Abstract
At the moment of signing the Stent for Life (SFL) Initiative on August 31st, 2009, it was shown that, in Serbia during 2008, 48% of patients with ST-elevation myocardial infarction (STEMI) did not receive any reperfusion and only 19% and 33% received primary percutaneous coronary intervention (p-PCI) or hospital thrombolysis, respectively. However, during 2009, there was a trend towards a substantial increase in p-PCI procedures. This was the result of the commitment of cardiologists, the contract signed by the Health Insurance Fund (HIF) for remuneration of catheterisation laboratory (cathlab) staff for each p-PCI procedure (2005), and the provision of new cathlabs by the Ministry of Health (MOH). The number of PCI centres and trained cardiologists has been rising simultaneously. Direct mobile telephone contact with interventional cardiologists has facilitated the transport of patients directly to cathlabs (from 7.5% before 2009 to 34.2% in 2010 and 2011). Although the number of patients treated with p-PCI is increasing (2006 - 647 p-PCIs; 2007 - 1,248 p-PCIs; 2008 -1,794 p-PCIs; 2009 - 2,468 p-PCIs; 2010 - 3,216 and 2011 - 3,498 p-PCIs), the percentage of patients who are treated within 120 minutes of establishing a diagnosis (first medical contact) is still not satisfactory (38%).
Abbreviations
ACS: acute coronary syndrome
AMI: acute myocardial infarction
cathlab: catheterisation laboratory
CCU: coronary care unit
CME: continuous medical education
EMS: emergency medical service
ER: emergency room
FMC: first medical contact
HIF: Health Insurance Fund
MOH: Ministry of Health
OH: other hospital
PHC: primary health centre
p-PCI: primary percutaneous coronary intervention
SFL: Stent for Life Initiative
STEMI: ST-elevation myocardial infarction
Introduction
In a survey conducted in 30 European countries, despite having almost the lowest GDP, Serbia had an equal number of primary percutaneous coronary interventions (p-PCI) for the treatment of patients with ST-elevation myocardial infarction (STEMI) as some of the developed countries, although that number was significantly below that achieved in the countries who were the front-runners1. Since then, Serbian interventional cardiologists, supported by the Ministry of Health, have been determined to introduce p-PCI as routine in the everyday management of patients with STEMI, urged by their own experience (since the 1980s, when p-PCI was occasionally performed during working hours only) and new cathlabs provided in the mid 2000’s, as well as the contract signed by the Insurance Fund of Serbia (IFS) for remuneration of cathlab staff for each p-PCI procedure in 2005. The survey showed that in Serbia 48% of patients with STEMI did not receive any reperfusion therapy and only 19% and 33% received p-PCI or hospital thrombolysis1, respectively, so it was necessary to achieve a big change in mentality, i.e., to create a “reperfusion culture”. Inclusion of Serbia in the Stent for Life (SFL) Initiative lunched by EAPCI/ESC was perfectly timed to help a mentality change in order to create a reperfusion culture that resulted in the continuous increase in the number of patients treated by p-PCI for STEMI. The MOH provided several new cathlabs as well as employing and training more interventional cardiologists in order to achieve the SFL goal of more than 600 p-PCIs per million inhabitants per year by 2015. A direct mobile telephone contact through 069 INFARKT with an interventional cardiologist on duty, and delegating the responsibility to the first medical contact doctor (FMC: emergency medical service (EMS) doctors as well as doctors working in primary and secondary care institutions) to establish diagnosis of STEMI, facilitated transporting patients directly to cathlabs (from 7.5% before 2009 to 34.2% in 2010 and 2011). Accordingly, an increase in the use of aspirin from 13.1% to 38.3% and clopidogrel from 12.7% to 34.2% by EMS was registered. However, the constant substantial increase in the number of patients treated by p-PCI each year (2006 - 647 p-PCIs; 2007 - 1,248 p-PCIs; 2008 - 1,794 p-PCIs; 2009 - 2,468 p-PCIs; 2010 - 3,216 p-PCIs and 2011 - 3,498 p-PCIs), has not been accompanied by a significant increase in the number of STEMI patients treated within 120 minutes of FMC2,3, which reached only 38%. The percentage of patients (only 53.3%) who have been transported by EMS points to the fact that more mentality and organisational changes are required. One of the biggest barriers has been to change the previous practice of transporting patients to the nearest institution even if it is a non-PCI one. A specifically designed reperfusion form has been proposed as part of official medical records which would facilitate these changes4.
The specific goal through the SFL Initiative for Serbia is to increase the availability of reperfusion therapy for patients with STEMI, and thus to reduce mortality and morbidity. To achieve that, the goal has been set to increase progressively the number of p-PCI procedures every year, in order to achieve 600 procedures performed per million inhabitants by 2015, respecting recommended timeframes proposed by the European Society of Cardiology/EAPCI guidelines.
Changing mentality
Awareness of the importance of early reperfusion in STEMI patients is still the challenge in Serbia. Building the “reperfusion culture” in the population, in the EMS and in primary healthcare physicians is very hard, and is a long-term job. Through the guidelines and through education, projects and various activities (working groups of interventional cardiology, working groups for urgent medicine, NGOs and associations) the MOH is trying to implement new roles, protocols and specific guidelines to improve the outcomes of STEMI patients. In December 2011, the new “Guidelines on Ischaemic Heart Disease” were published in Serbia. Capacity building was followed by CME on STEMI: twice a year from 2007 to 2011 in the City Emergency Health Centre in Belgrade and at least 10 SFL sessions during the most important meetings held in Serbia, some of them with ESC and/or EAPCI participation. STREAM and COMFORTABLE studies, in which Serbia has been included, have also helped mentality and organisational changes.
Changing the mentality of EMS teams and physicians in primary health centres (PHC)
The Group for the Implementation of SFL constantly agitates for STEMI patients to be driven not to the nearest hospital, but directly to the cathlab. It has been proposed to shorten admission procedures for STEMI patients, and agreement has been reached to bring patients directly to the cathlab, bypassing the emergency room and the coronary care unit (CCU). In order to track the time and treatment of patients with STEMI, a specially designed reperfusion form has been introduced. It consists of (Figure 1) a patient’s general data, time, place of the chest pain occurrence, the provoking factor, the treatment (especially administration of aspirin and clopidogrel), and the route by which the patient arrived for p-PCI. Pre-hospital/hospital diagnosis of STEMI has been delegated to EMS services and other non-PCI centres. The “reperfusion form” has been recommended as an official and mandatory medical document through the new “Law on Medical Records” (which the MOH haven’t yet finished). The MOH and Health Secretaries in Belgrade and Nis have recommended that all EMSs and CCUs should use this document in the trial period, but with poor compliance. It is still very hard to change that decade-long organisational habit and mentality of EMS physicians to drive the AMI patient to the nearest facility, even though the nearest hospital does not necessarily have the resources for p-PCI.
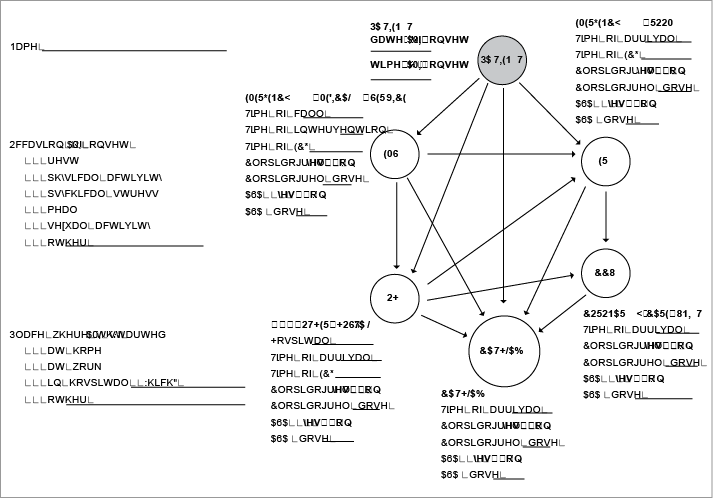
Figure 1. Reperfusion form.
Within the EU project on EMS, coordinated by the MOH (2009 to 2010), a few issues have been improved: the elaboration of recommendations, the elaboration of the maps to set up defibrillators in public places, development of the unified system of training of medical personnel of the EMS (according to the accredited standards), and elaborating the number of operators in the emergency communication control centres. The “Protocol for Pre-hospital Diagnosis and Treatment of ACS” was published in 2010, and about 1,800 printed copies were distributed to all EMS and primary healthcare physicians5. The aim was to improve the diagnosis, triage and treatment of patients with chest pain and to facilitate decision making for pre-hospital thrombolysis.
For faster emergency response, it is also planned to introduce the telephone number “112” for the integrated emergency service, which one can call even if it is not in the range of a cell phone or would normally require a certain amount of recharge.
The analysis of the CCUs’ registry data (Institute for Public Health - IPH, 2009) showed that almost two thirds of all patients with ACS reach a physician in primary care before admission to hospital. The facts are that ACS patients arrive in hospital by EMS (51.6%) and from PHC (12.9%), and that about 50% of sudden cardiac death in ACS occurs within the first four hours after symptom onset, and that two thirds of these events occur before reaching hospital. Thus, in the context of the pilot project “Implementation of protocol for pre-hospital diagnosis and treatment of ACS”, the EMS centre of Nis (south-east Serbia) has been founded by the MOH to be extended later throughout the country. Through this project, PHC physicians should be better informed about the importance of the “golden hour” and p-PCI advantages. Periodically, they should have compulsory meetings with the EMS teams to discuss practical matters as to how to improve the outcomes of their ACS patients and should be trained to be able to treat the ACS patient in the optimum way.
Changing the mentality of the population
The analysis of data from the Institute for Public Health (IPH) registry set on CCUs shows that 48% of patients reach hospital within six hours. Education of the population is the most efficient way to shorten the time from chest pain to calling the EMS. In particular, risk groups and members of their families are of high priority. Through the pilot project, they should be informed in detail about the nature of chest pain and about the importance of calling the EMS first. This education should be performed by TV and radio, and by way of brochures for patients distributed in the PHCs. Panel discussions funded by the local government and guided by EMS teams should also be organised with the enrolment of cardiologists from the referral p-PCI centre (CCU/IU). Through the campaign of the MOH, “Serbia for the healthy heart”, through media appearances and interviews given for the general population, cardiologists of Serbia started to synchronise education of the population about risk factors, recognition of chest pain and the importance of on-time admission to the hospital for a better outcome.
Changing organisation
In the Serbian health system there are many inherent organisational weaknesses, so it is not sufficiently adaptable to rapid changes and new challenges. There are enough health professionals, but their responsibilities are proportional to their salaries, which are not adequate. That is certainly not an excuse for someone’s “leisurely behaviour”, but that is simply the fact. The system is very much dependent on conscientious and responsible individuals determined to change such a system (these individuals have been the major players in SFL so far). Numerous instructions have been given and numerous rules have been applied, but strict organisation, which requires reward and disciplinary measures, is the only possibility in order to achieve better outcomes in this long-term comprehensive enterprise. For better organisation of EMS, there is an urgent need to provide more EMS teams to “jump in” and replace the team on duty transporting the patient to the p-PCI centre. A lot has been done for the provision of essential drugs to all EMS centres (aspirin, clopidogrel, heparins, tenecteplase, omeprazol), but the majority of EMS centres do not use these drugs in the pre-hospital management of STEMI patients. Fixed salaries demotivate staff for extra and new work. The remuneration of cathlab staff has proved effective and it should be applied as far as the actual economic situation allows.
Riding on the back of the enthusiasm of Serbia being incorporated into the SFL Initiative, significant results have been achieved in terms of the number of patients with STEMI treated by p-PCI (491 per million per year in the whole of Serbia, 711 per million per year in Belgrade). However, a lot of additional work on mentality and organisational changes is required to improve the quality of treatment, i.e., to increase substantially the number of patients treated within 120 minutes of FMC.
Experience in introducing p-PCI emanating from economically advanced countries is precious in this regard. It has been shown that mentality and organisational changes could be achieved by diligence and hard work in the long run. The mentality and organisational problems are almost the same in developed countries as in countries in transition, but the power to solve them is different6.
Conflict of interest statement
The authors have no conflicts of interest to declare.