In the current issue of EuroIntervention, Stoller et al explore the relationship of coronary flow and pressure measurements before and after transcatheter aortic valve replacement (TAVR)1. The main findings of the study were that coronary flow reserve (CFR) is unchanged after TAVR, in comparison to fractional flow reserve (FFR) which is increased. The authors conclude that most of the change in FFR was due to a reduction in mean aortic pressure.
Understanding the significance of coronary artery disease is of growing importance, and avoiding unnecessary percutaneous coronary intervention (PCI) in an often elderly TAVR patient population is likely to reduce morbidity and mortality.
Several authors have explored the effects of severe aortic stenosis on coronary haemodynamics2-6. Whilst measuring pressure or flow individually can help to get an insight into the mechanisms which adversely alter coronary haemodynamics, a much greater understanding can be gained from simultaneous measurement of coronary pressure and Doppler flow2,3. Using such measurements, and applying wave intensity analysis (WIA), it is possible to isolate the interactions between pressure waves arising from the proximal part of the coronary artery (due to left ventricular ejection), and those originating from the distal coronary artery (due to compression and decompression of small microcirculatory vessels during the cardiac cycle)7 (Figure 1). Findings from these studies in patients without aortic stenosis have shown that, during systole, pressures at the proximal coronary artery are very similar to those originating from the distal coronary artery. This is because left ventricular pressures are very similar between the cardiac lumen, aorta, and the intramyocardial compartment. In diastole, the proximal pressure decays gradually, as the elastic portions of the aorta recoil after the aortic valve is closed. However, distal pressure falls rapidly due to active relaxation of the myocardium and decompression of small microcirculatory vessels. In comparison, in patients with severe aortic stenosis, despite higher ventricular pressures, in systole the pressure in the proximal coronary artery is lower than that arising from the distal artery2. This is due to a ventricular-aortic pressure gradient in the presence of aortic stenosis. In such cases, in diastole the proximal coronary pressure is lower and the fall in pressure at the distal coronary is attenuated due to altered relaxation patterns in the hypertrophied ventricle. During stress, the ability of the aortic stenotic heart to increase coronary flow is limited as it is already working at near maximal capacity, resulting in symptoms of chest pain and breathlessness8. In studies using WIA or CFR, the resolution of left ventricular hypertrophy over months leads to more normal relaxation patterns, and is associated with a return to normal physiological reserve4,5.
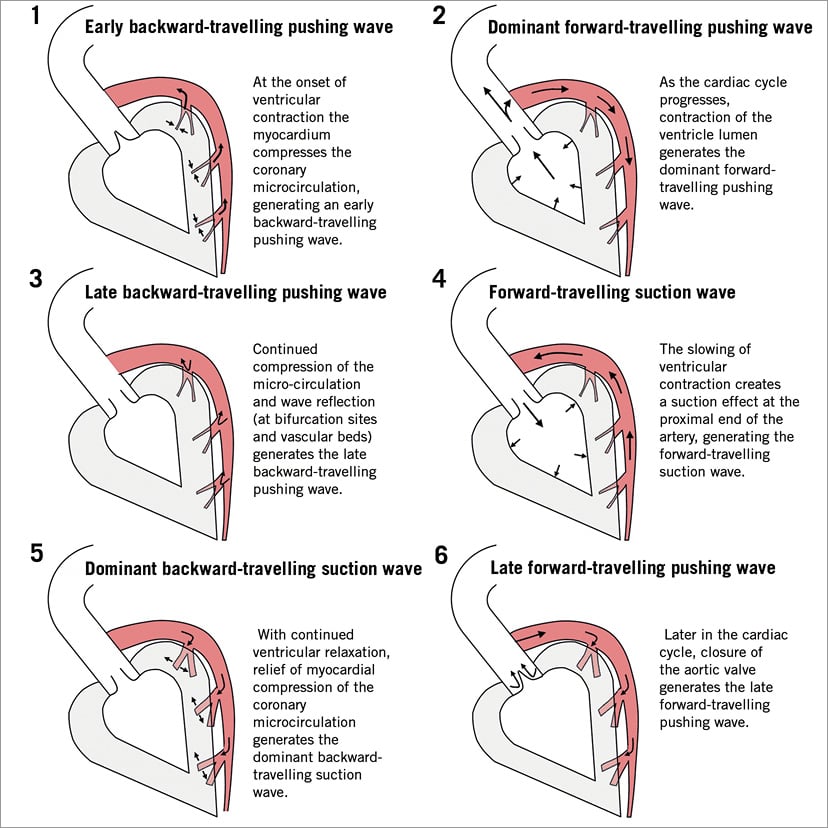
Figure 1. Sequence of energy waves in the human coronary artery during the cardiac cycle. Please note that the arrows represent direction of wave motion rather than direction of blood flow. From Davies et al7, with permission.
These findings have practical implications for the understanding and interpretation of the paper by Stoller et al. Recent invasive and non-invasive studies have shown that over time, as the left ventricular hypertrophy regresses, coronary flow and CFR increase4,5,9. In such cases, where coronary stenoses are present, it is likely that FFR would decrease as flow across the coronary stenosis is increased, thereby increasing the pressure ratio. This creates a significant clinical problem for FFR as stenosis assessment is markedly underestimated in the pre-TAVR setting, meaning that potentially significant coronary stenosis can potentially be inappropriately deferred. Stoller et al reported that FFR acutely increases following TAVR due to a fall in systemic pressures. This result directly opposes the recent findings from Pesarini et al who reported that FFR can either increase or decrease after TAVR, depending on the preprocedural FFR6. These conflicting results alert us to the complexities and difficulties in working within this complex and challenging environment.
It reminds us that factors other than treatment of the aortic valve, such as differences in anaesthetic protocols between studies, can inadvertently lead to changes in coronary haemodynamics and in this case FFR. Certainly, operators should always be careful when using adenosine in the presence of severe aortic stenosis as its effects are widely recognised to be blunted10, thereby inappropriately limiting the hyperaemic response. Pesarini et al demonstrated this in a recent study where no change between rest and hyperaemia pressure ratios was reported after administration of adenosine6. Furthermore, despite administration of adenosine, hyperaemic measures were actually higher than instantaneous wave-free ratio (iFR) measured at rest. Together, these observations lead to the conclusion that operators should be careful when using FFR in the presence of aortic stenosis in order to interpret the physiological severity of coronary stenoses.
From a physiological perspective, this phenomenon of hyperaemic blunting is not a problem for non-hyperaemic indices such as iFR. In iFR, measurements are made under rest conditions and as such do not require administration of adenosine11. Resting flow is very similar before and after TAVR2,3, meaning that when using iFR it is unlikely that coronary stenoses are inappropriately deferred, although it should be realised that validation studies are lacking to document thresholds for ischaemia in the setting of aortic stenosis.
Whilst we salute the work of Stoller et al which is both complex and demanding, we offer a word of caution. Pressure-derived thermodilution measures of resistance and coronary flow were developed in patients in the absence of aortic stenosis and as such no validation work has been performed. For practical reasons, a proximal stenosis in the left anterior descending coronary artery will be treated to avoid ischaemia due to rapid pacing during TAVR. The treatment of other lesions is questionable as it is conceivable that the patient’s symptoms are governed by the aortic stenosis. In this respect, validation studies using intracoronary haemodynamic parameters are eagerly awaited for guidance of coronary interventions in the presence of aortic stenosis. The intrinsic variability of measurement in a heterogenous group of patients with aortic stenosis means it is important to be cautious with definitive conclusions whilst the field is evolving.
Conflict of interest statement
J. Davies is a consultant for and receives research grants and IP royalties to Imperial College from Philips. J. Piek is a consultant for Philips/Volcano and a member of the Abbott Vascular Advisory Board.