Abstract
Aims: Single leaflet clip attachment (SLA) is a prevalent complication in percutaneous edge-to-edge repair of the mitral valve, leading to the recurrence of significant mitral regurgitation. The objective of this retrospective analysis was to evaluate a novel 3-D transoesophageal echocardiographic method for the assessment of clip attachment to the mitral leaflets.
Methods and results: We analysed a total of 87 patients treated for symptomatic mitral regurgitation. In 47 patients, clip attachment to the leaflets was assessed by conventional 2-D transoesophageal echocardiography supported by biplane TEE images (biplane TEE group). In 40 patients, clip attachment to the leaflets was assessed by the intraprocedural 3-D volume method in addition to the conventional method (volumetric TEE group). The primary endpoint was defined as clip complications consisting of SLA and clip displacement at any time after clip implantation. Clip complications occurred in nine patients (19.1%) in the biplane TEE group and in two patients (5%) in the volumetric TEE group (p=0.06). Regarding the grade of mitral regurgitation, in the follow-up period we observed a more pronounced deterioration in the biplane TEE group than in the volumetric TEE group.
Conclusions: These findings suggest that the additional use of 3-D volumetric transoesophageal echocardiography for the assessment of clip attachment to the mitral leaflets may contribute to a reduced rate of subsequent clip complications.
Introduction
Besides valve replacement, different methods of surgical mitral valve repair have been developed in the past decades and have become the preferred method of treatment for severe mitral regurgitation1. However, a significant number of high-risk patients are not eligible for any surgical approach.
The creation of a double orifice valve was first performed by Alfieri as a surgical approach to mitral valve repair for mitral regurgitation2,3. Based on this concept, the percutaneous edge-to-edge repair of the mitral valve using the MitraClip® system (Abbott Vascular, Redwood City, CA, USA) has recently been introduced and has been shown to be an effective and safe alternative method for patients with functional and degenerative mitral regurgitation4-10. Although in the EVEREST II trial percutaneous repair did not reduce mitral regurgitation as effectively as surgical mitral valve repair, the clinical outcome of patients treated by percutaneous repair was comparable to that of surgically treated patients. Moreover, percutaneous repair of the mitral valve has been shown to be associated with fewer major cardiovascular events and complications compared to surgical mitral valve repair5. Therefore, percutaneous repair of the mitral valve is an alternative particularly for patients at high risk for surgery6,7,9.
A crucial step during the percutaneous edge-to-edge repair of the mitral valve is the assessment of clip attachment to the mitral leaflets which may be challenging using 2-D transoesophageal echocardiography (2-D TEE). In the EVEREST I trial, single leaflet clip attachment (SLA) occurred in 9% of the patients, demonstrating the need for new techniques that allow a more reliable assessment of clip attachment4.
In current practice, the assessment of clip attachment is done by means of 2-D images in the intercommissural, LVOT and four-chamber view as well as the transgastric view. Recently, the introduction of biplane images has facilitated the assessment of clip attachment due to the acquisition of simultaneous perpendicular views. Furthermore, the recording of the grasping process gives valuable information about the amount of leaflet tissue fixed between the clip arms and the corresponding grippers.
We assessed the potential value of a novel method for the assessment of clip attachment using intraprocedural 3-D volume TEE.
Methods
STUDY DESIGN AND STUDY POPULATION
The objective of this retrospective analysis was to compare the standard approach for the assessment of clip attachment to the leaflets consisting of 2-D transoesophageal echocardiography supported by biplane TEE images (biplane TEE group) to intraprocedural 3-D volume transoesophageal echocardiography on top of the standard approach (volumetric TEE group).
Eligible patients with symptomatic degenerative (58 patients, 66.7%) or functional mitral regurgitation (29 patients, 33.3%) were primarily at high risk for conventional mitral valve repair or declined surgery. Key exclusion criteria were previous mitral valve clipping, recent myocardial infarction, active endocarditis or history of endocarditis and mitral valve orifice area <3.5 cm².
From June 2009 to April 2011 we treated 104 patients by percutaneous edge-to-edge repair of the mitral valve (109 MitraClip® procedures). The standard approach with 2-D TEE supported by biplane TEE images was predominantly used from June 2009 to June 2010. From July 2010 to April 2011 the 3-D volumetric method was used on top of the standard approach. In 100 cases (91.7%) the clipping procedure could be completed. Out of the 95 patients who met the inclusion criteria we were able to acquire follow-up data for 87 patients (91.6%), 47 patients in the biplane TEE group and 40 patients in the volumetric TEE group (Figure 1). In order to be included in this analysis at least two follow-up examinations, one to three days after and six weeks after clip implantation, had to be available. Mean follow-up was 9.3 and 8.2 months in the biplane TEE group and the volumetric TEE group, respectively.
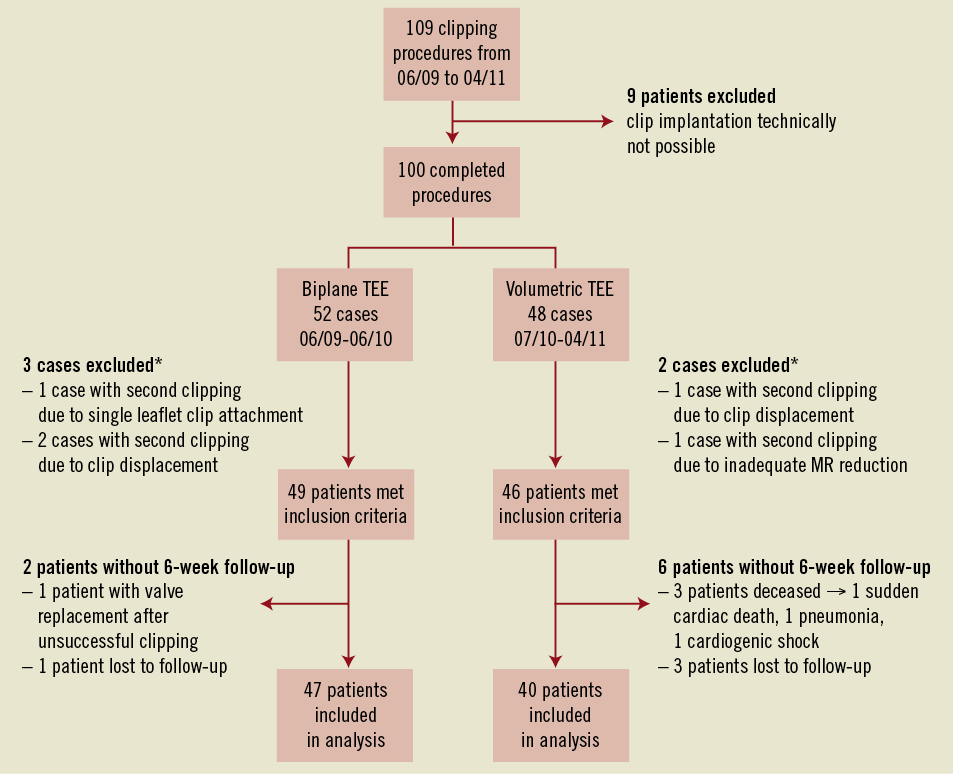
Figure 1. Enrolment and follow-up. MR: mitral regurgitation; pt.: patient; *in patients with two subsequent clipping procedures only the first procedure was included in this analysis
Echocardiographic guidance was provided by four independent echocardiographers with significant experience in TEE guidance of interventional procedures who consented to the standard course of action during a MitraClip® procedure.
PROCEDURAL TECHNIQUE
The procedures were performed under general anaesthesia with transoesophageal as well as fluoroscopic guidance as previously described5.
The echocardiographic studies were done using the Philips IE33 system and the Philips QLab quantification software (software version 8.1; Philips Healthcare, Best, The Netherlands).
During the percutaneous edge-to-edge repair procedure both mitral leaflets are grasped in order to coapt the valve after the clip is correctly positioned. The mitral leaflets should finally be fixed and held in place between the clip arm and the corresponding grippers.
In both groups we initially assessed clip attachment by 2-D echocardiography in the LVOT and four-chamber view with the highest frame rates possible (52 Hz). In addition to this, we assessed the attachment of the partially closed clip to the mitral leaflet by aligning the biplane axis in the LVOT view to both mitral leaflets fixed between the clip arms and grippers separately (frame rate 36 Hz). The leaflet fixed between the clip arm and the grippers could be assessed in the corresponding perpendicular intercommissural view (Figure 2). In order to delineate clip attachment, off-axis biplane imaging was used in addition to standard procedural views if applicable.
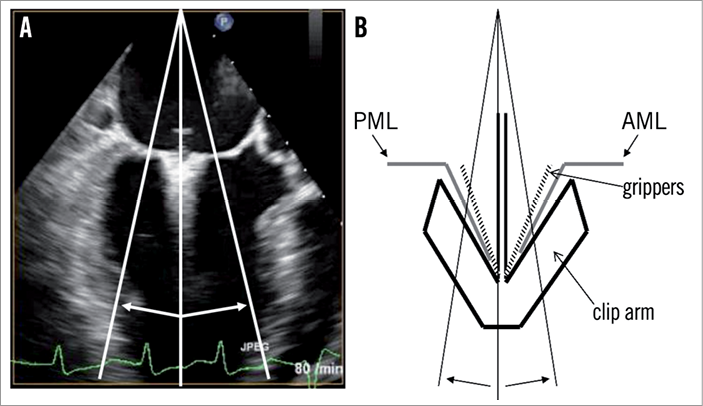
Figure 2. Patient with functional mitral regurgitation. A) Standard LVOT view with possible biplane TEE axes; B) Schematic magnification of the mitral leaflets fixed between the clip arms and grippers; An accurate alignment to both mitral leaflets fixed between the clip arms and grippers is technically not possible; PML: posterior mitral leaflet; AML: anterior mitral leaflet
In the volumetric TEE group, we used a novel method for the intraprocedural assessment of clip attachment in addition to 2-D echocardiography supported by biplane TEE images. Briefly, we acquired a full 3-D volume of the mitral valve consisting of four cardiac cycles in the intercommissural view (50-80°) during apnoea (frame rate 18 Hz). To analyse the clip attachment further during the procedure, we imported the volume into the 3-D QLab application on the IE33 system (Figure 3). The upper left quadrant (medial-lateral oriented vertical plane, here green) shows the intercommissural view, the upper right quadrant (anterior-posterior oriented vertical plane, here red) the LVOT view perpendicular to the intercommissural view and the lower left quadrant (horizontal plane, here blue) shows a transverse section of the mitral valve depicted from the left atrium.
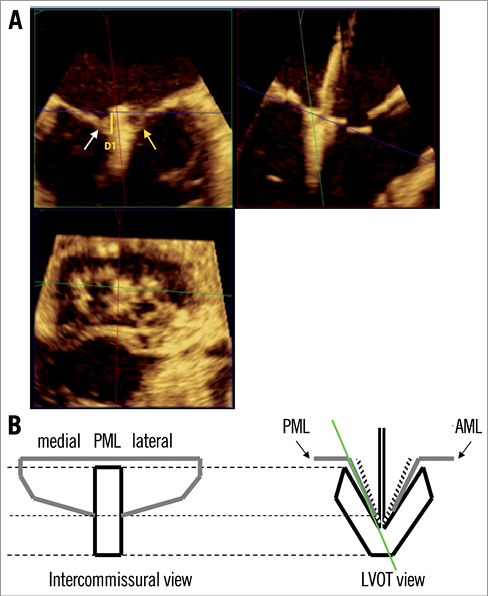
Figure 3. Clip attachment to the PML. A) Patient with functional mitral regurgitation. In the upper right quadrant the medial-lateral oriented plane (here green) is aligned to the PML fixed between the clip arm and the corresponding grippers. In the upper left quadrant the PML reaching medially (white arrow) and laterally (yellow arrow) into the clip is visualised. D1 (yellow bar) marks the part of the PML fixed into the clip. The lower left quadrant depicts a cross-section of the mitral valve with the tissue bridge connecting the AML and PML; B) Schematic magnification of the PML in the intercommissural view by accurate alignment of the medial-lateral oriented plane to the PML fixed between the clip arm and grippers. The schematic view corresponds to the upper right and upper left quadrant in the 3-D volume application, respectively. PML: posterior mitral leaflet; AML: anterior mitral leaflet; LVOT: left ventricular outflow tract
To visualise the mitral leaflets, we magnify the images and forward the dataset to mid systole in the cardiac cycle. In the upper left quadrant we align the anterior-posterior oriented vertical plane (here red), in the upper right quadrant we align the medial-lateral oriented vertical plane (here green) with the axis of the MitraClip®, and the horizontal plane (here blue) is placed on the top edge of the MitraClip® perpendicular to the axis of the clip.
Next, the anterior and posterior mitral leaflets are analysed separately. To evaluate proper attachment of the clip to the posterior mitral leaflet we now align the medial-lateral oriented vertical plane (here green) with the PML fixed between the posterior clip arm and the corresponding grippers of the partially closed clip (Figure 3). In the lower left quadrant the medial-lateral oriented plane can be adjusted to the orientation of the commissure if necessary. In the upper left quadrant the PML reaching medially and laterally into the clip can now be visualised. The part of the PML fixed into the clip can be determined by measuring the distance between the lowermost part of the leaflet and the top edge of the clip (yellow bar). Six millimetres of the leaflet had to be fixed between the clip arm and the corresponding grippers in order to be considered adequate. To analyse attachment of the clip to the anterior mitral leaflet, the medial-lateral oriented plane has to be adjusted to the AML as described for the PML (Figure 4).
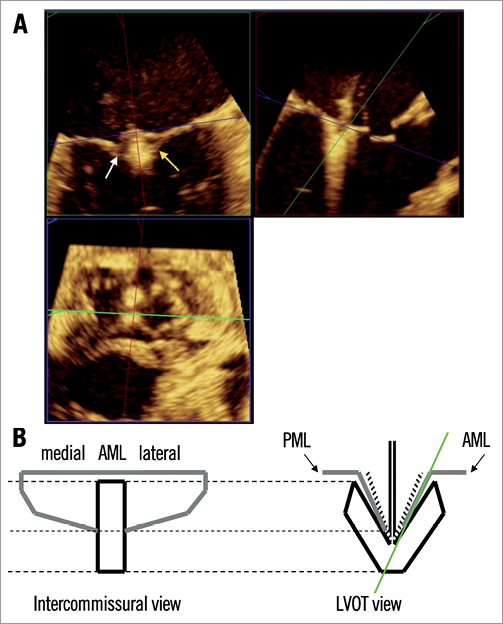
Figure 4. Clip attachment to the AML. A) Patient with functional mitral regurgitation. In the upper right quadrant the medial-lateral oriented plane (here green) is aligned to the AML fixed between the clip arm and the corresponding grippers. In the upper left quadrant the AML reaching medially (white arrow) and laterally (yellow arrow) into the clip is visualised. The lower left quadrant depicts a cross-section of the mitral valve with the tissue bridge connecting the AML and PML. There the medial-lateral oriented plane was adjusted to the orientation of the commissure; B) Schematic magnification of the AML in the intercommissural view by accurate alignment of the medial-lateral oriented plane fixed between the clip arm and grippers. The schematic view corresponds to the upper right and upper left quadrant in the 3-D volume application; PML: posterior mitral leaflet; AML: anterior mitral leaflet; LVOT: left ventricular outflow tract
ECHOCARDIOGRAPHIC FOLLOW-UP
After percutaneous edge-to-edge repair of the mitral valve transthoracic echocardiographic follow-up examinations were performed up to two years after clip implantation. Regular examinations were scheduled one to three days, six weeks, six months and 12 months after clip implantation. Echocardiographic examinations were performed more than 12 months after clip implantation if clinical deterioration occurred. In case of transthoracic echocardiographic examinations with a suspicion of clip displacement or single leaflet clip attachment with recurrence of significant mitral regurgitation transoesophageal echocardiography was performed to clarify the aetiology of the mitral regurgitation. Mitral regurgitation was quantified using standard 2-D and Doppler echocardiography and graded from 1+ to 4+11. In cases with a suspicion of clip displacement a second echocardiographer involved in the clipping procedures assessed the grade and aetiology of mitral regurgitation.
ENDPOINTS
The primary endpoint of this analysis was defined as single leaflet clip attachment (SLA) or clip displacement leading to the recurrence of significant mitral regurgitation at any time after successful clip implantation. Single leaflet clip attachment was defined as complete detachment of the clip from a single mitral leaflet. Clip displacement was defined as displacement of the clip from a single mitral leaflet without complete disruption of the tissue bridge. Secondary endpoints were defined as grade of mitral regurgitation directly after clip implantation and at the time of the last follow-up available as well as the procedure time in the two groups.
DATA ANALYSIS
We used Fisher’s exact test to compare categorical variables and the Mann-Whitney U test for the comparison of continuous variables. A two-tailed p-value <0.05 was regarded as statistically significant.
Results
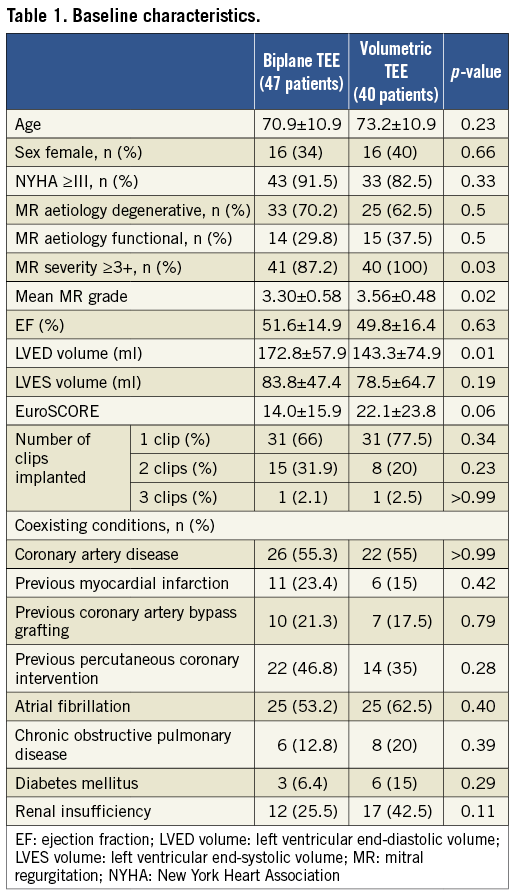
We analysed the rate of single leaflet clip attachment or clip displacement of a total of 87 patients, 47 patients in the biplane TEE group and 40 patients in the volumetric TEE group. Regarding the baseline characteristics of the two groups, the LVED volume was significantly higher in the biplane TEE group. The mean MR grade was significantly higher in the volumetric TEE group (3.56±0.48) compared to the biplane TEE group (3.3±0.58). Furthermore, we observed a trend towards a higher calculated logistic EuroSCORE in the volumetric TEE group (22.1%) than in the biplane TEE group (14.0%) indicating an increased risk of cardiac surgery for this patient population (Table 1)12. The number of clips implanted in both groups was comparable. In 66% of the patients in the biplane TEE group and in 77.5% of the patients in the volumetric TEE group one clip was implanted (p=0.34) whereas in 31.9% of the patients in the biplane TEE group and 20% of the patients in the volumetric TEE group two clips were implanted (p=0.23). Three clips were implanted in one patient of each group.
Overall we observed 11 clip complications (12.6%) including four SLAs (4.6%) and seven clip displacements (8%) which led to the recurrence of significant mitral regurgitation. We did not observe clip embolisations. A case of SLA is shown in Figure 5 as well as in Moving image 1 and Moving image 2.
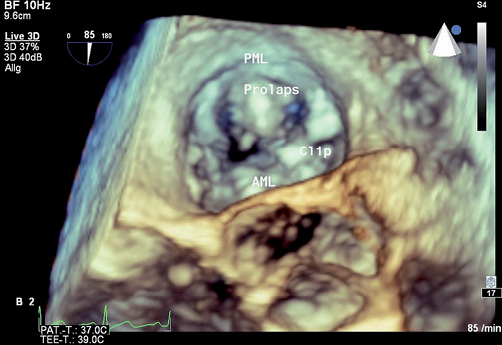
Figure 5. Patient with flail leaflet of the P2 segment leading to severe degenerative mitral regurgitation. Single leaflet clip attachment after detachment of the clip from the PML within one month after successful mitral valve clipping. Moving image 1 and 2 online show the corresponding clips. PML: posterior mitral leaflet; AML: anterior mitral leaflet
In the conventional biplane TEE group we observed nine clip complications (19.1%) including four SLAs and five clip displacements. Three clip complications occurred within the first days after the procedure, one occurred within the first six weeks after the procedure and four occurred within the first six months after the procedure. Only one clip complication occurred about two years after the procedure.
There were two clip displacements (5%) in the volumetric TEE group, one within the first days after the procedure and one within six weeks after the procedure (Figure 6). We did not observe SLAs in the volumetric TEE group. All confirmed clip complications except one clip displacement in the volumetric TEE group occurred in patients treated for degenerative mitral regurgitation.
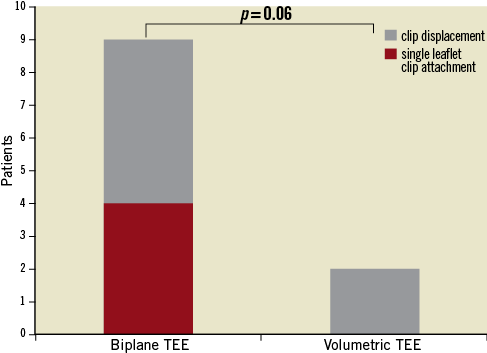
Figure 6. Assessment of SLA and clip displacement.
Regarding the grade of mitral regurgitation, the success rate directly after percutaneous edge-to-edge repair (4.3% vs. 12.5% MR ≥3, p=0.24) and at the time of the last follow-up (25.5% vs. 35% MR ≥3, p=0.36) was comparable in the biplane TEE group and in the volumetric TEE group, respectively. In the follow-up period we observed a significant deterioration of the MR grade in both groups that was more pronounced in the conventional biplane TEE group (Table 2, Figure 7). Overall, in relation to the grade of mitral regurgitation before clipping, at the time of the last follow-up available we observed a comparable MR grade reduction in the volumetric group and in the biplane TEE group, respectively (–1.31 vs. –1.17) (Table 2).
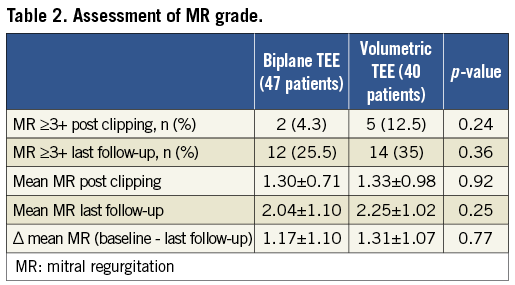
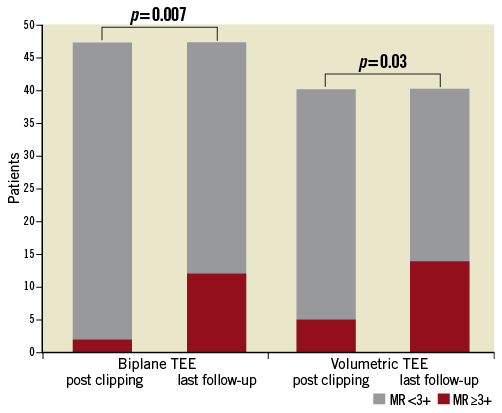
Figure 7. Assessment of MR grade post clipping and at the time of last follow-up. MR: mitral regurgitation
The additional use of the intraprocedural 3-D volume method did not lead to a prolongation of the mean procedure time. We observed a mean procedure time of 225±133 min in the volumetric TEE vs. 227±103 min in the biplane TEE group (p=0.6).
To emphasise further the clinical potential of the 3-D volume method described above, we provide a clinical case where the attachment of the clip to the PML was critical due to a limited length of the PML (9 mm). The grasping of the PML appeared good (Moving image 3) and the clip has been shown to be attached to the PML using 2-D TEE (Moving image 4) and 2-D TEE supported by biplane images (Moving image 5). The 3-D volumetric analysis gave us the crucial additional information that laterally 7 mm and medially 5 mm of the PML was fixed between the clip arm and the corresponding grippers (Figure 8, black bars).
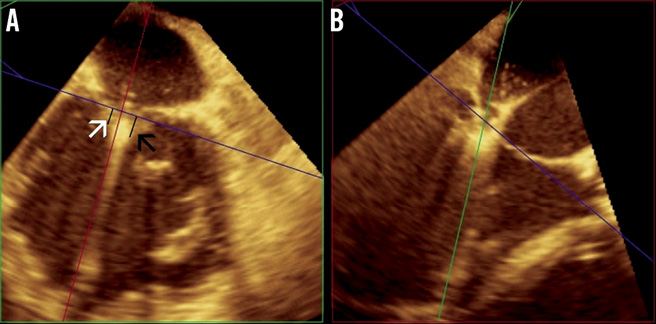
Figure 8. Patient with severe functional mitral regurgitation. Intraprocedural 3-D volume analysis of clip attachment to the PML. In the right quadrant the medial-lateral plane (here green) is aligned to the PML fixed between the clip arm and the corresponding grippers. In the left quadrant the PML reaching medially (white arrow) and laterally (black arrow) into the clip is visualised. Medially 5 mm and laterally 7 mm of the PML are fixed between the clip arm and grippers (black bars). Moving images 3, 4 and 5 provide further imaging of this MitraClip procedure.
Discussion
In this analysis of our data we show that the additional intraprocedural 3-D volume analysis of clip attachment to the mitral leaflets is feasible and does not prolong the mean procedure time. We observed that the rate of SLA and clip displacement was lower when we used 3-D volume analysis on top of the standard method consisting of 2-D TEE supported by biplane TEE images. Hence, 3-D imaging using volumetric analysis in addition to standard techniques may help to confirm a secure clip attachment during the mitral valve clipping procedure.
Although percutaneous edge-to-edge repair of the mitral valve has been shown to be a safe and effective non-surgical method for the treatment of functional as well as degenerative mitral regurgitation4,5,7,9, in the EVEREST II trial percutaneous coaptation of the mitral leaflets could not reduce mitral regurgitation as effectively as mitral valve repair5. One of the most critical steps during the MitraClip® procedure is the assessment of clip attachment after both mitral leaflets have been grasped with the clip. In this context, the relatively high frequency of single leaflet clip attachments could have contributed to this finding. However, several factors including left ventricular remodelling following strain changes, annulus flattening and the absence of a mechanism that constricts the annulus might also explain the superiority of surgical mitral valve repair concerning MR grade reduction.
SLA occurred in 9% of the treated patients in the EVEREST I trial leading to the recurrence of significant mitral regurgitation4. In line with these results, we observed SLA in approximately 9% of the treated patients using the standard approach for the assessment of clip attachment. There were no SLAs in the volumetric TEE group resulting in an overall rate of SLA of 4.6% in the whole study population of 87 patients. Considering both SLA and clip displacement, we observed a rate of clip complications of approximately 19% using the standard approach as opposed to 5% using intraprocedural 3-D volume analysis. These data support the concept that 3-D volumetric analysis in addition to standard techniques may help to improve the evaluation of clip attachment to the leaflets during the MitraClip® procedure, eventually reducing the occurrence of SLA and clip displacement.
Regarding the grade of mitral regurgitation, our analysis shows a comparable success rate directly after the procedure and at the time of the last follow-up available in the biplane TEE group and in the volumetric TEE group, respectively. The more pronounced deterioration of the MR grade in the biplane TEE group in the follow-up period can be attributed to the higher rate of SLA and clip displacement in the biplane TEE group. However, the higher mean end-diastolic volume in the biplane TEE group could also explain the more pronounced MR grade deterioration by less favourable left ventricular remodelling after the clipping procedure.
Overall the application of the novel 3-D volume method did not lead to superior results compared to the standard approach. This is probably due to the significantly higher initial MR grade in the 3-D volume group. Furthermore, we treated a more complex patient population at higher risk for cardiac surgery in the volumetric TEE group compared to the biplane TEE group (mean logistic EuroSCORE 22.1% vs. 14.0%).
In the EVEREST II trial, the rate of grade 3+ or 4+ mitral regurgitation at 12 months follow-up was reported to be 21% in the percutaneous repair group. Overall, at the time of the last follow-up available, we observed a rate of grade 3+ or 4+ mitral regurgitation of 29.9%. We attribute the difference in these results to the higher number of high-risk patients not eligible for surgery who were included in this analysis.
All except one clip complication occurred in patients treated for degenerative mitral regurgitation, suggesting the particular usefulness of our novel method for this subset of patients. One reason for this could be that the implanted clip is exposed to more stress in degenerative than in functional mitral valve disease. Regarding the baseline characteristics, the LVED volume in the biplane TEE group was significantly higher than in the volumetric TEE group. This potential risk factor could have influenced the higher rate of SLA and clip displacement in the biplane TEE group due to the increased horizontal stress the implanted clip is exposed to in a dilated ventricle.
Furthermore, the intraprocedural 3-D volume analysis of clip attachment could be of particular use in patients with degenerative mitral regurgitation due to the atypical orientation and increased mobility of the placed clip, which may complicate the use of the standard method for the assessment of clip attachment.
The majority of SLAs and clip displacements (all except one) occurred within the first six months after the implantation of the MitraClip®. This result is consistent with reported data that an organised fibrous capsule develops within 300 days after the clip implantation, stabilising the clip13.
Limitations
Results have to be interpreted with caution due to the low number of patients and events in both groups. Furthermore, data were collected retrospectively. In the volumetric TEE group the intraprocedural 3-D volume analysis was used in addition to the conventional 2-D method supported by biplane TEE images to provide additional information. In the volumetric TEE group slightly more patients did not have a six-week follow-up (Figure 1) and the mean follow-up duration in the volumetric TEE group (8.2 months) was shorter than in the biplane TEE group (9.3 months). This could partly explain the reduced rate of SLA and clip displacement in the volumetric TEE group.
Most importantly, the volumetric TEE method was predominantly used in the later patients suggesting the learning curve with all steps of the MitraClip® procedure could have contributed to the reduced rate of SLA and clip displacement in the volumetric TEE group. However, among the 49 consecutive patients who met the inclusion criteria in the biplane TEE group, clip complications were equally distributed suggesting the initial lack of experience did not substantially influence the data presented here (three clip complications in roughly the first third of patients, three complications in the middle third and three complications in the last third of patients).
Due to the above-mentioned limitations, our data have to be considered as hypothesis-generating. A prospective randomised comparison of volumetric TEE to biplane TEE is necessary to clarify the value of volumetric TEE for the assessment of clip attachment to the mitral leaflets.
Conclusions
The assessment of clip attachment to the leaflets is one of the critical and most difficult steps in percutaneous edge-to-edge repair of the mitral valve. SLA and clip displacement are a clinical problem that has been shown to occur in a relevant number of treated patients, and leads to the recurrence of significant mitral regurgitation4. Here we present a new method using intraprocedural 3-D volume transoesophageal echocardiography which has the potential to reduce the rate of SLA and clip displacement if used on top of the standard method. Our data indicate that the volumetric TEE method may be of particular use for patients with degenerative mitral regurgitation.
Conflict of interest statement
F. Michalk, J. Mehilli, A. Kastrati and J. Hausleiter received speaker honoraria from Abbott Vascular. The other authors have no conflicts of interest to declare.
Online data supplement
Moving image 1 and Moving image 2. Patient with flail leaflet of the P2 segment leading to severe degenerative mitral regurgitation.
3-D (Moving image 1) and 2-D (Moving image 2) demonstration of single leaflet clip attachment after detachment of the clip from the PML within one month after successful mitral valve clipping. PML: posterior mitral leaflet; AML: anterior mitral leaflet
Moving image 3. Patient with severe functional mitral regurgitation. Grasping of the PML appears good.
Moving image 4. Patient with severe functional mitral regurgitation. Assessment of clip attachment to the PML using 2-D TEE shows the PML being fixed between the clip arm and grippers.
Moving image 5. Patient with severe functional mitral regurgitation. Assessment of clip attachment to the PML using 2-D TEE supported by biplane TEE images shows the PML being fixed between the clip arm and grippers.
Supplementary data
To read the full content of this article, please download the PDF.

