Abstract
Bifurcations are increasingly being treated with bioresorbable vascular scaffolds (BVS) and accounted for about 25% of patients treated in the large multicentre GHOST-EU registry. This registry, along with bench testing, has provided a glimpse of the techniques and limitations of treating bifurcations with BVS. The provisional strategy remains the default approach to bifurcation treatment with BVS. If correctly performed, SB dilatation, T-kissing inflation, crossover to side branch stenting and elective double stenting are feasible without causing scaffold disruption. Theoretically, when the scaffolds are resorbed, the normal bifurcation anatomy, flow and vascular function will be restored, while jailed SBs will be liberated. However, data from the GHOST-EU registry are awaited to confirm the long-term safety and efficacy of BVS in coronary bifurcations.
Introduction
The treatment of coronary bifurcations that have side branches >2 mm with bioresorbable vascular scaffolds (BVS) has been considered off-label and excluded from the pivotal BVS studies. However, bifurcations may still be associated with higher event rates than non-bifurcation lesions, and concerns remain about implanting two stents in the bifurcation and about the risks of excess metal at the carina. Thus, it has been postulated that BVS may have potential advantages in bifurcations that are greater than those which have been demonstrated for simple lesions. The absence of a permanent metallic cage as the scaffold reabsorbs and the restoration of normal bifurcation anatomy, flow and vascular function may result in the unjailing of side branches (SB), less shear stress and a decreased risk of late complications, in particular scaffold thrombosis1,2. Potential limitations in treating bifurcations with BVS are the larger profile, decreased deliverability, increased strut thickness which limits the performance of certain bifurcation techniques, and limited tolerance to post-dilatation (0.5 mm) that impacts on the performance of bifurcation optimisation techniques such as dilatation towards the SB and final kissing balloon inflation (FKBI) because of the possible breakage of connectors. Lesion preparation, scaffold sizing, scaffold implantation and optimisation are essential to ensure optimal outcomes with BVS3. In this review, we summarise the largest real-world experience and lessons learnt as regards what should and should not be done with respect to treating bifurcation lesions with BVS.
Bifurcations in the GHOST-EU registry
Despite an initial hesitancy, experienced centres have explored and evaluated the techniques for treating bifurcations with these new devices. The large multicentre GHOST-EU (Gauging coronary Healing with biOresorbable Scaffolding plaTforms in EUrope) registry offers a glimpse of the real-world experience with BVS4. The first publication of the GHOST-EU registry included 1,731 Absorb BVS (Abbott Vascular, Santa Clara, CA, USA) implanted in 1,189 patients. In 27% of patients, an Absorb BVS was implanted at a bifurcation lesion. Almost half of the bifurcation lesions treated were true bifurcations and the left anterior descending diagonal artery bifurcation was the most common bifurcation treated. Over 80% of bifurcations were treated with a provisional approach of only the main branch (MB) with crossover to stenting of the SB in about 5% of cases. FKBI was performed in 18% and sequential SB-MB dilatation in 5% of bifurcations. The left main represented only 1.2% of lesions treated, mostly due to the unavailability of scaffolds 4.0 mm or larger. The technical aspects discussed below also apply to left main bifurcations with the exception that serial inflation of the BVS may be required in patients who cannot tolerate the long balloon inflation required for BVS implantation. However, due to limited experience of treating the left main bifurcation we have not made any specific recommendations in this regard in the current review.
Technical aspects of BVS implantation in bifurcations
The GHOST-EU registry has provided important insights into the techniques of bifurcation PCI with BVS. The suggestions below are based on the operators’ personal experience in combination with data obtained from benchtop testing. The main technical aspects of treating bifurcations with BVS are summarised in Table 1 and are discussed below.
PROVISIONAL APPROACH REMAINS THE DEFAULT STRATEGY EVEN WITH BVS
As seen in the GHOST-EU registry, the provisional approach remains the default strategy for treating bifurcations and can be performed as previously described for metallic stents5. As a result of the limited post-dilatation capability of BVS, stent size selection for the MB has been an issue of debate. In general, we still select the BVS size based on the distal MB unless there is significant tapering of the vessel and the difference between the proximal and distal MB is ≥1 mm. Some experts believe that BVS size should always be selected based on the proximal MB in order to allow performance of the proximal optimisation technique (POT)6. However, in our experience, the proximal MB diameter is usually within 0.5 mm of that of the distal MB, thus allowing the performance of a POT without the risk of disruption. Furthermore, the current scaffold balloons are fairly compliant and tend to dilate more at the shoulders of the balloon. We are concerned about the risk of distal edge dissection when sizing based on the proximal MB. The POT should be performed as normal with non-compliant balloons even at high pressure but respecting the dilatation limit of 0.5 mm larger than the scaffold implanted. Ormiston et al have demonstrated that proximal post-dilation of a 3 mm Absorb with a 3.5 mm non-compliant balloon inflated slowly to 14 atm does not cause any scaffold disruption7.
SB wires can be jailed as normal and removed without difficulty. Similar to metallic stents, the MB BVS should be re-crossed at the most distal strut to ensure optimal scaffolding of the SB ostium8. Residual SB stenosis after MB stenting can be treated with gentle SB balloon dilatation, followed by MB post-dilatation or FKBI to correct any MB scaffold distortion. Bench testing has shown that the struts of a 3.0 mm scaffold can be dilated towards the SB with even a 3.0 mm balloon without causing fractures as long as the inflation pressure is <10 atm7. As in the use of metallic stents, SB dilatation and FKBI are not mandatory, and in some cases the SB may unjail spontaneously as the scaffold reabsorbs.
FKBI CAN BE PERFORMED AT LOW PRESSURE WHEN NEEDED
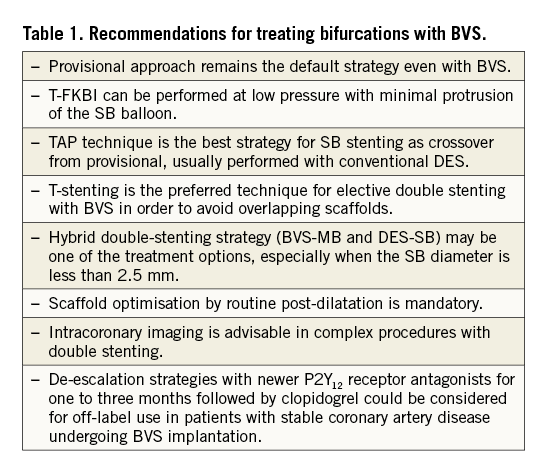
The majority of bifurcations in the GHOST-EU registry were treated with a simple strategy of MB stenting without any treatment of the SB. However, in selected cases of a suboptimal result at the SB due to plaque or carina shift, FKBI was performed. However, significant overlapping of the kissing balloons in the MB scaffold should be avoided and can result in scaffold disruption. FKBI performed at low pressure with minimal protrusion of the SB balloon (called T-FKBI or snuggling/hugging balloons) is feasible and does not appear to be associated with in vivo scaffold disruption (Figure 1). Ormiston et al have shown that, when performing T-FKBI, an inflation pressure of 5 atm is a safe threshold for two 3.0 mm non-compliant balloons in a 3.0 mm scaffold7. In patients who underwent systematic double stenting of both branches in GHOST-EU, T-FKBI was performed in half as compared to metallic stents where FKBI is considered mandatory. However, it must be noted that some operators prefer sequential SB and MB dilatation rather than FKBI, in order to avoid scaffold disruption and excessive elliptical expansion with FKBI.
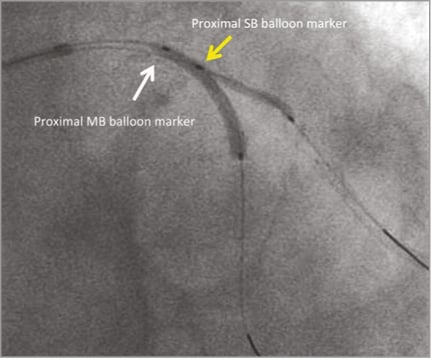
Figure 1. Fluoroscopic image demonstrating an example of T-kissing balloon inflation with minimal protrusion of the SB balloon into the MB.
THE TAP TECHNIQUE IS THE RECOMMENDED STRATEGY FOR SB STENTING AS CROSSOVER FROM PROVISIONAL
As in the use of metallic stents, the TAP technique is our preferred strategy for crossover from provisional when the SB needs to be stented9. The TAP technique is easy to perform and results in complete coverage of the ostium without excessive overlapping struts. We have successfully performed TAP stenting with another BVS (Figure 2) in some cases with large SBs and favourable anatomy (narrow angulation and minimal proximal MB disease). However, due to the large profile (1.4 mm) and strut thickness (157 µm) of BVS, it is not rare to fail to implant a BVS in the SB. Thus, the TAP technique is usually performed with a conventional DES (Figure 3), as a BVS may not pass so easily through the struts of the MB BVS. Irrespective of the stent implanted in the SB, it is important to pay particular attention to the sequence of deflation of the kissing balloons (main branch first, side branch last)10.
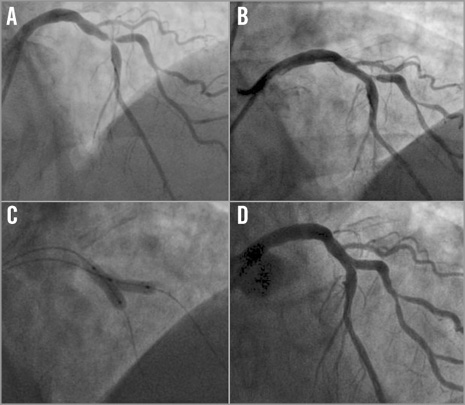
Figure 2. TAP with BVS for crossover from provisional. Angiographic images demonstrating a critical true bifurcation stenosis (Medina 1,1,1) involving the left anterior descending artery and first diagonal branch (A) treated initially with a provisional approach of implanting a BVS 3.5×18 mm in the MB. Despite T-FKBI, a significant stenosis remained at the ostial SB (B) and thus the SB was stented with a BVS 3.0×12 mm using the TAP technique (C) with an excellent final angiographic result (D).
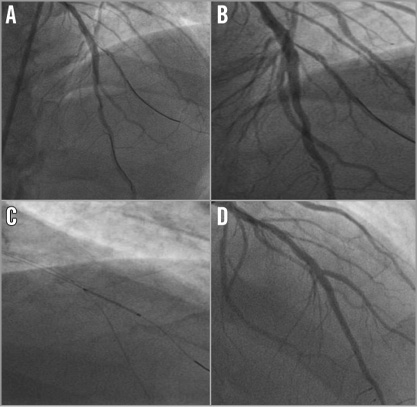
Figure 3. Hybrid TAP with DES on SB for crossover from provisional. Angiographic images after implantation of a BVS 3.0×28 mm on the left anterior descending artery demonstrating a significant stenosis of the diagonal branch (A). Dilatation of the SB with a drug-coated balloon resulted in a dissection (B) that was treated with TAP stenting with a 2.25×15 mm metallic DES (C), resulting in an excellent final result (D).
T-STENTING IS OUR PREFERRED TECHNIQUE FOR ELECTIVE DOUBLE STENTING WITH BVS IN ORDER TO AVOID OVERLAPPING SCAFFOLDS
T-stenting techniques are the first choice for planned double BVS implantation (Figure 4) while the culotte and crush techniques should be avoided to prevent excessive overlapping of the thick struts and structural deformation of the scaffold. However, T-stenting requires precise SB scaffold placement and a favourable bifurcation angle close to 90°. In shallow bifurcations, protrusion of the BVS into the MB at the carina level is unavoidable in order to cover the SB ostium fully and can result in an inadvertent crush of the SB scaffold and major scaffold fractures. In these cases, the crush may be performed as a rescue technique to correct the severe scaffold disruption of the crushed SB scaffold11. However, this should be avoided in favour of a hybrid strategy of DES on the SB and a BVS on the MB, as discussed below.
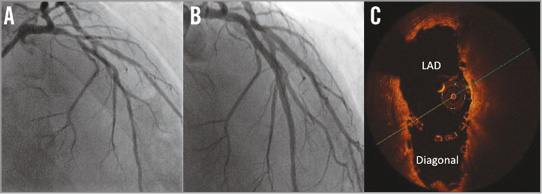
Figure 4. Elective T-stenting with two BVS. Angiographic images of a true bifurcation stenosis with diffuse disease of the left anterior descending artery and first diagonal branch (A) treated with T-stenting of the SB (BVS 3.0×28 mm and 2.5×28 mm) followed by implantation of two BVS (3.5×28 mm and 3.0×28 mm) in the MB (B). OCT confirmed an excellent result at the neocarina of the bifurcation and full coverage of the SB ostium without scaffold disruption (C).
A HYBRID DOUBLE-STENTING STRATEGY (BVS-MB AND DES-SB) MAY BE PREFERABLE TO A TWO BVS STRATEGY
In true bifurcations with significant and diffuse SB disease requiring elective double stenting, we prefer a hybrid strategy of implanting a DES in the SB, crushing the DES with a balloon, followed by implanting a BVS in the MB (Figure 5)12. This hybrid strategy is particularly useful when the SB diameter is less than 2.5 mm and/or the bifurcation angle is narrow.
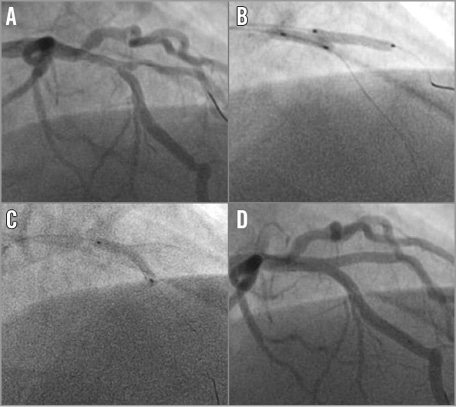
Figure 5. Hybrid mini-crush stenting. Angiographic images of a true bifurcation with a shallow angle of the SB (A) treated with mini-crush stenting of the SB with a 2.5×16 mm metallic DES (B), followed by implantation of a BVS 3.0×18 mm in the MB (C), resulting in an excellent final angiographic result at the bifurcation (D).
SCAFFOLD OPTIMISATION AND EFFECTIVE ANTITHROMBOTIC THERAPY ARE ESSENTIAL
BVS are less forgiving than DES and thus optimisation of the final result is even more important. Optimal lesion preparation, stepwise inflation and routine high-pressure post-dilatation with a non-compliant balloon are mandatory3. We also strongly advise that intravascular imaging be utilised to guide BVS optimisation and to evaluate malapposition and underexpansion when complex bifurcation techniques are performed. New adenosine diphosphate P2Y12 receptor antagonists, such as prasugrel and ticagrelor, were only given to a limited number of patients in the overall GHOST-EU registry (26.2%) and the bifurcation subgroup (19%). Although prasugrel and ticagrelor are currently approved for use in patients with acute coronary syndromes only, it has become our routine practice to recommend these more potent P2Y12 receptor antagonists in the first one to three months after BVS implantation and also in patients with stable coronary artery disease undergoing bifurcation percutaneous coronary intervention, with later transition to clopidogrel (“de-escalation strategy”), particularly if they have undergone complex procedures and are not at high risk of bleeding. However, data are needed to support this approach.
Conclusions
Bifurcations are increasingly being treated with BVS and in real-world practice account for about 25% of lesions undergoing BVS implantation. Bifurcations can be treated with BVS and metallic stents in a similar way. In particular, the provisional approach remains the default strategy. However, these devices are structurally different compared to conventional metallic stents and thus there are certain rules with regard to SB dilatation and kissing balloon inflation which need to be respected when implanting BVS in bifurcations in order not to damage their structural integrity, which as a result could increase the risk of events such as restenosis and thrombosis.
As these devices are less forgiving compared to DES, optimisation of the final result and appropriate antithrombotic therapy are essential when scaffolds are implanted in complex lesions. Data from the GHOST-EU and other registries will provide important information with regard to the safety and efficacy of BVS in bifurcations but will require long-term follow-up to evaluate whether BVS will have any advantage over DES.
Conflict of interest statement
C. Tamburino has received speaker’s honoraria from Abbott Vascular. D. Capodanno has received consulting honoraria from Abbott Vascular. The other authors have no conflicts of interest to declare.

