Stent for Life Initiative and 2016 Stent for Life Forum
The Stent for Life Initiative (SFL), an EAPCI and EuroPCR alliance, was established in 2008 as an international network of national cardiac societies and partner organisations to address inequalities in patient access to primary PCI, a lifesaving revascularisation treatment for ST-segment elevation acute myocardial infarction (STEMI)1-3. SFL supports the implementation of the ESC Clinical Practice Guidelines (Guidelines) at national and regional levels through the formulation of strategies, the creation and implementation of educational programmes, and through advocacy activities and awareness campaigns4. Currently, 21 national cardiac societies and partner organisations from Europe, Africa, Asia and South America are part of SFL. When the SFL Forum 2016 gathered in Prague on 26 and 27 February 2016 for the 5th SFL annual conference, SFL Russia (represented by B.G. Alekyan and V. Ganyukov) and SFL South Africa (represented by R. Delport and A. Snyders) signed the SFL Declaration and joined the Initiative.
Barriers to overcome when developing an SFL regional STEMI network
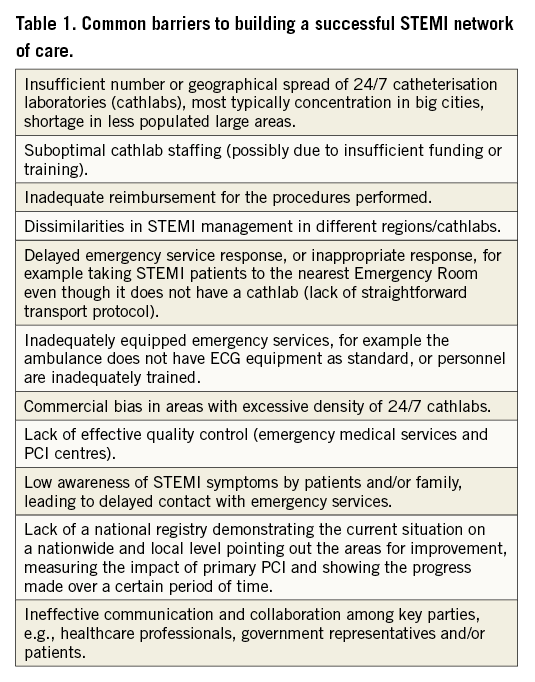
Situational analyses from SFL participating countries have shown that the adherence to guidelines is influenced by many factors and varies from country to country, and from region to region5. An in-depth understanding of healthcare system-level barriers and unique challenges in the regional context facilitates the development of more effective strategies for improving the quality of the STEMI system of care in a given country (Table 1).
Importance of the role of government - experience from SFL Bulgaria, SFL Spain, SFL Turkey and SFL Egypt
Government support and involvement is crucial for the success of SFL in each country. This is why continuous efforts are needed to convince the government representatives to integrate SFL into a supported national programme. The most frequent problems are associated with difficult access to the Minister of Health, so good relationships with decision makers in the government can promote collaboration. In countries with marked decentralisation of the authorities it takes even more effort to address and iron out differences between and within regions, such as in Spain or Italy. Frequent changes in government, especially in the Ministry of Health, such as those faced in Egypt or in Saudi Arabia, can hamper ongoing political support. However, once achieved, governmental support greatly assists the accomplishment of the objectives and the action plan. In due course, SFL leaders have become members of national government bodies as advisors or directors, e.g., in Romania, Turkey, Spain and Saudi Arabia.
SFL results at three years and the implementation of SFL principles under complex political situations
SFL country representatives from Bosnia-Herzegovina and Ukraine, who joined SFL in 2012, reported at the SFL Forum 2016 that geographic mapping, situational analysis, proper planning and execution are critical success factors for building SFL regional STEMI networks, even under complex political conditions.
One hundred and fifty-three primary PCI/1 million inhabitants were performed in 2012 in Bosnia-Herzegovina, and 338 primary PCI/1 million were performed in 2015, representing an increase in the percentage of primary PCIs performed from 19% to 41% of all STEMI patients hospitalised, while the number of facilities providing primary PCI care increased from five to six.
Results from SFL Ukraine are encouraging as well. There were only three STEMI networks providing primary PCI in 2012 in the Ukraine, covering 13% of the country’s territory. In three years, that number has increased to 14 STEMI networks involved in SFL covering 60% of the territory. The number of primary PCIs performed has increased from 75 primary PCI/1 million inhabitants to 146 primary PCI/1 million, in 2012 and 2015, respectively.
Results from SFL Bosnia-Herzegovina and SFL Ukraine, together with SFL countries who joined the programme in 2009, e.g., Bulgaria, France, Greece, Romania, Serbia and Turkey, and who presented their three-year results at the SFL Forum 2012, demonstrate that building SFL regional STEMI networks is effective and can be accomplished in relatively short periods of time. Partnerships and cooperation between STEMI referral hospitals, primary PCI hospitals and EMS teams are a prerequisite. Transportation and clinical pathway protocols and an acute coronary syndrome (ACS) registry should be developed and endorsed by regional and/or national government officials.
Delegates concluded that stakeholders in the implementation of SFL originate from different areas. They have various backgrounds (medical, industry, political, etc.), but they have a common target – to reduce mortality and morbidity in ACS patients by improving access to primary PCI. By combining their efforts towards that common target, stakeholders can boost the effect on reduced costs. It is the strength of the SFL Initiative that it is able to unite partners from different areas, with various skills, sharing common goals.
Building SFL regional STEMI networks and emergency services infrastructures in emerging countries
SFL Argentina, SFL Mexico and SFL Tunisia presented the one-year progress of SFL implementation in their respective territories. SFL leadership in Argentina focused its efforts on aligning all three cardiac societies on programme objectives and on integrating SFL into a national cardiology programme. Country situational mapping was initiated: 228 primary PCI centres and 64 non-PCI centres participated in the SFL country mapping phase. Preliminary results indicate that 39,810 PCIs and 8,470 primary PCIs were performed in 2014, and the primary PCI utilisation is 202/1 million inhabitants in Argentina. Next, 12 pilot centres were selected to initiate development of an SFL regional STEMI network. Three-year objectives will be agreed upon after barrier identification in each SFL pilot region in Argentina.
The SFL Forum expert group agreed that primary PCI should be the preferred treatment not only in developed countries, but in emerging countries as well. If a STEMI patient is located close to a primary PCI centre with a presumed short transportation time to hospital, primary PCI is the preferred treatment. For patients in rural areas, with suspected long transportation time to PCI-capable hospitals, the pharmacoinvasive strategy with thrombolytic therapy followed by catheterisation and PCI if indicated within three to 24 hours of thrombolysis would be utilised. Results from SFL emerging countries presented at the SFL Forum 2016 conference, e.g., India, Argentina, Mexico, and South Africa, revealed that building and integrating a regional emergency medical services infrastructure is a key prerequisite to support STEMI patients’ access to a pharmacoinvasive strategy in those areas where primary PCI is not accessible in a given timeframe, and a mechanism for inter-hospital transfer of patients is required. The STEMI India “Hub and Spoke” model, as well as the STEMI Sri Lanka “Wagon Wheel” model were discussed and it was confirmed that priority should be given to building regional STEMI networks around existing primary PCI centres.
Results from the SFL economic model
The SFL economic model was developed to demonstrate the financial, economic, and clinical benefit of timely STEMI admissions and primary PCI treatment. The SFL economic model uses country- or region-specific data to evaluate the impact of the Stent for Life Initiative based on increased treatment with primary PCI versus the alternative approaches of thrombolytics or no reperfusion. Outcomes from an increased primary PCI mix were measured against a scenario assuming that the SFL Initiative never occurred and rates remain unchanged.
For Portugal, the SFL economic model was measuring data from 2010 to 2013. STEMI PCI was 264 per million in 2010 when the SFL Initiative began and increased to 341 per million by 2013. On-time STEMI admissions also increased over this time period. The net result of these improvements was a reduction in mortality of 414 lives and nearly 46 million USD of variable cost savings. The burden of disease also decreased by almost 150 million USD.
For Russia, we focused on the Kemerovo region where most of the SFL gains have been achieved, measuring from 2011 (the start of the SFL Initiative) to 2014. PCI, as a percent of on-time STEMI admissions, increased from 12% in 2011 to 33% in 2014 (which corresponds to 272 STEMI PCI per million inhabitants). During this time period, there was approximately 1.83 million USD of investment in cathlabs and in the interventional cardiology workforce. However, the productivity savings of 5.7 million USD due to higher rates of PCI more than offset this amount.
For Spain, SFL looked at the Basque country region, as the data were most consistent from this area. Over the course of the SFL Initiative, the initial STEMI PCI per million was estimated at 254 in 2012 and grew to 341 by 2015, while on-time admissions improved by five percentage points. Due to the relatively high gross domestic product per capita and low inflation rate, significant cost savings of approximately three million USD were achieved in an area of less than 700,000 people.
These three impressive examples of economic analysis show the transformative power of STEMI network implementation, resulting in many lives saved along with reduced spending.
STEMI patient education - improving the quality of care of patients surviving an acute heart attack
It has been observed that a level of lay public education and patient literacy influences the access of STEMI patients to a reperfusion therapy as well as their outcomes when discharged from the hospital.
The SFL Initiative is calling for collaboration with the European Association of Cardiovascular Prevention and Rehabilitation (EACPR) and the Council of Cardiovascular Nursing and Allied Professions (CCNAP) to address the early critical phase secondary prevention after STEMI, beginning immediately after the initial cardiac event during hospital stay.
Preliminary results from situation mapping in SFL pilot countries participating in the SFL survey, Portugal, Romania, Spain, Greece and the Czech Republic, reveal that a great disparity exists among countries, country regions and hospitals, and confirms a lack of implementation of structured secondary prevention intervention at discharge from a primary PCI centre. To improve patient-related adherence to prevention therapy, Contract4Life/After a Heart Attack programme will be implemented in selected SFL pilot countries. A nurse-assisted education programme will be delivered in selected primary PCI centres to evaluate its impact on the re-hospitalisation rate of STEMI patients, and STEMI patient risk profile after 12 months.
Conclusion
The SFL Forum 2016 was, once again, a great and stimulating opportunity for SFL country delegates from four continents to share their experiences. For the first time, measurable achievements after only three years of SFL implementation were reported, highlighting the important medical and economic impact of the SFL alliance. Even greater effects can be anticipated in Russia and South Africa, two large countries which have now joined the programme.
Conflict of interest statement
Z. Kaifoszova is managing Stent for Life on behalf of EAPCI and EuroPCR. The other authors have no conflicts of interest to declare.