Abstract
The rate of percutaneous coronary intervention for acute ST-segment elevation myocardial infarction varies between European countries. The variations arise partly because of differences between countries in the primary percutaneous coronary intervention network system. The lack of an organised primary percutaneous coronary intervention network system in Turkey was the main reason for the low rate of primary percutaneous coronary intervention in Turkey. The Stent for Life project has increased the awareness of the importance of the prompt treatment of ST-segment elevation myocardial infarction in our country. Primary percutaneous coronary intervention has emerged as the preferred reperfusion strategy for patients with ST-segment elevation myocardial infarction in pilot cities after three years of Stent for Life project. In the present manuscript, we aim to summarise the current situation and the targets of the Stent for Life project in Turkey.
Introduction
Historically, access to the use of primary percutaneous coronary intervention (p-PCI) in acute ST-segment elevation myocardial infarction (STEMI) patients in Turkey has been low. In 2010, patient access to p-PCI was 8% in acute STEMI patients1. Thrombolysis was the dominant reperfusion strategy before the Stent for Life (SFL) project. Turkey has participated in the SFL project since 2009 initiating SFL in 18 pilot cities. Good progress has been achieved since that time. The number of p-PCI has increased significantly year after year. It has created a specific collaboration protocol between p-PCI centres, ambulances and emergency systems in the STEMI networks.
Current status of the SFL project
The SFL project was implemented in collaboration with our Ministry of Health and the Turkish Society of Cardiology. Successful collaboration has been achieved during the project and the Ministry of Health have supported the SFL project very strongly. The project targets were very clear. We have set up a network to reach those targets. The three main targets were: 1) to increase the use of p-PCI in more than 70% of all STEMI patients; 2) to achieve p-PCI rates of more than 600 per million inhabitants per year; and 3) that all existing p-PCI centres should offer a 24-hour p-PCI service seven days a week (24/7). Mortality from STEMI is lower in countries with p-PCI dominance than in countries where thrombolysis represents the treatment of choice2,3. We therefore aimed to reduce the mortality from STEMI through participating in the SFL project.
Cities were divided into three areas: the p-PCI area, a thrombolytic area covered by the cardiologist, and a thrombolytic area covered by the interventionalist (Figure 1). At the beginning of the SFL project, we established pilot cities and we set up a STEMI network. There was no consensus between emergency medical systems and first medical contact centres. No transport-chain protocol had been proposed previously by the Ministry of Health in Turkey. Patients being admitted to public hospitals were transported to non-PCI centres due to a lack of communication between first contact emergency medical systems and the hospitals. After the implementation of the SFL project in collaboration with our Ministry of Health, direct communication between emergency medical systems, ambulances and PCI centres prior to admission was achieved.
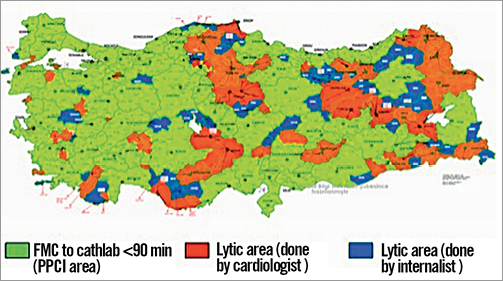
Figure 1. A primary percutaneous coronary intervention (p-PCI) colour map which was divided into three areas: p-PCI area, thrombolytic area covered by a cardiologist, thrombolytic area covered by an interventionalist.
In the pilot cities, after the SFL project started, the primary PCI rate reached over 90% in three years (Figure 2). In the last five years, the number of ambulances and emergency stations has been increased by the Ministry of Health, resulting in a marked increase in the number of cases reached by emergency medical systems and brought to hospital. The average time to arrival at the patient’s side was 12 minutes in the city area. In the pilot cities, the emergency medical system (ambulance) brings the STEMI patient directly to the p-PCI centre. The education of ambulance doctors and emergency doctors was started locally by experienced cardiologists. The percentage of STEMI patients arriving to the first hospital via ambulance services has increased from 20 to 77.33%1.
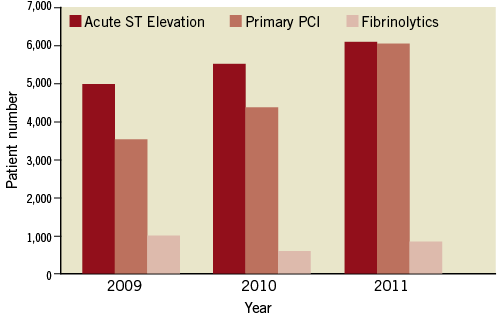
Figure 2. Primary percutaneous coronary intervention (p-PCI) in acute ST-segment elevation myocardial infarction.
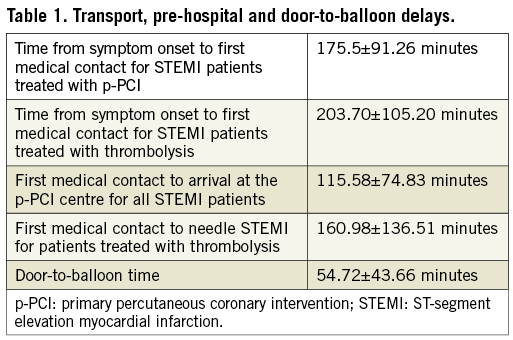
Time from the onset of symptoms to p-PCI seems to correlate directly with mortality rates4. Efficiency has also increased within hospitals with a mean door-to-balloon time for the pilot cities of 54.72±43.66 minutes (Table 1). Although door-to-balloon times have shortened progressively over the years, the time duration between onset of symptoms and transport of STEMI patients to PCI centres remains long. Consequently, it has been decided to increase awareness of the importance of the prompt treatment of STEMI. There has been no nationwide public campaign related to heart attack and p-PCI as yet, due to the incompleteness of p-PCI organisation in all regions of the country. However, local public campaigns have been started in two cities as part of the SFL project. Simulation courses for revascularisation techniques in acute STEMI have been organised for three years (one course per month) for young cardiologists. It has been reported that drug-eluting stents can safely be used in cases of STEMI5. However, bare metal stents were used in 87.3% of primary PCI cases and the use of drug-eluting stents was 8.11% in our country.
Barriers still to overcome
The main barriers to overcome in Turkey are that there are insufficient nurses and technicians for 24/7 PCI, especially in university hospital cathlabs, and an absence of additional payment to cardiologists for primary angioplasty. Therefore, only 57% of p-PCI centres can offer a 24-hour p-PCI service seven days per week. Time from symptom onset to first medical contact remains long due to lack of awareness of myocardial infarction.
Conclusion
Primary PCI has emerged as the preferred reperfusion strategy for patients with STEMI in pilot cities after three years of the SFL project. To date, no investigations into the medical transport chain and transport durations have been conducted nationwide. We have taken a snapshot of the country concerning STEMI management and we have also collected data regarding p-PCI rates and treatment strategies from the SFL project.
Conflict of interest statement
The authors have no conflicts of interest to declare.