Mitral valve regurgitation (MR) is the most prevalent valvular heart disease in developed nations and is estimated to occur in up to 10% of the population older than 75 years of age1. Although surgical valve repair or replacement is considered to be the gold standard of care, at least half of all patients with secondary MR do not undergo curative surgery2. Such patients have expected mortality rates of 50% within five years3. There is therefore a considerable unmet clinical need to develop transcatheter devices to treat inoperable patients with symptomatic severe MR. Given the unqualified success of transcatheter aortic valve implantation (TAVI), a rush to develop transcatheter solutions for MR is axiomatic. Several transcatheter mitral repair devices have been commercialised in Europe and report variable success in reducing MR and improving symptoms. These devices, however, are not suitable for all patients, are technically challenging, and report high rates of prognostically significant residual MR. The development of transcatheter mitral valve replacement (TMVR) technology has the potential to complement repair devices in patients declined surgical intervention.
The considerable anatomical challenges associated with the development of TMVR devices have been clearly documented4: the valve system must be delivered to, anchor, and seal within a large, non-circular, saddle-shaped, highly dynamic, and acalcific annulus that is tethered to a complex, highly individualised, subvalvular apparatus, and intimately related to the left ventricular outflow tract (LVOT), the coronary sinus, and the left circumflex coronary artery. These anatomic hurdles have rendered TMVR device development a difficult and painstaking process.
Since the first human implant of the CardiAQ™ transcatheter mitral valve (Edwards Lifesciences, Irvine, CA, USA) on 12 June 2012, a dizzying number of transcatheter mitral valve systems have been developed and tested in animal models, each with unique anchoring, sealing, and deployment mechanisms. Human implants have been reported with at least nine devices: CardiAQ (Edwards Lifesciences); Tiara™ (Neovasc, Richmond, BC, Canada)5; FORTIS™ (Edwards Lifesciences)6; Tendyne (Abbott Vascular, Roseville, MN, USA)7; Intrepid™ (Medtronic, Minneapolis, MN, USA)8; Navi™ (NaviGate Cardiac Structures, Inc., Lake Forest, CA, USA); MValve (MValve Technologies Ltd, Herzliya, Tel Aviv, Israel); HighLife™ (HighLife Medical, Irvine, CA, USA)9; and Caisson (Caisson Interventional, Maple Grove, MN, USA). Importantly, early clinical results have been mixed with development programmes not infrequently suspended due to adverse events. Acute and subacute complications include: malposition, paravalvular leak, embolisation, left ventricular outflow tract (LVOT) obstruction, leaflet thrombosis, haemolysis, aortic valve injury, reduced ejection fraction, and stroke. Thirty-day mortality rates as high as 54% have been reported10. The impact of non-fatal periprocedural complications, such as paravalvular leak and LVOT obstruction, and the prevalence/impact of new device-related complications on longer-term clinical outcome remain unknown. Such information is essential to design clinical trials to compare the efficacy of TMVR to transcatheter mitral repair devices or indeed optimal medical therapy.
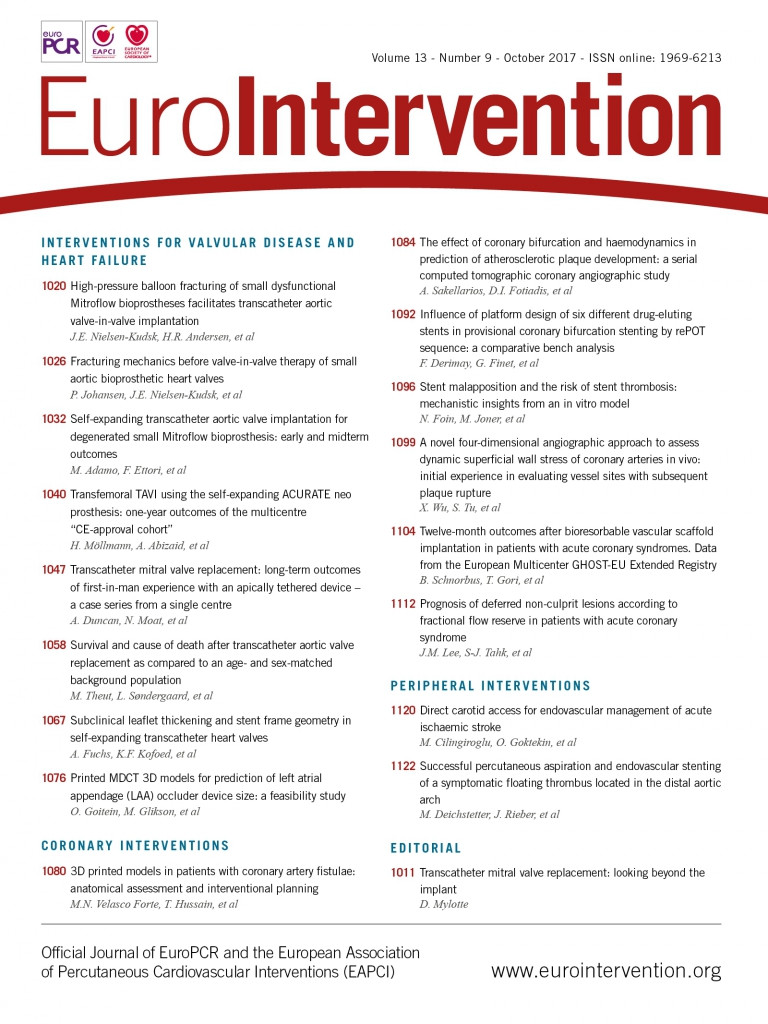
In this edition of EuroIntervention, Duncan et al report medium-term (two-year) results from the first five high-risk patients treated under compassionate use with the apically tethered D-shaped Tendyne TMVR system at the Royal Brompton Hospital, London11.
In this single-centre experience, all patients survived to hospital discharge, despite the occurrence of typical TMVR complications: one case of LVOT obstruction treated by LVOT stenting, one case of paravalvular leak, and one patient with mild haemolysis. Device thrombosis was a concern despite oral anticoagulation (OAC). There was one suspected transient ischaemic attack and one stroke death by 12 months (both patients with known atrial fibrillation and one was not compliant with OAC). Also, there was one additional case of echocardiographic device thrombosis after temporary discontinuation of OAC for atrial fibrillation ablation (resolved with resumption of OAC). At two years, four patients were alive, all with improved functional class and without new device-related complications. In particular, there were no concerns with the apical tether of the device which could, for example, lose traction as the left ventricle remodels.
These data are relevant and timely. Progress in the field of TMVR should not be defined simply by demonstrating transseptal feasibility, reduction in delivery catheter dimensions, or lower rates of periprocedural complications. The TAVI revolution has taught us to assess carefully the longer-term impact of “benign” periprocedural “hitches” which may have considerable bearing on clinical outcome (paravalvular leak). Identifying late complications after hospital discharge is of similar importance (late stent thrombosis). In this context, it is gratifying that, among patients with device-related complications such as LVOT obstruction, haemolysis, and paravalvular leak, stabilisation rather than progression was observed during follow-up. In contrast, the occurrence of device thrombosis in the current study is of considerable concern, especially given similar events with TAVI in the mitral position12, the FORTIS valve13,14, the Mitra-Spacer™ (Cardiosolutions, Bridgewater, MA, USA)13,14, and anecdotal unpublished reports of thrombosis with other TMVR systems. Insufficient OAC is frequently described in such cases, but clearly further study is required on the intensity and duration of coumadin therapy (± antiplatelet therapy) in TMVR recipients. Moreover, one could speculate that the efficiency of 4D multislice computed tomography in detecting subclinical valve thrombosis should be routinely applied at pre-specified time points after TMVR15. The success of TMVR may hinge on the early identification and treatment, and, ultimately, avoidance of valve thrombosis and its sequelae.