Abstract
Primary percutaneous coronary intervention (PPCI) is the recommended treatment for patients with acute ST-segment elevation myocardial infarction (STEMI). A survey conducted in 2008 in the European Society of Cardiology (ESC) countries reported that the annual incidence of hospital admissions for acute STEMI is around 800 patients per million inhabitants. The survey also showed that STEMI patients’ access to reperfusion therapy and the use of PPCI or thrombolytic therapy (TT) vary considerably among countries. Northern, Western and Central Europe already had well-developed PPCI services, offering PPCI to 60-90% of all STEMI patients. Southern Europe and the Balkans were still predominantly using TT and had a higher proportion of patients who were left without any reperfusion treatment. The survey concluded that a nationwide PPCI strategy results in more patients being offered reperfusion therapy. To address the inequalities in STEMI patients’ access to life-saving PPCI and to support the implementation of the ESC STEMI treatment guidelines in Europe, the Stent for Life (SFL) Initiative was launched jointly by the European Association of Percutaneous Cardiovascular Interventions (EAPCI) and EuroPCR in 2008. The aim of the SFL Initiative is to improve the delivery of life-saving PPCI for STEMI patients. Currently, 10 national cardiac societies support the SFL Initiative in their respective countries. SFL national action programmes have been developed and are being implemented in several countries. The formation of regional PPCI networks involving emergency medical services, non-PPCI hospitals and PPCI centres is considered to be a critical factor in implementing PPCI services effectively. Better monitoring of STEMI incidence and prospective registration of PPCI in all countries is required to document improvements in health care and to identify areas where further effort is required. Furthermore, studies on potential factors or characteristics that explain the national penetration of PPCI are needed. Such knowledge will be necessary to increase the effectiveness and efficiency of the implementation, and will be the first step in ensuring equal access to PPCI treatment for STEMI patients in Europe. Establishing the delivery of PPCI in an effective, high-quality and timely manner is a great challenge.
Introduction
Primary percutaneous coronary intervention (PPCI) and thrombolytic therapy (TT) are the two alternative reperfusion strategies for ST-elevation acute myocardial infarction (STEMI) patients. Randomised clinical trials have shown that PPCI is superior to TT in reducing mortality, reinfarction and stroke1. These benefits are probably due to obvious advantages for PCCI, such as a much higher early mechanical reperfusion rate, the ability to treat simultaneously the underlying stenosis, and the lower risk of severe bleeding, in particular intracranial bleeding. The European Society of Cardiology (ESC) STEMI treatment guidelines recommend PPCI as the preferred treatment if: 1) the first medical contact (FMC) – balloon time is less than 90-120 minutes, 2) the interventionalist is experienced (i.e., performs more than 75 PCIs per year), and 3) the patient is treated in a high-volume centre (i.e., one in which more than 36 PPCIs are performed per year)2.
PPCI in Europe
EUROPEAN SURVEY 2008
In order to obtain realistic data about how patients with acute myocardial infarction (AMI) were treated in Europe, a survey of the ESC countries was conducted in 20083. In each country, data were collected on existing national STEMI or PCI registries, STEMI epidemiology and treatment, and PCI and PPCI centres and procedures. For the 30 ESC countries participating, results from national and/or regional registries were included in the survey. If no registry data were available, estimates from leading national experts were accepted.
The survey found an annual incidence of hospital admissions for AMI around 1,900 patients per million inhabitants with an incidence of STEMI of about 800 per million. The dominant reperfusion strategy was PPCI in 16 countries and TT in 8 countries. PPCI was used in 5-92% of all STEMI patients and TT in 0-55% of all STEMI patients. Reperfusion treatment (PPCI or TT) was used in 37-93% of STEMI patients. In countries where TT was the dominant reperfusion strategy, significantly fewer patients received reperfusion therapy. The number of PPCIs per million inhabitants per year varied between 20 and 970.
Furthermore, the mean population served by a single PPCI centre varied between 0.3 and 7.4 million. In countries offering PPCI services to the majority of their STEMI patients, a STEMI centre covered a population of between 0.3 and 1.1 million. In-hospital mortality of all consecutive STEMI patients varied between 4.2% and 13.5%, between 3.5% and 14% for patients treated by TT, and between 2.7% and 8% for patients treated by PPCI. The time reported from symptom onset to FMC varied between 60 and 210 minutes; in TT patients FMC to needle time varied between 30 and 110 minutes; in PPCI-treated patients FMC to balloon time varied between 60 and 177 minutes.
The survey confirmed that STEMI patients’ access to reperfusion therapy and the use of PPCI and/or TT varies considerably among European countries. A nationwide PPCI strategy for STEMI was associated with more patients being offered reperfusion therapy. Northern, Western and Central Europe already had well-developed PPCI services, offering PPCI to 60-90% of all patients. Southern Europe and the Balkans were still predominantly using TT. Where this was the case, a higher proportion of patients was left without any reperfusion treatment. The survey results also suggested that countries with a mean population of 750,000 PPCI per centre performing 600 PPCIs annually per million inhabitants should have been able to meet the need for treating all STEMI patients with PPCI. Countries in which nearly all existing PCI centres offered 24-hour seven-days-a-week (24/7) PPCI services appeared to obtain the best results. Overall, the survey showed that there was a substantial heterogeneity of reperfusion practices in Europe and that there were many opportunities to improve care3.
Learning best practice from other countries
The Zwolle group from the Netherlands performed the first large European studies on PPCI4. In other pioneer countries like the Czech Republic and Denmark PPCI was implemented nationwide more than 10 years ago after publication of the PRAGUE and DANAMI-2 studies5-7. Countries like Germany and Switzerland have also been using a high rate of PPCI for a decade. In Sweden, PPCI was almost fully implemented after the publication of national registry data showing better outcome for PPCI than TT8. In the UK, strong political initiatives based on evidence including national registries have boosted the implementation of PPCI during the last four years.
These examples show how results of national randomised trials and registries, sometimes combined with the presence of strong individuals, have convinced national politicians to encourage the implementation of PPCI.
In 2009, Knot et al published an article describing the management of STEMI in five European countries: Austria, the Czech Republic, Denmark, the Netherlands and Sweden9. The article highlighted several key factors necessary for successful implementation of PPCI programmes and effective PPCI network building. These critical success factors were identified based on the experience of the five best-practice countries. The publication revealed several important key areas necessary for successful implementation of PPCI such as:
– stakeholder involvement (professional societies, government, patients)
– establishment of 24/7 PPCI networks to cover the STEMI population
– the launch of transportation protocols to bypass the nearest hospitals without catheterisation laboratories
The publication was meant to serve as a guide and source of inspiration for other countries which are aiming to implement PPCI.
The Stent for Life Initiative
The paper by Knot et al was part of the Stent for Life (SFL) Initiative, which was launched jointly by the European Association of Percutaneous Cardiovascular Interventions (EAPCI) and EuroPCR in 2008. National cardiac societies from Bulgaria, France, Greece, Serbia, Spain and Turkey signed the SFL Declaration at the ESC Congress in Barcelona in 200910. The aim of the SFL Initiative is to improve STEMI patients’ access to life-saving PPCI, thereby reducing mortality and morbidity10. Countries with an unmet medical need for the optimal treatment of STEMI and countries where the use of PPCI can be encouraged were invited to join the SFL Initiative. Currently, 10 countries participate in the initiative –Bulgaria, Egypt, France, Greece, Italy, Portugal, Romania, Serbia, Spain and Turkey– and several other countries are interested in becoming affiliated.
The main strategic objectives of the SFL Initiative are: 1) to design and implement national action programmes to increase PPCI access to more than 70% of all STEMI patients; 2) to achieve PPCI rates of more than 600 per million population per year; and 3) to offer a 24/7 PPCI service in PPCI centres in order to cover the needs of the STEMI patient population.
The SFL Initiative is a practical approach with the mission “to improve the delivery and patient access to the live-saving indications of PCI thereby reducing the mortality and morbidity of patients suffering from acute coronary syndromes”. The aim of SFL is to support national implementation programmes. Knowledge and tools are offered from the SFL central organisation in order to help create tailored national or regional action programmes, as the barriers for implementation of PPCI are different in the participating countries. Thus, countries such as Greece, France, Italy, Spain and Turkey have chosen a regional approach in their management of STEMI and implementation of PPCI programmes. They have developed and implemented specific collaboration protocols and guidelines for transfer to PPCI centres. Bulgaria, Egypt, Portugal, Romania and Serbia are examples of countries with a national approach to the implementation of PPCI with direct support from the government in the implementation of the STEMI treatment guidelines.
The progress of the implementation of PPCI in the SFL target countries has been described recently11 and will also be presented in more detail in other articles in this supplement.
Potential barriers for implementation
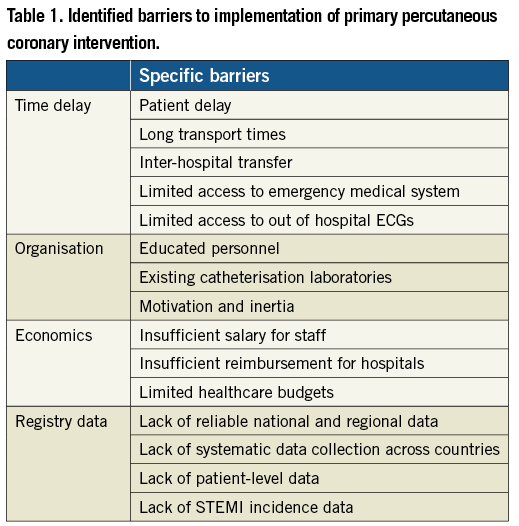
The explanation for the lack of complete PPCI implementation in Europe requires more research. However, some barriers identified in the literature on implementation of health care technology in general might provide preliminary indications to guide this research. A literature review from 2005 on the studies of health technology diffusion in the 30 countries within the Organisation for Economic Co-operation and Development (OECD) showed interplay between multiple factors as the explanation for cross-country variation in the diffusion of various markers of health care quality12. The strongest correlation was found between technology diffusion and economic variables, such as the total health expenditures per capita and economic incentives to hospitals. The diffusion model was based on a theory used in health promotion planning, which was found very useful in explaining the interplay of multiple factors influencing the diffusion. Figure 1 shows a similar model giving an overview of some of the significant factors and structures considered to play a part in the introduction of new technology11,12. Implementation of new technology usually calls for multidisciplinary action across departmental and organisational boundaries. Existing literature identifies timely delivery, organisation and training, economic schemes or other factors as key players for the implementation of PPCI (Table 1)14-17.
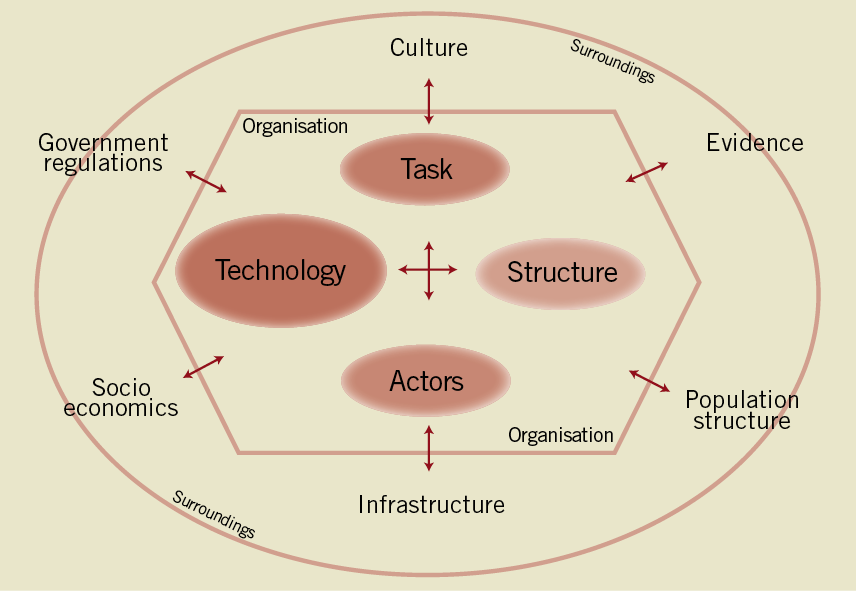
Figure 1. Factors and structures considered to play a role in the introduction of new health technology (modified from ref 15).
Reducing time delay
The success of PPCI depends greatly on timely access, and system delays have been shown to be independently associated with mortality and development of heart failure14-16. Across Europe, the majority of STEMI patients present to community hospitals without PPCI facilities, so the need for well-functioning regional pre-hospital systems for early diagnosis and immediate transport to a PPCI centre is crucial11. Patients diagnosed by pre-hospital electrocardiogram (ECG) and transferred directly to a PPCI centre have a lower mortality18. The difficulty of providing timely access to appropriate facilities within the recommended time frame (90-120 minutes or less from first medical contact to initiation of reperfusion) is one of the major barriers to PPCI delivery. Studies have shown that widespread adoption of PPCI was potentially limited by anticipated transport delays and practicalities associated with transfer of patients from noninvasive hospitals to PPCI centres14,17,19-24. However, randomised studies and meta-analyses suggest that PPCI is superior to TT even when it requires inter-hospital transfer19,25, and that the advantages of PPCI over TT are limited to hospitals with a high or intermediate volume of cases. These findings have prompted some European countries to establish PPCI networks, in which patients bypass or are transferred immediately from local hospitals to specialist centres to reduce system delay26,27. These networks have shown impressive reductions in case fatality rates 18,24,27,28. This approach requires centralised and coordinated communication and transfer organisation between local hospitals, PPCI hospitals, and the emergency medical system (EMS). Networks require the availability of ambulances with 12-lead ECG capability and appropriately trained paramedics, which is not the case in several European countries today11. The influence of EMS organisation in Europe on the implementation of PPCI has not yet been estimated, but is probably important. Because of these access and infrastructure issues, and the critical importance of time to treatment, TT may be generally preferred in areas, e.g., in mountainous regions, that cannot meet the time goal for PPCI29. However, even in patients for whom TT is successful, the guidelines now recommend angiography and in many cases percutaneous coronary intervention (PCI) within 24 hours, which further underlines the need to establish PPCI networks30.
The formation of regional networks involving emergency medical services (EMS), non-PCI hospitals and PPCI centres could be necessary to implement PPCI services effectively. We suggest that such regional networks should cover an area comprising a population of approximately 0.5 million (0.3-1 million); a smaller area could lead to a suboptimal workload and thus suboptimal treatment effectiveness, while a larger area may cause PCI centre overload9. This can be achieved only by respecting the right of local hospitals and local cardiologists to take care of their patients after primary PCI has been completed and the patient is stabilised. Transfer of the patient after successful PPCI to the local hospital nearest to the patient’s home for medical treatment and rehabilitation should be encouraged9.The number of PPCI centres necessary to cover the needs of the STEMI population in one country should be defined by the national stakeholder such as the national society of cardiology and the ministry of health. PPCI national or regional networks should be established and transportation protocols implemented. Non-PCI hospitals should have a qualified cardiologist available 24/7 so that they are able to provide appropriate care for AMI patients after the intervention. The primary transport of STEMI patients by EMS from the site of FMC to hospital should bypass the nearest non-PCI hospital. Experience shows that well-trained nurses or paramedics may achieve similar effectiveness to physicians in the triage and transport of AMI patients. In other words, EMS staff training is more important than EMS staff structure30. All EMS ambulances should be equipped with resuscitation facilities and the necessary medications. The patient must be taken from the EMS vehicle directly to the catheterisation laboratory. This can only be achieved if the catheterisation laboratory has been informed in advance of the arrival of a STEMI patient. Immediately after the diagnosis has been established, the catheterisation laboratory should be informed and given the patient’s approximate time of arrival. In this way delays can be minimised and the recommended timeframe (less than 90-120 minutes from FMC to initiation of reperfusion) can often be achieved17.
Organisation and training
Delivery of PPCI requires appropriate cardiac catheterisation laboratories with specialised and experienced staff. Lack of cardiac nurses, technicians, and other trained staff may threaten the sustainability of PPCI. Outcomes from STEMI are related to appropriate staff education and specialisation, as well as a sufficient volume of procedures26,32,33. An extensive survey in Canada identified the lack of catheterisation laboratories and experienced staff as primary barriers to complete implementation17.
In 2008, the UK National Health Service published a comprehensive report on PPCI implementation13. Based on qualitative interviews, the report highlighted some important barriers towards implementation of PPCI amongst the employees. They expressed concerns about the availability of sufficient equipment, training, and hospital beds for unplanned admissions. They also worried about the disruption in the planned working day programme delaying elective cases, and some staff were not happy to work across role boundaries14. Another principal barrier was the 24-hour requirement for specialist staff to be available to respond in an emergency32 and a resistance towards a change in working hours.
In Europe, the optimal rate of use of PPCI in STEMI is uncertain, so there are no standards for organisation of systems or training of clinicians and other health personnel26,34-36. Appropriate staffing is essential to achieve anticipated outcomes, and the requirement for additional resources might be a major barrier to achieve the staff requirements in some countries. Regional networks with specialist PPCI centres as suggested in the SFL programme might be the best solution to overcome this barrier24,27,37,38.
Modern health care systems are complex and often specialised in many branches that correspond to several broad disease categories. Launching a successful programme for PPCI requires the commitment and collaboration of all members of the health care team. Unfortunately, few investigations of the potential organisational barriers to providing PPCI have been performed39-43, but it is likely that regional networks could shift patient load between different hospitals. This change would require reorganisation of hospital structures, formations of new organisational networks, and formal partnership agreements across municipalities14, all of which may encounter political resistance38.
Economics
Recent studies emphasise that PPCI is socio-economically cost-effective, regardless of the high costs of establishing the technology14,44. This cost-effectiveness is due to a reduction in hospital duration, fewer readmissions, a reduction in subsequent coronary angiography, and patients returning to the labour market faster14,44. Even if these elements do not offset the higher initial implementation cost, the net effect on costs may be justifiable if PPCI results in an improvement in health outcomes14,44. However, PPCI is closely linked to timely delivery of the treatment and unlikely to be cost-effective if significant time delays are present14. More studies are required to explore this conceivably important barrier to implementation.
In some European countries, current funding systems could create structural barriers and disincentives to implementation46. In US conducted studies, concerns have been raised about resistance to PPCI from non-PCI-capable hospitals. Non-PCI-capable hospitals anticipate the loss of revenue sources and desirable patients with the implementation of PPCI, mainly because the demographics of STEMI patients favour older and better-insured patients38,47,48. Losses for the individual hospital would need to be weighed against the benefits in terms of reduced mortality and morbidity, and the potential cost savings for the global healthcare system.
Several studies have acknowledged the important influence of payment methods on technology diffusion14,49. The reimbursement schemes both for physicians and hospitals can be a strong incentive for technology use. Since PPCI delivery should be available 24 hours a day, national agreements on payment for out-of-hours work can play a tremendous role in the distribution. The direct influence has not yet been explored in newer studies, but Ayanian et al conducted a study using a large sample of community-based physicians who evaluated the necessity of cardiac catheterisation after an acute myocardial infarction50. For this group of patients, physicians employed by managed-care organisations were far less likely than physicians in the fee-for-service sector to believe that angiography was necessary, and invasive cardiologists were more likely than non-invasive cardiologists to believe that the procedure was necessary50.
In the face of cost-containment activities, considerably more information is needed about the kinds of financial arrangements and incentives that influence physicians’ approaches to providing care. Empirical research will be particularly valuable in this respect43. More detailed description of the importance of economics is given in a separate paper of this supplement.
The need for cardiac registries in Europe
The 2008 survey was the first large-scale study to register the access to reperfusion therapy in Europe. Since very few comprehensive national or international data registries exist, the survey data were often based on expert estimations, causing a potential overestimation or underestimation of the distribution of reperfusion therapy in Europe. Other international and national studies concerning the use of PPCI confirm that variation in the access to PPCI is a substantial problem both within and across countries in Europe3,51-54.
To our knowledge, no comprehensive overview of existing cardiac registries in Europe is available. Some national and regional registries and initiatives have been established to register the PPCI activities, such as the Berliner Heart registry, Hellenic PCI registry in Greece, Il GISE in Italy (registration made by the national cardiology society), MINAP in England, RO-STEMI in Romania, and Portugal, where the National Department of Health is responsible for collecting national indicators of cardiovascular diseases. Moreover, within the last few years, the European Society of Cardiology has focused on the need for comprehensive registries for cardiology. Nevertheless, country-based or hospital-based registries are often based on voluntary work, and frequently this lacks funding. At the same time, these registries are further hampered by the variety of data collection methods as well as a lack of sufficient coverage for them to be representative of the population-wide medical system targeting cardiac disease. Moreover, remarkably few sources exist for incidence data on ischaemic heart disease49. The incidence serves as an approximation to the underlying demand for health care services, in other words as a source for organisation of a PPCI strategy. Systematic documentation and surveillance of health status, treatment schemes and treatment outcomes of heart patients are needed in all European countries49-56. Databases are important to address the full diversity of access to treatment among regions and countries, to target initiatives including implementation strategies, and to compare healthcare systems against each other. Obtaining adequate data to conduct precise quantitative comparisons of the impact of technological change on changes in expenditures and outcomes across countries will help to redirect resources to other parts of the healthcare system49. National and international collaborations with the establishment of minimum aggregated data sets are needed. Examples of such successful collaborations have been seen in other medical settings57.
SFL public campaign
The timely delivery of treatment is dependent on the patients’ ability to recognise heart attack symptoms and to call the EMS (patient delay). The general population’s knowledge regarding the symptoms of AMI and unstable angina pectoris, the absolutely key role of time (every minute counts), their country’s unique national emergency phone number, AMI treatment (including PPCI) and basic cardiopulmonary resuscitation are probably the most important parts of the entire process. SFL countries have reported a lack of public knowledge in these fields. Extensive surveys were launched in Portugal and France to define the need for public education. Both surveys confirmed that the public awareness of acute coronary syndrome (ACS) symptoms and of the need to call EMS quickly is low. In Portugal, 77% of patients with ACS arrive at hospital by their own means of transport, e.g., by taxi or private vehicle. In France, fewer than 50% of patients with ACS called the EMS directly11.
To address this issue, the SFL Initiative has recently developed a public awareness campaign with the slogan “ACT NOW. SAVE A LIFE”. This campaign aims to educate patients to act quickly and to call the unique national emergency phone number in order to be transferred by ambulance to a PPCI centre, bypassing the nearest hospital without PPCI facilities. Bulgaria, Portugal, Spain and Turkey are SFL pilot countries where the “ACT NOW. SAVE A LIFE” campaign has been rolled out. Egypt, France, Italy and Romania have already implemented widespread public education campaigns to educate the public about the symptoms of ACS and the need to call the EMS quickly. The impact of the “ACT NOW. SAVE A LIFE” campaign will be measured and a case study will be published in 2012.
2011 SFL survey
In order to see if reperfusion therapy practices have changed since 2008 a new SFL survey in the ESC countries is currently on-going. The national society presidents of the 53 ESC countries have been contacted and encouraged to help obtain data on reperfusion strategies in their country. So far 32 countries have responded to the survey. We hope that the results will enable us to monitor the changes in reperfusion therapy that have occurred in the last three years.
Conclusions
Since the time the SFL Initiative was launched, several activities have been initiated in the participating countries. Preliminary reports suggest that major increases have been seen in the numbers of PPCIs performed. Improvements in STEMI mortality rates have also been observed. A detailed report describing the situation of STEMI treatment in Europe will be presented at the ESC Congress in August 2012 in Munich.
Implementation of PPCI has multiple barriers and involves patients, physicians, support staff and policymakers. Close co-operation among the key healthcare stakeholders has proved to be very effective in achieving the appropriate implementation of PPCI programmes in SFL countries. The SFL Initiative has proved to be an effective model of collaboration combining support and participation from interventional cardiologists, government representatives, EMS, industry partners and patients.
Conflict of interest statement
The authors have no conflict of interest to declare.