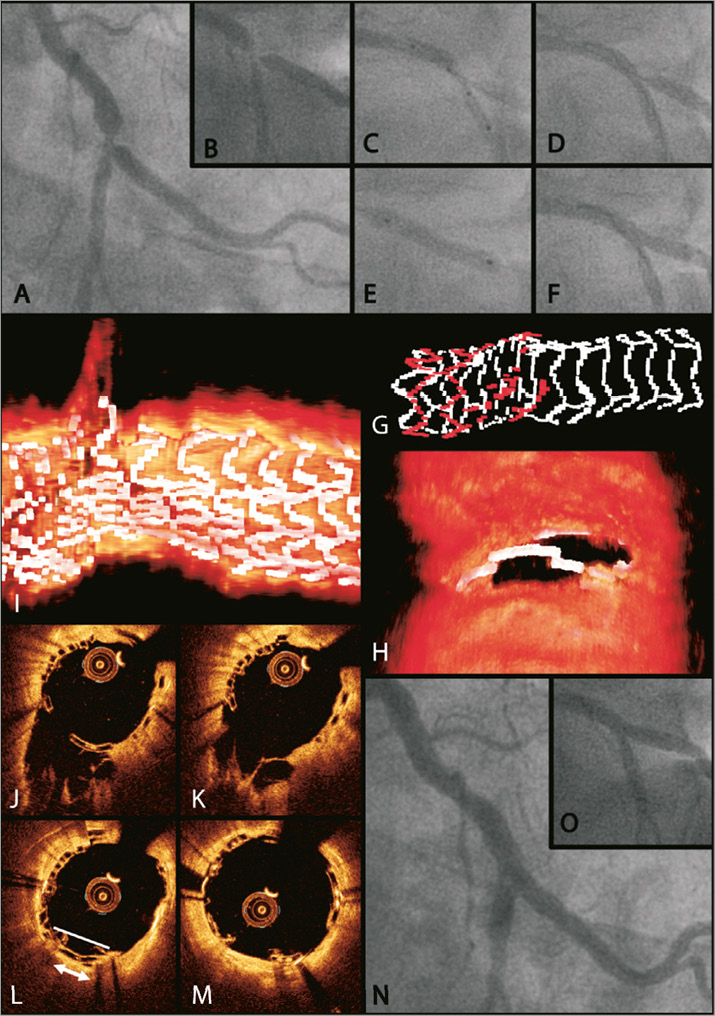
Figure 1. Pre- and post-procedural angiograms and 3D OCT. Pre- and post-procedural angiograms and 3D OCT with side branch jailing by BVS and cut-away views from the stents to assess proximal Tryton coverage of patients 1-10.
Figure 1 shows the ostial views and proximal Tryton stent coverage per patient. There were two patients in whom SB ostia were divided into two compartments, two patients with three compartments, one with four compartments, and two with five compartments. The relation between the number of compartments and the ostial SB MLD, showing that increasing MLD of the SB ostium is associated with a higher number of compartments, is outlined in Figure 2.
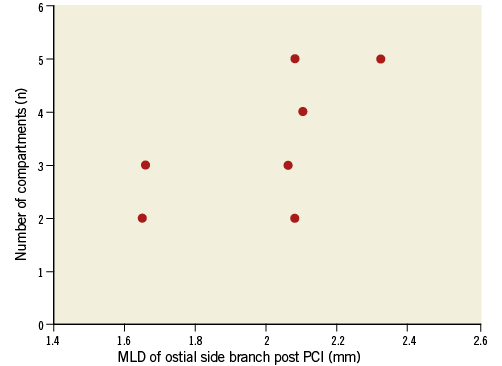
Figure 2. Relation between number of compartments and minimal lumen diameter of the ostial side branch. MLD: minimal luminal diameter, PCI: percutaneous coronary intervention
The following jailed SB strut classifications were observed: V shape (two cases), T shape (one case), double T shape (one case), and more complex combinations in the other three cases: a “T and V” shape, a “T and double V” shape, and an “H and double V” shape (Figure 1).
The proximal Tryton stent was completely covered by the MB BVS in four cases, partially in three cases and incompletely covered in only one case (Figure 1).
CLINICAL FOLLOW-UP
Median follow-up was 187 (IQR 159-262) days. No cardiac deaths, recurrent MIs or STs were observed. Two patients returned for re-PCI of the target lesion. The two patients were the above-mentioned patients who had residual stenoses >30% post procedure. Patient 6 had recurrent chest pains after hospital discharge. Six days after index PCI the SB ostium was successfully treated by implanting a XIENCE Xpedition (2.5×8 mm) (Abbott Vascular) in the SB ostium finishing the procedure with FKBI (Online Figure 6G). The other patient (patient 5) developed recurrent complaints of angina. Diagnostic angiography showed focal in-stent restenosis of the Absorb scaffold in the MB (distally from the SB) and diffuse in-stent restenosis in the Tryton stent. FFR measurements showed that these stenoses were significant (FFR in the distal MB: 0.71, FFR in the SB: 0.75). The patient underwent elective PCI with placement of a Combo (OrbusNeich, Fort Lauderdale, FL, USA) drug-eluting stent in the MB and treatment of the SB with a drug-eluting balloon (SeQuent Please™; B. Braun Melsungen AG, Melsungen, Germany). One other patient (case 7) was treated during an elective re-PCI for a lesion distal from the target lesion, which was initially thought to be non-significant, 30 days after index PCI. Devices placed during index PCI were still patent. As a result, TLR and TLF rates were 20%.
Discussion
To our knowledge, this is the first-in-man combined use of the Absorb BVS and the Tryton Side Branch Stent. We showed that the combined use of these two devices for the treatment of complex bifurcation lesions was feasible in eight out of 11 bifurcation lesions in 10 patients. In one bifurcation, procedural success could not be obtained due to failure to advance any stent (Absorb, XIENCE, Tryton) in the SB due to sharp angulations in combination with considerable calcifications. In two other patients, angiographic success could not be obtained due to residual SB ostium stenosis, both resulting in re-PCI of the target lesions. As a result, TLR and TLF rates were 20%. No cardiac deaths, recurrent MIs or STs were observed.
Angiographic failure of case 6
3D OCT reconstructions were used to evaluate the reason for the angiographic failure in case 6. Although device success was obtained in this patient (i.e., the operators were satisfied with stent positioning and device deployment during the procedure), the angiographic result at the SB ostium was very poor. The 3D OCT reconstructions derived from the final OCT pullback showed an unusual appearance of the Tryton stent in the MB at the level of the SB (Online Figure 6H). While in the other cases it could be clearly visualised that the panels of the transition zone of the Tryton stent were facing towards the SB ostium, with the distal part of the panels being in the SB ostium (Online Figures 1P, 2L, 3L, 4M, 5K, 8M, 9I and 10G), the panel of the sixth case was clearly aligned towards the distal MB (Online Figure 6I). We believe that the Tryton stent was initially positioned too proximally with the transition zone being entirely deployed in the main branch (Online Figure 6B). Because the transition zone is linked to the distal part by only one connector, we think a gap appeared between the transition and distal zones opposite that link (Online Figure 6K and Online Figure 6J), with the stent being bent on the calcified ostial SB plaque opposite the carina (arrows in Online Figure 6C and Online Figure 6F). As a consequence, the distal Tryton stent part was not well aligned at the level of the carina with insufficient ostial scaffolding at the level of the carina. This was corrected by placing an ostial stent during re-PCI. This angiographic failure could have been avoided by preparing the calcified ostial lesion with cutting balloons or even rotablation, and by placing the Tryton stent a little bit more distally. It is recommended to position the stent in such a way that the carina lies one third from the distal middle marker, whereas in case six the distal middle marker was placed exactly at the level of the carina (Online Figure 6B).
Final kissing balloon inflation
In general, the BVS can only be post-dilated to a limited extent with larger sized balloons, because of the previously observed potential risk of acute scaffold disruptions when the scaffold is overstretched19. With FKBI, two balloons are inflated simultaneously in the proximal MB, almost per definition resulting in overexpansion of the BVS. Therefore, we believe FKBI should be avoided in bifurcation treatment using Absorb scaffolds, and so none of the procedures in the current series was finished by FKBI. Although FKBI is considered mandatory in two-stent techniques and recommended by the IFU of the Tryton stent, no differences in one-year TLR rates were observed in a previous study between those patients treated with the Tryton stent in whom FKBI was performed and those in whom FKBI could not be performed20. Currently, a randomised trial is being conducted by the Nordic-Baltic study group comparing FKBI with no FKBI in patients treated with the Tryton stent. This trial will give a more definite answer as to whether FKBI is mandatory in every procedure in which a Tryton stent is used. If it is demonstrated that there is a clear benefit of FKBI in Tryton stent procedures, this will limit the feasibility and applicability of the currently proposed Tryton stent/Absorb scaffold approach. It is worth mentioning that in the current series no overhanging struts shifting out of their expected range, suggesting BVS strut fractures19, were observed.
Previous studies on Absorb scaffold in bifurcation lesions
Previous clinical trials on the BVS predominantly concerned relatively low-risk lesions, excluding patients with bifurcation lesions involving SBs more than 2 mm in diameter21,22. Therefore, clinical follow-up data on bifurcation lesions with large SBs are lacking with only one case report showing the long-term fate of jailed BVS struts on an SB <2 mm23. A previous 3D OCT study on patients included in the ABSORB cohort B trial assessing jailed BVS SB struts showed that 3D OCT is feasible and offers advantages over conventional 2D OCT to evaluate in which way the SB are jailed by the BVS struts. Our findings confirm the observations of this previous study. We also observed that an increase in SB vessel size is related to an increase of the total number of compartments (Figure 2). We could also reproduce the proposed classification of jailed SB strut appearances. However, we also observed some other appearances not classified before: the “double V” for example, but also combinations of the previously described appearances such as “T and V” (Figure 1). Clinical follow-up data of cohort B and the current series in relation to the different jailed SB patterns are needed to gain more insight into the long-term fate of jailed Absorb SB scaffold struts in bifurcations with large SB diameters17,23.
Limitations
The first limitation is the relatively small number of patients included in the current report. Larger studies, randomised data and long-term follow-up (including intravascular imaging) will be needed to evaluate whether this approach is safe and feasible in daily clinical practice. Of special interest will be what happens with BVS struts jailing the SB. Furthermore, because the methods of 3D OCT reconstructions are not yet validated and volume-rendering software does not take into account the curvature of the vessel, 3D OCT findings should be appreciated as being hypothesis-generating.
Conclusions
We present a new treatment strategy in complex bifurcation lesions using the Tryton dedicated bifurcation stent in combination with the Absorb bioresorbable vascular scaffold in 10 patients with 11 bifurcation lesions. The Absorb scaffold and Tryton stent could be delivered at the intended site in all except one bifurcation lesion, due to calcifications and sharp angulations. Angiographic success (<30% residual stenosis) was not achieved in two bifurcations, both eventually resulting in TLRs, leading to a TLR rate of 20%. 3D OCT revealed incorrect Tryton positioning as a reason for one of the angiographic failures, which proves that 3D OCT is a valuable tool for providing insights into the mechanistic aspects of complex PCI procedures. Before this new treatment approach may be considered as a potential opportunity to treat bifurcation lesions with side branches >2 mm with the Absorb BVS, long-term clinical follow-up including intravascular imaging and randomised data will be needed.
| Impact on daily practice Although Tryton stent/Absorb scaffold placement was feasible in 10/11 bifurcations, the relatively high TLR/TLF rate at six months precludes this treatment strategy from being used in daily clinical practice on a large scale. More data, including randomised data with intravascular imaging, are needed to evaluate further the optimal treatment strategy of bifurcation lesions with bioresorbable scaffolds. |
Conflict of interest statement
M.J. Grundeken receives consultancy fees from Tryton Medical. J.J. Wykrzykowska receives consultancy fees from Tryton Medical and Abbott Vascular. J.J. Piek is a member of the Abbott Vascular Medical Advisory Board. The other authors have no conflicts of interest to declare.
Supplementary data
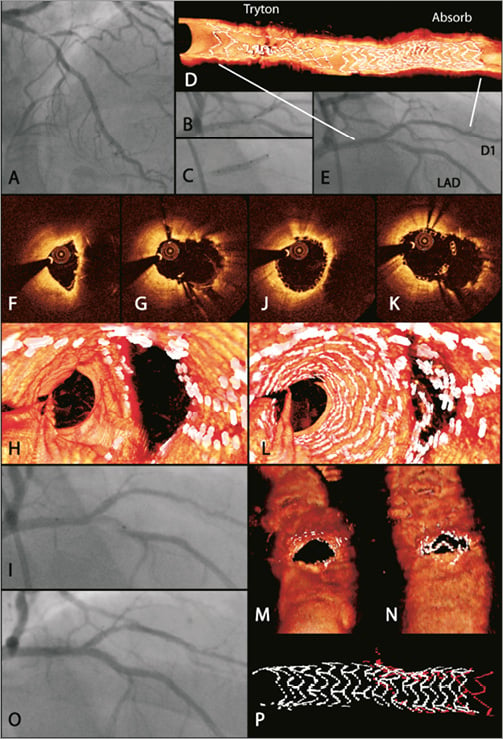
Online Figure 1. Case 1. The first patient was a 48-year-old male with a history of PCI of the right coronary artery (RCA) and ramus circumflex (RCx) branch in 2006. His risk factors for coronary artery disease (CAD) were hypercholesterolaemia, smoking and a positive family history. He presented with progressive complaints of ischaemic chest pains during exercise. The performed exercise test was suggestive of ischaemia in the anterolateral wall. Diagnostic angiography showed a chronic total occlusion of the RCA, patent stents in the RCx, and a bifurcation lesion of the left anterior descending (LAD) artery/first diagonal (D1) branch (A), with involvement of both the proximal MB and the ostial SB (Medina 1,0,1). Furthermore, there was a second subtotal lesion in D1 observed (A). Flow was suboptimal in the D1 (Thrombolysis In Myocardial Infarction [TIMI] 2 flow), while flow was not compromised in the LAD. The patient was planned for PCI of the LAD/D1 bifurcation and D1 lesions. After wiring the LAD, the proximal LAD was predilated with a 2.5×15 mm Trek balloon (Abbott Vascular, Santa Clara, CA, USA). Thereafter, the D1 was wired and the D1 ostium and lesion in D1 were dilated using 1.0×10 mm Sapphire (OrbusNeich, Fort Lauderdale, FL, USA) and 2.5×15 mm Trek balloons. A 2.5×18 mm Absorb BVS was advanced in the SB to treat the lesion in the distal D1 and inflated at 8 atm. Then, a 3.5-2.5×19 mm Tryton stent was positioned using the four radiopaque markers on the delivery system (B) and deployed (C, note the tapering of the delivery balloon) in a non-overlapping but adjacent fashion with the previously placed BVS, as confirmed with offline 3D OCT (D). To ensure accurate apposition of the wedding bands of the proximal part of the Tryton stent, the proximal part of the Tryton stent was post-dilated with a 3.0×15 mm Trek non-compliant (NC) balloon towards the D1. Angiography showed a good result in the proximal LAD and D1 (E). Then the wire in the D1 was retracted and re-crossed into the distal LAD. OCT still frames from an LAD pullback after Tryton placement showed the bifurcation at the level of the carina (F) and side branch ostium (G) before Absorb placement in the MB showing an open side branch ostium with Tryton and some pinching of the proximal MB (F and G). After that, the LAD was dilated at the level of the SB ostium with a 3.0×15 mm NC Trek balloon, followed by placement of a 3.0×18 mm BVS at 10 atm (I). OCT still frames (J and K) at the same level as the OCT still frames (F and G) showed that the MB pinching was resolved while the SB ostium was still widely opened. The procedure was finalised with post-dilatation of the BVS in the LAD using a 3.25×15 mm Trek NC balloon at 8 atm. SB wire re-crossing and final kissing balloon inflation (FKBI) were not performed. Final angiography showed a good result (O), with optimal TIMI 3 flow in both branches. Offline 3D OCT evaluation showed good deployment of the Absorb BVS in the LAD and D1 (D). A fly-through view and a view from outside the vessels (H and M) showed a widely open ostium after Tryton placement. The same views after MB BVS placement (L and N) showed V- and T-type jailed SB strut patterns. Furthermore, 3D OCT showed that the BVS in the LAD did not cover one of the two Tryton wedding bands (P).
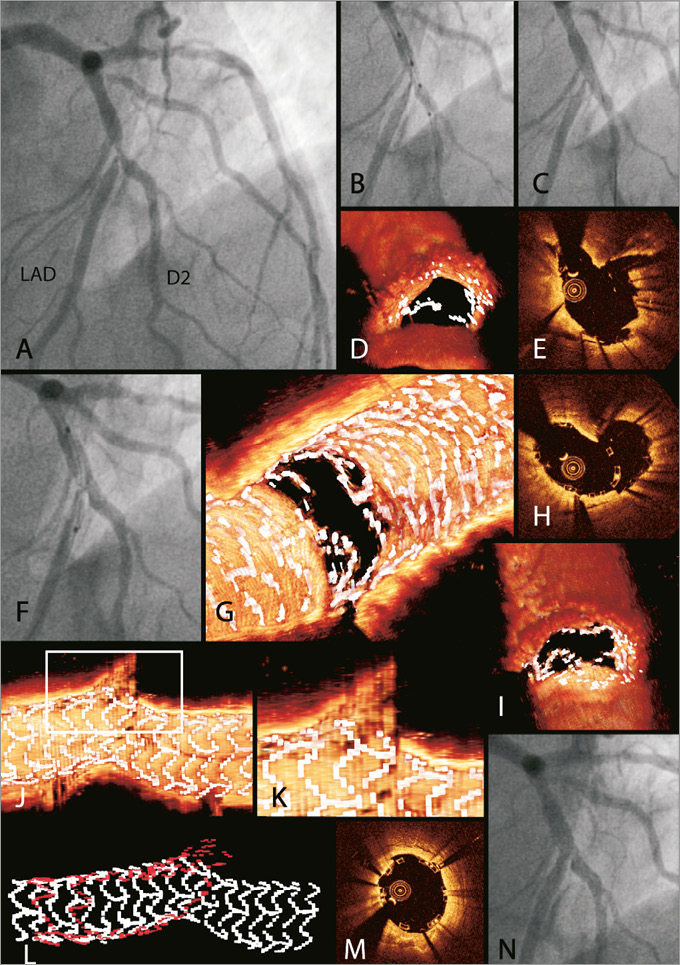
Online Figure 2. Case 2. The second patient was a 64-year-old male known to have dyslipidaemia but without any other past medical history. He presented with complaints of typical ischaemic chest pains. Diagnostic angiography showed vessel wall irregularities of the RCA (maximal stenoses 40%), minor vessel wall irregularities of the RCx and a complex LAD/second diagonal branch (D2) bifurcation lesion, with >95% stenoses of the proximal MB, distal MB and ostial SB (Medina 1,1,1) (A). It was decided to perform a PCI of the LAD/D2 bifurcation lesion. The procedure was started by wiring both branches. After predilation of the SB and MB with 2.0×15 mm and 2.5×15 mm Trek balloons, respectively, a 3.5-3.0×18 mm Tryton stent was positioned from the proximal MB into the SB using the two middle markers (B), with a good angiographic result in the SB after Tryton deployment (C). A 3D OCT reconstruction with a view from outside the vessel to the SB ostium showed an opened ostium of the SB with some of the Tryton struts in front of the SB ostium (D), as is also shown in the OCT still frame at the level of the SB ostium (E). After deployment of the Tryton stent, the SB wire was re-crossed into the distal MB and the MB was predilated with a 3.0×15 mm Trek NC balloon at 12 atm. Then a 3.0×18 mm BVS was placed (F) in the MB (inflation at 10 atm), and the procedure was finalised with post-dilation of the BVS with a 3.25×15 mm Trek NC balloon at 8 atm without additional SB rewiring or FKBI. After post-dilation of the Absorb there were just a limited number of struts visible in front of the ostium, as shown by a 3D OCT reconstruction viewing from the lumen towards the SB (G) or viewing from outside the vessel towards the SB ostium (I). An OCT still frame (H) and a 3D OCT reconstruction with a cut-away view at the level of the SB ostium (J, with the white rectangle indicating the area enlarged in K) showed that the Absorb is “flaring” into the SB ostium, enlarging the BVS cell size towards the SB ostium. 3D OCT reconstructions of the separate stents showed that the Tryton (in red) is completely covered by the Absorb (in white), as recommended in the instructions for use (L). An OCT still frame at the level of the proximal Tryton/Absorb overlap showed good apposition of both the Tryton and Absorb struts (M). Final angiography showed a good result (N).
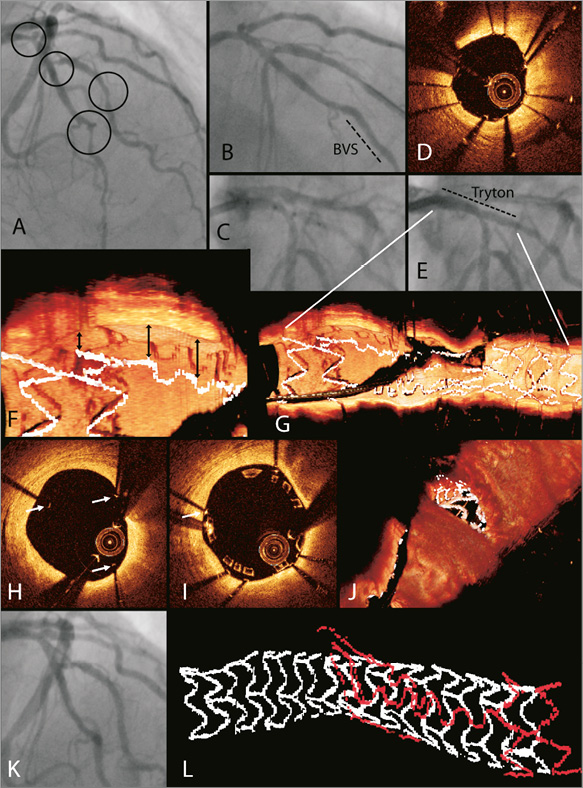
Online Figure 3. Case 3. The third patient was a 66-year-old male who presented with atypical retrosternal chest pains. The patient had diabetes mellitus (medically treated, non-insulin-requiring), hypertension and a positive family history of cardiovascular disease. Myocardial perfusion scintigraphy with adenosine revealed reversible perfusion defects in the anteroseptal region. Diagnostic angiography showed a distal 80% LAD lesion with ostial stenoses of the D1 and D2 and a fourth lesion in the D2 (encircled in A). It was decided to treat the patient with two Tryton stents, one in the D1 (Medina 1,1,1 bifurcation lesion) and another one in the D2 (Medina 0,0,1) in combination with Absorb scaffolds in the LAD and an additional BVS in the D2. First, the LAD was wired and the distal LAD lesion was predilated with a 2.5×15 mm Trek balloon at 10 atm. After predilation, a 2.5×18 mm Absorb was deployed at 10 atm (B). Thereafter, the D2 was wired and both the D2 ostium and the lesion in the D2 were predilated with a 2.5×15 mm Trek NC balloon at 10 atm. An attempt to advance a BVS into the D2 was made. However, the BVS could not be advanced due to calcification and sharp angulations. The BVS was retracted from the patient without difficulties and discarded. It was decided to treat the lesion with a XIENCE Xpedition (Abbott Vascular) DES instead; however, this stent could also not be advanced. Since the angiographic result of the D2 ostial and distal lesions was acceptable, the operator decided not to attempt further stent placement in the D2. The procedure was continued by wiring the D1 and predilating the ostium with a 2.0×20 mm Trek balloon. Subsequently, a 3.0-2.5×19 mm Tryton stent was advanced and positioned using the four radiopaque markers (C) and deployed at 10 atm. The proximal Tryton was post-dilated towards the SB ostium with a 3.0×15 mm NC balloon. An OCT pullback from D1 to proximal LAD showed good apposition of the Tryton stent in the SB (D). The angiographic result of the SB ostium after Tryton deployment was excellent (E), although a cut-away view from a 3D OCT reconstruction showed considerable malapposition of one of the two Tryton wedding bands and one of the three fronds (G, detail enlarged in F). An OCT still frame at the level of the fronds (white arrows) also showed the malapposed fronds (H). The guidewire in D1 was re-crossed into the distal LAD, fenestrating the Tryton stent, and the MB was predilated with a 3.0×15 mm NC balloon at 10 atm. A (new) 3.0×18 mm BVS was advanced and placed in the MB at the LAD/D1 bifurcation (at 10 atm) after which the BVS was post-dilated with a 3.5×15 mm balloon at 10 atm. The final angiogram showed a good result of the distal LAD and LAD/D1 lesions with satisfactory results in the D2 and LAD/D2 lesions (K). An OCT still frame from the final pullback showed well-apposed wedding bands and three fronds of the Tryton in the proximal MB, although the apposition of Absorb was not complete (I). Offline 3D OCT reconstructions of the final pullback showed T and double V shaped BVS struts in front of the SB ostium (J). The final angiogram showed a good result in the LAD/D1 bifurcation and an acceptable result in the LAD/D2 bifurcation (K). A 3D OCT reconstruction of the two separate stents showed that the Absorb (white) did not completely cover the proximal Tryton stent, leaving one wedding band uncovered (L).
Online Figure 4. Case 4. The fourth patient was a 58-year-old male with a history of stable angina, which was medically treated until current presentation with ST-segment elevation myocardial infarction (STEMI) with elevations in V1, V2 and aVL. He was transferred to the catheterisation laboratory for a primary PCI. Angiography showed some vessel wall irregularities in the RCA, a small but normal RCx, and a proximal LAD occlusion (A). The LAD was wired and thrombus aspiration was performed. After thrombus aspiration, two lesions were seen, one subtotal proximal LAD lesion and a Medina 1,1,1 LAD/D1 bifurcation lesion (see circles, B). First, the proximal LAD and both the MB and the SB of the bifurcation lesion were predilated with a 2.5×15 mm Sapphire balloon (8 atm). Then, a 3.0-2.5×19 mm Tryton stent was positioned (C) and deployed from the proximal MB into the SB at 10 atm, after which angiography showed good results at the SB ostium (D). Next, the proximal part of the Tryton stent was post-dilated using the delivery balloon. Thereafter, the SB wire was re-crossed through the Tryton into the distal LAD and the MB was dilated with a 2.5×15 mm Sapphire balloon at 14 atm. A 3.0×28 mm BVS was advanced and deployed at 11 atm in the MB (E). Angiography revealed residual stenosis (black arrow) of the proximal subtotal LAD lesion after predilations (F). Subsequently, a second BVS (3.5×18 mm at 8 atm) was placed in the proximal LAD, overlapping the first BVS, to treat the proximal LAD lesion. The Absorb scaffolds in the LAD were post-dilated using a 3.0×15 mm Trek NC balloon at 12 atm. The final angiogram showed a good result in the proximal LAD and LAD/D1 bifurcation lesion (I). A 3D OCT reconstruction with fly-through view from the lumen (G) and from outside the vessel (H) at the SB ostium showed an open ostium with a V-shaped jailed SB strut. A cut-away view at the level of the SB ostium of a 3D OCT reconstruction (K) showed “flaring” of the Absorb struts into the SB. An OCT still frame at the level of the carina showed an open SB ostium with only some jailed SB struts (L). 3D OCT reconstructions of the three separate stents/scaffolds showed well the alignment of the three stents/scaffolds where they overlapped (M). An enlargement of the overlapping stents/scaffolds showed that the proximally placed second Absorb (in blue) considerably overlapped the distally placed Absorb (in white), and that they both covered the Tryton stent (in red) wedding bands (P). An enlargement of the proximally placed Absorb (J) showed some signs of unequal strut distribution (white arrows), compared to the distally placed Absorb (N), although OCT revealed well-apposed struts at the level of the three stents/scaffolds overlapping (O), as well as at the level of the distal and proximal Absorbs.
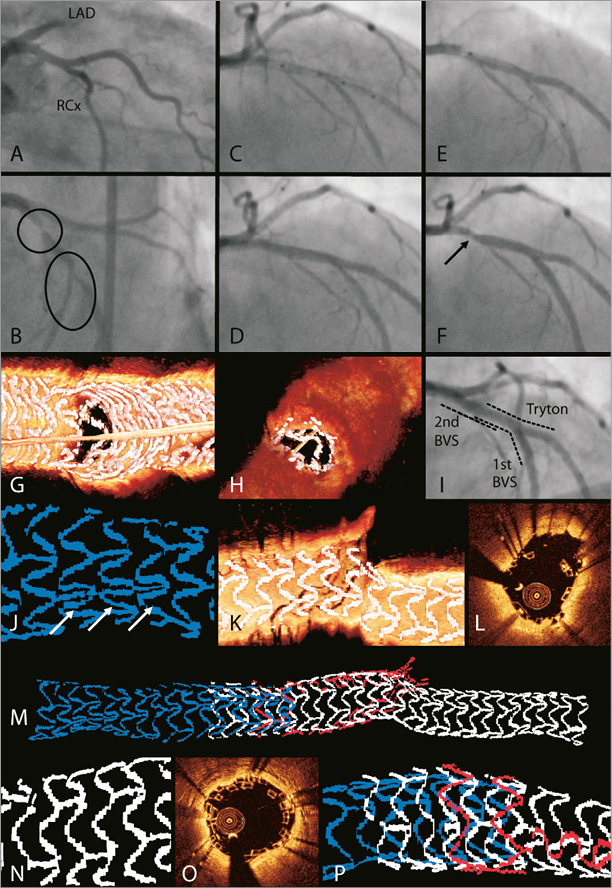
Online Figure 5. Case 5. The fifth case was a 70-year-old male patient with hypertension, diabetes (medically treated, non-insulin-dependent), and hypercholesterolaemia. He presented with typical complaints of stable angina. A diagnostic angiogram (A and B) showed a significant LAD/D2 bifurcation lesion with involvement of both MB and SB (Medina 1,1,1) and the patient was planned to undergo a PCI of the bifurcation lesion with the Tryton/Absorb treatment strategy. First, the LAD and the D2 were wired and both branches were predilated with a 2.0×20 mm Trek balloon (10 atm). Subsequently, a 3.5-2.5×19 mm Tryton was positioned (C) and deployed (D) from the proximal MB into the ostial SB at 8 atm, after which angiography showed a good result of the D2 ostium (E). The proximal part of the Tryton stent was post-dilated towards the SB ostium using a 2.5×15 mm Trek balloon (12 atm). After SB wire re-crossing into the distal MB through Tryton, the LAD was predilated with a 2.5×15 mm Trek balloon at 14 atm. Thereafter, a 3.5×28 mm BVS was positioned (F) and deployed at 15 atm in the main branch. Angiography after BVS deployment showed some residual stenosis in the MB opposite the SB ostium (G). Multiple post-dilations of the BVS were performed using 3.0×15 mm and 3.5×15 mm Trek NC balloons (H). Final angiography showed a good result with only minor residual stenosis less than 20% opposite the side branch ostium (black arrow in I and J). The 3D OCT reconstruction of the stents could not be used due to cardiac motion artefacts: both elongation (white arrows), shortening (yellow arrows), as well as repetition (red arrow) artefacts were observed (K). OCT still frames showed perfect alignment of the Absorb and Tryton in the proximal MB with good apposition to the vessel wall (L). An OCT still frame at the carina level (M) showed a calcified plaque responsible for the residual stenosis seen on the angiograms of panels E-I.
Online Figure 6. Case 6. The sixth case was a 52-year-old male patient with a positive family history of cardiovascular disease and a history of a transient ischaemic attack and a STEMI, treated with a primary PCI of the RCA nine months before. He presented with recurrent complaints of chest pains. A diagnostic angiogram (A) showed an LAD/D1 bifurcation lesion with a significant 80% ostial lesion of the D1 and an intermediate stenosis of the LAD (Medina 1,1,1). The short LAD lesion was assessed with an FFR measurement, which was 0.85, and lumen measurements on OCT, which showed a minimum lumen area in the LAD of 3.4 mm2. It was decided to perform a PCI using the Tryton/Absorb treatment strategy. First, both branches were wired and the ostium of the D1 predilated with a 2.5×15 mm Trek balloon. Then, a 3.5-2.5×19 mm Tryton was placed in the proximal MB-ostial SB at 10 atm (B). Exact Tryton positioning was difficult because of excessive motion of the coronaries during heartbeats. The proximal part of the Tryton stent was post-dilated towards the SB ostium using a 3.0×12 mm Trek non-compliant balloon (12 atm). Angiography showed a suboptimal result at the SB ostium due to a severely calcified plaque at the SB ostium opposite the carina (C, black arrow). After SB wire re-crossing into the distal MB through Tryton, a 3.5×18 mm Absorb was deployed at 8 atm in the LAD. After BVS deployment, the angiographic result was poor (F). “Fly-through” views derived from three-dimensional (3D) optical coherence tomography (OCT) reconstructions looking from proximal to the carina in the same angle before (D) and after (E) the procedure showed considerable shifting of the carina as the explanation for the pinched ostium. To improve the result of the SB ostium, a wire was fenestrated through the Absorb into the SB, and the D1 ostium was dilated with a 2.0×20 mm balloon at 10 atm. Although the angiographic result in the D1 was slightly improved, OCT still frames from an OCT pullback revealed distorted geometry of the Absorb with jailed SB struts “sagging” towards the LAD lumen (not shown). Therefore, in order not to jeopardise the LAD by the risk of ST of these struts, and to ensure optimal scaffolding of the LAD, it was decided to post-dilate the BVS with a 4.0×8 mm non-compliant Trek balloon at 6 atm. Although the final angiographic result of the LAD was excellent, the angiographic result of the SB ostium remained very poor. Because flow in the SB was optimal, it was decided to stop the procedure and to observe the patient to see whether he would develop recurrent angina. One week after the initial procedure, the patient underwent a re-PCI of the ostial SB. A short DES was placed at the ostium of the SB (G, see inset) with a satisfactory final angiographic result after final kissing post-dilatation (G). The 3D OCT reconstructions of the initial procedure revealed the reason for the carinal shifting causing pinching of the SB ostium. A cut-away view from a 3D OCT reconstruction of the separate devices showed an unusual appearance of the Tryton stent in the MB at the level of the SB (H). Panel I shows a cut-away view looking from the same direction as in H, with the Absorb BVS being “filtered out”. Two cells from one of the three panels could be clearly visualised (* and §). The panel is aligned along the MB vessel wall, opposite the carina, whereas in the other patients the panels of the transition zone were positioned towards the SB ostium (Online Figures 1P, 2L, 3L, 4M, 5K, 8M, 9I, and 10G). Panel K illustrates what we believe happened: the struts between the transition zone and the distal zone were separated because the Tryton stent was bent over the calcified lesion at the level of the single connector between the distal and transition zones. By doing this, the panels of the transition zone (with cells * and § in panel K corresponding with the cells in panel I) were apposed to the MB wall instead of the carina in the SB ostium. Panel J shows an enlargement of the final angiography with an illustration of Tryton to illustrate how we believe the stent was positioned after MB stent deployment. Because the panels of the transition zone were not covering the SB ostium, the carina was not scaffolded properly and carinal shifting could occur. Panel L illustrates how Tryton should be positioned with the distal one third of the panels being positioned in the ostium, scaffolding the SB (cells indicated by * and § correspond with the cells in panels I and K).
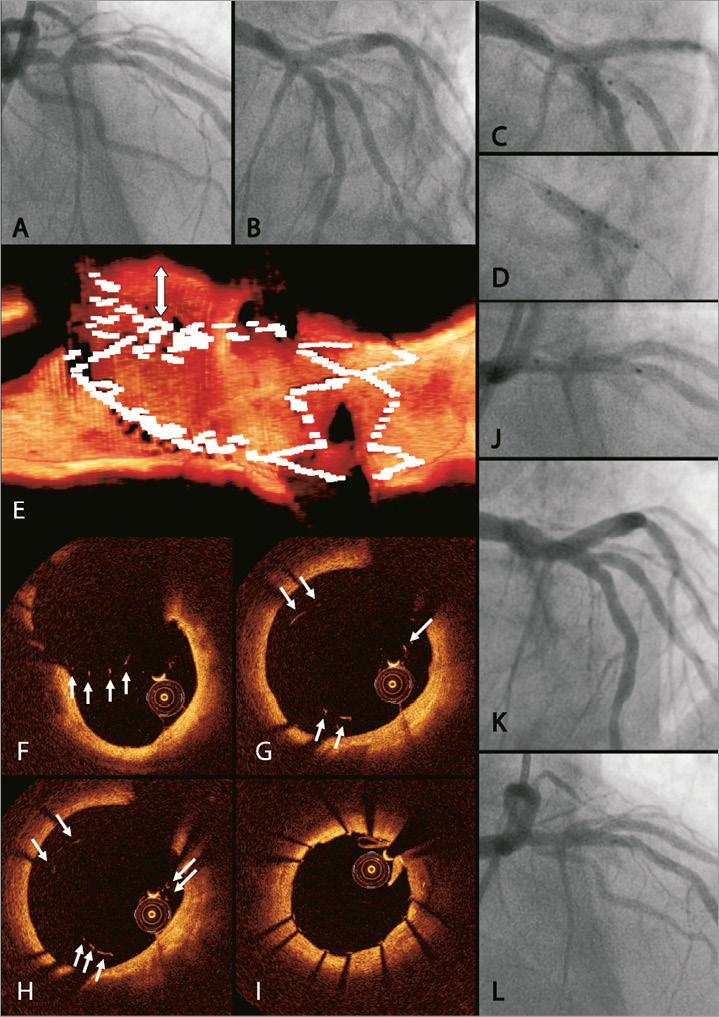
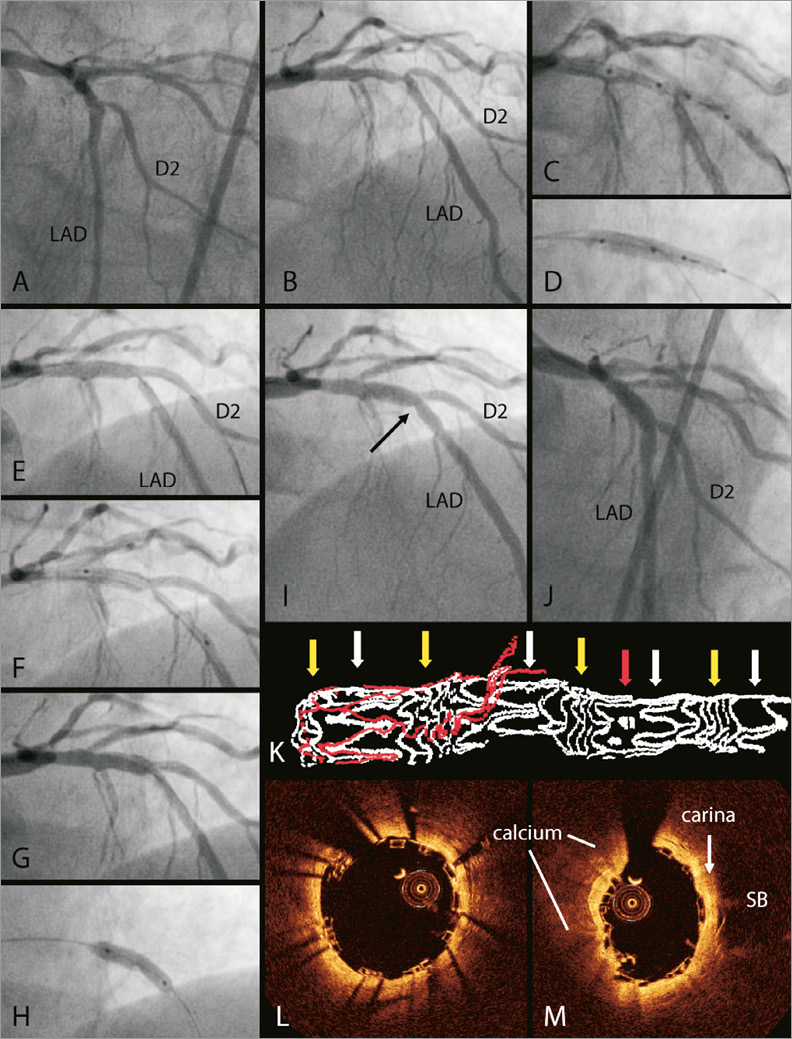
Online Figure 7. Case 7. The seventh patient was a 76-year-old male, without any past medical history, currently presenting with NSTEMI with positive troponins and negative T-waves on the ECG in leads V2-V6. Diagnostic angiography showed an intermediate stenosis in the proximal RCA, an RCx without stenoses, and a subtotal stenosis of the proximal LAD with a 70% stenosis of the D1 ostium (Medina 1,0,1) (A and B). It was decided to perform a PCI of the LAD/D1 bifurcation lesion and to perform an FFR measurement of the RCA lesion. First, both the LAD and D1 were wired. After predilation of the SB ostium and proximal LAD with a 2.5×15 mm Trek balloon, a 3.5-3.0×18 mm Tryton stent was positioned from the proximal MB into the SB (C). After positioning and deployment of the Tryton stent (D), the SB wire was re-crossed into the distal MB and the MB was predilated with a 3.5×12 mm Trek NC balloon at 8 atm. Thereafter, a 3.5×18 mm BVS was deployed in the MB at 11 atm (positioning of the BVS shown in J). The BVS was post-dilated proximally with a 4.0×12 mm Trek NC balloon at 12 atm. The SB was not re-crossed and FKBI was not performed. Final angiography showed a good result with TIMI 3 flow in both branches (K and L). FFR of the RCA lesion was 0.83. OCT pullbacks were performed after Tryton placement and a final pullback was obtained post procedure. However, the final OCT pullback was of insufficient quality and not suitable for 3D OCT reconstructions. Three-dimensional OCT reconstructions of the pullback after Tryton placement showed malapposition of the fronds in the proximal MB (white arrow, E). Panels F-I show OCT still frames from the SB ostium to the proximal MB, demonstrating malapposition of a panel facing towards the SB ostium (white arrows in F), and of the fronds in the proximal MB (white arrows in G and H), while the wedding bands are well-apposed (I). A residual stenosis in the distal LAD was initially left untreated. However, due to persistent angina, the patient returned for a re-PCI after one month, which was performed successfully.
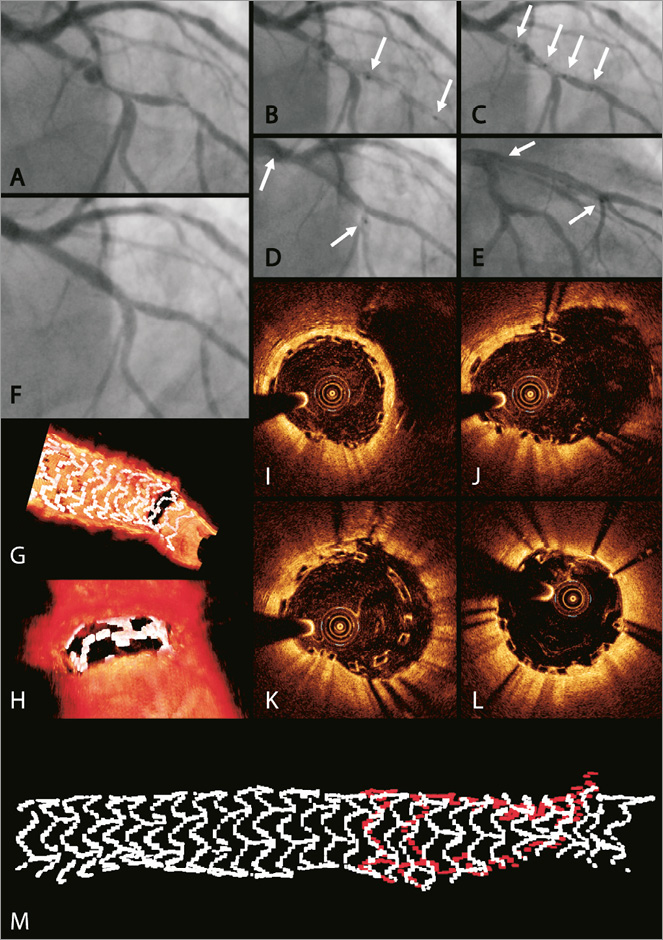
Online Figure 8. Case 8. Patient number eight was a 72-year-old male patient known with stable angina for two years, which was successfully medically treated. However, he developed progressive angina with ST-segment depressions in II, V4-V6 and ST-segment elevation in a VR during exercise testing. He had a medical history of acute MI 15 years before for which he did not undergo a percutaneous intervention. Diagnostic angiography showed a dominant RCA with an 80% stenosis in the right posterior descending artery, a small RCx/IM with vessel wall irregularities, and a LAD/D1 bifurcation lesion with a stenosis (90%) in the proximal LAD and lesions of the SB at the ostium and more distally (Medina 1,0,1) (A). The patient was planned to undergo an elective PCI of the LAD/D1 and RCA lesions. First, the LAD and D1 were wired and the distal D1 lesion was predilated with a 2.5×20 mm Sprinter Legend RX balloon (Medtronic, Minneapolis, MN, USA). Then, a 2.5×18 mm Absorb BVS was positioned (B, white arrows indicating proximal and distal markers on the delivery balloon) and deployed in the D1 at 14 atm and post-dilated with a 2.5×20 mm Sprinter Legend RX balloon at 16 atm. Thereafter, a 3.0-2.5×19 mm Tryton was positioned (C, white arrows indicating the four radiopaque markers on the delivery system) from the proximal LAD into the D1 and deployed at 14 atm. Subsequently, the MB was dilated with a 2.5×20 mm Sprinter Legend RX balloon after which a 3.0×28 mm BVS was deployed at 14 atm in the main branch (D and E for BVS positioning; white arrows indicating distal and proximal markers of the delivery balloon). The BVS in the MB was post-dilated using a 3.0×15 mm Trek NC balloon at 18 atm. The SB was not re-crossed and FKBI was not performed. Panel F shows the final angiographic result. The lesion in the right descending posterior artery was treated with a 2.5×15 mm XIENCE Xpedition (Abbott Vascular). Three-dimensional OCT reconstructions looking at the SB showed an open carina with jailed BVS struts in a “T and V” appearance (G and H). Panel G also shows how the distal end of the Absorb is placed just distally to the SB ostium. OCT still frames from the same pullback show the jailed BVS struts jailing the SB (J and K), with the BVS being well-apposed just distal from the bifurcation at the level of the carina (I) and in the proximal MB at the overlap with the proximal Tryton stent (L). Three-dimensional OCT reconstructions from the separate devices show complete coverage of the Tryton stent (M).
Online Figure 9. Case 9. The ninth patient was a 53-year-old male patient with a recent STEMI for which he underwent a primary PCI with a XIENCE Xpedition stent placement in the RCx. Besides the culprit lesion in the RCx, angiography revealed a distal LAD lesion and a Medina 1,1,1 lesion of the LAD/D1 bifurcation (A and B). After primary PCI, it was decided by the local Heart Team to treat the LAD/D1 lesion in an elective setting. LAD/D1 treatment: after wiring of LAD and D1, the distal LAD lesion was dilated with a 2.5×15 mm Sprinter Legend RX balloon and treated with a 2.5×18 mm BVS (10 atm). Thereafter, the D1 was predilated using a 2.5×15 mm Sprinter Legend RX balloon (8 atm). Then, an Absorb BVS was placed in the D1 (C). A 3.5-3.0×15 mm Tryton was positioned from the proximal LAD into the D1 using the four radiopaque markers on the delivery system (D, most proximal marker not visible) and deployed at 10 atm, overlapping with the previously placed BVS. Three-dimensional OCT reconstructions show precisely how the Absorb and Tryton were positioned relative to each other, showing a considerable overlap (E and F), with perfect alignment visible on 2D OCT (G). Thereafter, the wire in the D1 was re-crossed in the distal LAD. Subsequently, the MB was dilated with a 3.0×8 mm Trek NC balloon (10 atm) after which a 3.0×28 mm BVS was deployed at 9 atm in the main branch (positioning shown in H). The BVS in the MB was not post-dilated. Furthermore, the D1 was not re-crossed and the D1 ostium not dilated. No FKBI was performed. Panel I shows the 3D OCT reconstruction of the final OCT pullback in the MB. Only one of the Tryton wedding bands was overlapped by the BVS. Panel J shows a 3D OCT reconstruction with an ostial view showing that the SB ostium was divided into five compartments. The final angiogram shows a perfect result (K and L).
Online Figure 10. Case 10. The tenth patient was a 64-year-old male patient with typical anginal chest pains during exercise. His risk factors for coronary artery disease included hypercholesterolaemia and a positive family history of cardiovascular disease. Exercise test showed ST-segment depressions in leads V5 and V6. Diagnostic angiography showed vessel wall irregularities in the RCA, a non-diseased left main, two 80% stenoses in the LAD, and an RCx/marginal branch bifurcation lesion with both MB and SB involvement (Medina 1,1,1) (A and B). It was decided by the local Heart Team to perform a PCI of both lesions in the LAD and of the RCx/marginal branch bifurcation. First, the LAD was wired and, after predilatations using a 2.5×15 mm Sprinter Legend RX balloon, two Combo (OrbusNeich) DES were used to treat the lesions in the LAD. Thereafter, the RCx and marginal branch were wired and predilated with a 2.5×15 mm Sprinter Legend RX balloon in both branches. Then, a 3.5-3.0×18 mm Tryton was placed from the proximal RCx towards the distal RCx at 7 atm (C). Subsequently, the wire in the distal RCx was retracted and fenestrated through the Tryton stent towards the marginal branch. Angiographically, the result of the distal RCx ostium was improved considerably (D). The MB was predilated with a 3.0×15 mm Sprinter NC balloon at 8 atm and a 3.5×18 mm BVS was deployed in the MB at 9 atm (E). The BVS was not post-dilated. Furthermore, no SB post-dilations or FKBI were performed. Final angiography showed a good result (F, N, and O). Offline 3D OCT reconstructions showed complete coverage of the two Tryton wedding bands (G). Furthermore, a cut-away view looking at the SB ostium showed one BVS strut “flaring” towards the SB (I). This was also observed on consecutive OCT still frames (J-M), showing a straightened BVS strut (white arrow) in an unexpected place when compared with the previous two frames (J and K), as indicated by the solid white line in L. Panel M shows perfect apposition of the BVS-Tryton layers in the proximal MB. Panel H shows an ostial view from outside the vessel showing a V-shaped appearance of the jailed BVS strut.