![]()
Abstract
Serbia’s interventional community has been facing the multifaceted challenge of an ageing population with cardiovascular diseases as the primary cause of death nationwide, coronary artery disease (CAD) being the most prevalent subset. The following two fields of activity have marked the trajectory of progress in the field of interventional cardiology in Serbia: first, the expansion of the infrastructure, mainly through the opening of new catheterisation laboratories across all of the country’s administrative regions, which has resulted in better accessibility to coronary interventions for the general population; second, the creation of national platforms for continuous education, training and the promotion of clinical research in interventional cardiology, with close programmatic links to European Association of Percutaneous Cardiovascular Interventions (EAPCI)-based educational initiatives, including the curriculum for interventional cardiology. As growth seems to be inherent to the concept of progress, we report here on the expanding numbers of coronary interventions in the period between January 2010 and December 2015, and the early experiences with structural heart interventions in Serbia.
Demographics and organisation
As of 1 January 2015, the Republic of Serbia covers a territory of 88,499 km2 and has an estimated population of roughly seven million (n=7,114,393), according to the Statistical Office of the Republic of Serbia.
According to the report of the Institute of Public Health of Serbia for 2013, cardiovascular diseases were the second most cited reason for hospitalisations (n=154,145), after malignancies (n=172,851)1. Importantly, cardiovascular diseases have continuously been responsible for more than half of deaths in Serbia (53.7%, n=53,367 in 2013), and thus rank as the leading cause of mortality1. Within the scope of cardiovascular diseases, the two main mortality drivers were cerebrovascular diseases (24.7%) and ischaemic heart disease (18.5%). Furthermore, and of special importance for the domain of interventional cardiology, acute coronary syndromes (ACS) were responsible for 55.7% of deaths attributed to ischaemic heart disease. In absolute numbers, the population-based national ACS registry for 2012 recorded 20,981 patients with the diagnosis of ACS. The reported incidence of ACS in Serbia in 2012 was thus 291.4 per 100,000 inhabitants. In the same period, 5,817 persons died with an ACS diagnosis, which amounted to an ACS-related death rate of 80.8 per 100,000 inhabitants1.
ORGANISATION OF INTERVENTIONAL CENTRES
Considering the above-described high prevalence and impact on overall mortality of cardiovascular diseases in general and ischaemic heart disease in particular, the societal relevance of measures and initiatives aimed at decreasing the burden of cardiovascular diseases is vast, as is the consequent responsibility of the community of interventional cardiologists. In line with this, the network of PCI centres was gradually expanded during the period from 2010 to 2015. As of December 2015, 13 hospitals with PCI availability, with a total of 19 catheterisation laboratories, were operating in Serbia. On-site surgery is available in five of these hospitals. The combined number of independent operators is 89 and 22 are in training. All of the 13 currently operating PCI centres are offering primary PCI (pPCI), of which six are located in Belgrade, the capital and the biggest city in Serbia, with a population of 1,659,440. Of the six PCI centres in Belgrade, five were offering a 24h/7d primary PCI service as of 2015. With the opening of four new PCI centres at the level of regional hospitals between 2010 and 2014, the primary goal of delivering timely invasive treatment to all ACS patients has been actively pursued, as 95% of the population could now reach a PCI centre within a two-hour time window.
Health insurance contributions to the National Health Insurance Fund are compulsory for all citizens generating income. For persons not generating income and not insured as family members of those with income, contributions to the National Health Insurance Fund are made from the budget of the Republic of Serbia. Healthcare services are delivered within healthcare facilities recognised by the Health Facilities Network Plan, which applies to all 13 hospitals with PCI availability. Reimbursement policy is such that all interventional procedures which are indicated by a cardiologist are covered by the National Insurance Fund, for all insured citizens. Patients with acute coronary syndromes are admitted for emergent invasive treatment in all of the centres, irrespective of their insurance status.
CERTIFICATION AND ACCREDITATION
The current educational pathway consists of five years of internal medicine and one year of cardiology. Young interventionalists usually undergo basic training in the catheterisation laboratory during their internal medicine rotations and proceed with education in interventional cardiology in accordance with the local situation in their respective hospitals. Nevertheless, the interventionalist community in Serbia has recognised the need for a structured educational programme that will as a first step need to be certified by a professional organisation (i.e., the Working Group on Interventional Cardiology) and then eventually be accredited by the competent government authority. During the meeting of the Working Group on Interventional Cardiology in December 2015, an initial agreement was reached to adopt the EAPCI-endorsed curriculum for interventional cardiology subspecialty training in Europe2 as the foundation of the programme. In the next phase, potential educational centres and the appointment of programme directors would be discussed.
CONTINUOUS MEDICAL EDUCATION
In the light of the dynamic character of interventional cardiology, innovative approaches to education both for fellows in training and for more experienced interventionalists are mandated3. In Serbia, two annual educational platforms have been established in collaboration with the Working Group on Interventional Cardiology: BASICS (Belgrade Summit of Interventional Cardiologists) and SINERGY (Serbian Conference on Interventional Cardiology)3. Both meetings feature live cases of complex percutaneous interventions that are simultaneously discussed by the participants, while the 2016 edition of SINERGY introduced two novel session tracks: 1) an introductory course on complex PCI for young interventionalists with lectures by international faculty and case-based learning, and 2) panel discussion on specific regional challenges in everyday clinical practice (i.e., the prevalence of ACS which is higher than in the rest of Europe) with the participation of leading interventionalists from the region of Southeastern Europe.
CLINICAL RESEARCH
Due to its fast-paced innovative nature, clinical research may be considered an inseparable part of the practice of interventional cardiology. Regarding the structure of clinical research, interventionalists in Serbia have worked in two directions: first, towards an upgrade of the existing national ACS registry, which had previously been developed by the Institute of Public Health in collaboration with coronary care units across the country; second, aiming at nationwide clustering of research projects, as initiated at the SINERGY 2016 congress, by bringing together all relevant cardiovascular research groups from Serbia. The ultimate aim is to reach a consensus on the most important research areas (i.e., ACS and heart failure) and to facilitate cross-disciplinary collaboration between interventional cardiology and other branches of cardiovascular research, including basic science.
Coronary interventions
Initial agreement on the data collection process and permission to publish the collected data was obtained from all interventional centres in Serbia in March 2016. Data were centrally collected via a standardised electronic questionnaire that was filled out and sent in by a designated individual from each interventional centre. Any conflicting issues were resolved on an individual basis with each of the interventional cardiology department chairs.
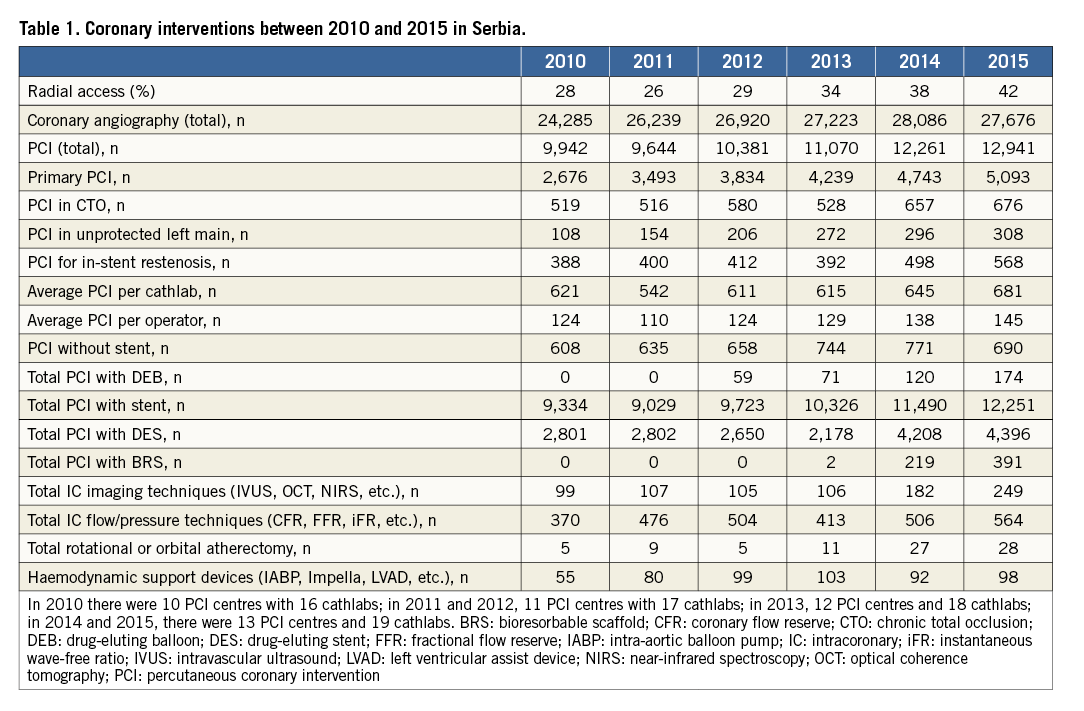
CORONARY INTERVENTIONS: THE GROWING TREND IN 2010-2015
In the time period from 2010 to 2015 there was a 30% increase in the combined annual number of percutaneous coronary interventions in Serbia (Table 1). This rising trend was not only attributed to the opening of new PCI centres, but also to an overall increased level of healthcare, with more patients being referred to non-invasive and invasive evaluation of ischaemic heart disease, as demonstrated by the concurrent 15% rise in the total number of coronary angiographies (Table 1). While the number of elective PCI increased only moderately (by 8% between 2010 and 2015), the number of pPCI for STEMI nearly doubled. This finding may be revealing of the focus of Serbia’s interventionalists in the past six years, namely to combat ACS as a highly prevalent, life-threatening disease. The number of complex interventions continued to increase from 2010 to 2015 in tertiary centres, including PCI of chronic total occlusions (CTO) and unprotected left main (LM), with the concurrent increase in the use of invasive imaging techniques (Table 1). The rate of intracoronary flow measurements as means of invasive ischaemia assessment is rising and amounted to 2% of all coronary procedures in the year 2015. Drug-eluting stent (DES) penetration has remained stable at around 30% throughout the studied time period (28% in 2010 and 33% in 2015). The DES penetration rate is predicted to increase to 50% in 2016. The use of drug-eluting balloons (DEB) has been scarce and mostly restricted to cases of in-stent restenosis (ISR) and small-vessel disease. Bioresorbable scaffolds have been in use since 2013. Among haemodynamic support devices, the intra-aortic balloon pump (IABP) has been used the most, albeit in a considerably small number of cases (0.5% to 0.7% of total PCI). Rotational atherectomy is mostly used in two tertiary hospitals in Belgrade, which utilise this technique in up to 1% of the total PCI. Finally, the gradual expansion of the transradial approach, from 28% in 2010 to 42% in 2015 (Table 1), has coincided with mounting evidence in favour of radial over femoral access, particularly in patients with ACS.
STENT FOR LIFE INITIATIVE
The management of patients with ACS has been one of the top national healthcare priorities due to ACS being the major cause of death. In order to facilitate implementation of the guideline-supported ACS management at a national level, the Cardiology Society of Serbia officially joined the Stent for Life Initiative at the European Society of Cardiology (ESC) Congress in Barcelona, on 31 August 2009. After joining the Stent for Life Initiative, the rate of pPCI increased 2.3-fold, from 311 per million inhabitants in 2009 to 717 per million inhabitants in 2015 (Figure 1). The predefined goal of 600 primary PCI per million inhabitants was reached in 2013. Concurrently with increasing the number of interventional procedures, efforts have been made to reduce time delays to intervention by actively involving the Emergency Medical Services (EMS). The predefined goals for the EMS have been to reach the patient within eight minutes after being contacted. According to the Belgrade EMS data from 2015, the average time from being contacted to reaching the patient was 12.4 minutes. Of all STEMI patients reaching a PCI centre in Belgrade in 2015, 28% were transferred by the EMS to the catheterisation laboratory, which, albeit an improvement from 7% prior to 2009, clearly still leaves room for further progress.
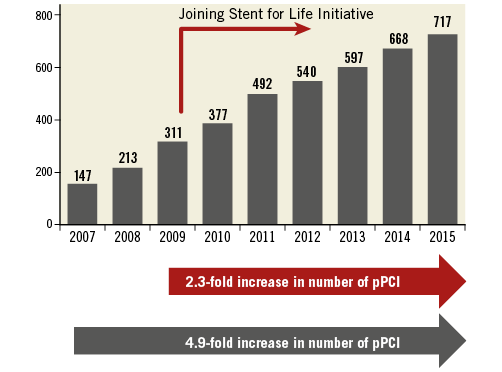
Figure 1. Stent for Life Initiative and progress in the treatment of patients with STEMI. Number of patients treated with pPCI per 1 million inhabitants in the years 2007 to 2015. After joining the Stent for Life Initiative in 2009, the rising trend continued, reaching the pre-set goal of 600 pPCI/1 million inhabitants in 2013.
BELGRADE STEMI NETWORK
After achieving the three main goals in the management of STEMI patients, i.e., i) increasing the number of primary PCI beyond 600/1 million inhabitants, ii) opening new regional PCI centres and thus allowing 95% of the population to reach a PCI centre within 120 minutes, and iii) decreasing the time delay to pPCI in close collaboration with the EMS, the next step could be the creation of regional networks for pPCI, which have already been successfully implemented in different countries throughout Europe and the world4.
The first STEMI network in Serbia is being launched in Belgrade (a pilot project with a starting date of 1 October 2016). It will be based on a rotational principle of six pPCI centres, similar to the Viennese model4. All six hospitals will treat STEMI patients during the on-hours (7:00 a.m. to 7:00 p.m.), while two centres per day will be responsible for the off-hours (7:00 p.m. to 7:00 a.m.). Thereby, the essential features of a successful STEMI network, such as a single telephone number, ambulances staffed with physicians and direct telephone access to the catheterisation laboratory, will be implemented4. Also, as insufficient case load is a known limitation in the pPCI domain, the rotational principle of the Belgrade STEMI network will provide a better balance regarding the pPCI rate among PCI centres in Belgrade, leading to a higher minimal pPCI rate per centre and thus an enhanced level of experience for individual interventionalists.
Structural heart interventions
While percutaneous closure of atrial septal defects (ASD) and patent foramen ovale (PFO) is performed more often, percutaneous valve interventions and left atrial appendage closure (LAAC) are only in the infancy of their development in Serbia (Table 2).
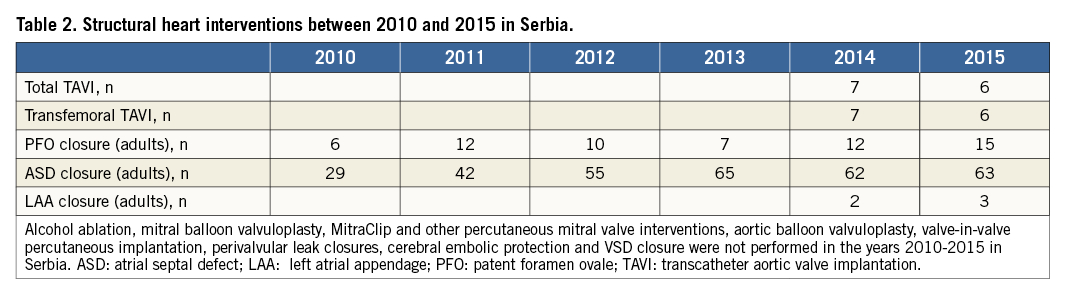
Our initial results with percutaneous implantation of self-expanding aortic valves in patients with symptomatic aortic stenosis with high surgical risk are promising5. The implantation technique appeared to be effective, safe and feasible with a very low complication rate5. Of course, TAVI, as treatment technique of choice in selected patients, needs to be extended with consistent application and performance, as this highly sophisticated procedure requires considerable experience and there is a learning curve. On the other hand, the prevalence of degenerative aortic stenosis is associated with advanced age and, as such, is expected to represent an increasingly important public health problem in our country. Thus, support from the national health authorities and national health funding system is essential in the wider application of this novel technique, as TAVI is a therapeutic option that has demonstrated improved survival and quality of life. The Valve for Life Initiative, similarly to the very successful Stent for Life Initiative, is important and is a promising way to increase awareness of valvular heart disease in the general population, to allow widespread access to transcatheter heart valve interventions, and to raise educational standards for healthcare professionals.
Conclusion
In order to meet the goal of reducing the burden of cardiovascular diseases in Serbia, the interventional community will have to act both efficiently by maximising the output of the available resources, and effectively by tackling the disease subsets with the greatest societal impact, such as ACS. The hitherto achieved growth in the number of coronary interventions generates new challenges and warrants new pathways of progress, particularly in the field of structural heart interventions, and new educational modalities for interventional cardiologists.
Acknowledgements
The authors would like to thank Professor Emeritus Miodrag Ostojic for his pioneering work in the field of interventional cardiology in Serbia, as well as Professor Zoran Perisic, Dr Gabrijela Stojkovic and Dr Goran Colakovic for their support in the nationwide data collection and also for their many valuable suggestions.
Conflict of interest statement
The authors have no conflicts of interest to declare.

