The world’s biggest killer is ischaemic heart disease, which was responsible for 16% of the world’s total deaths in 2019. Non-ST-segment elevation acute coronary syndrome (NSTE-ACS) is a syndrome that encompasses unstable angina and non-ST-segment elevation myocardial infarction (MI). Patients in this heterogeneous population (Figure 1) account for the majority of ACS presentations, but management strategies for this group have remained a subject of debate for decades. In this issue of EuroIntervention, Eggers et al1 show that coronary angiography of NSTE-ACS patients performed within 24-72 hours (vs ≤24 hours) is not associated with worse outcomes (all-cause mortality, major adverse events), challenging current guideline recommendations.
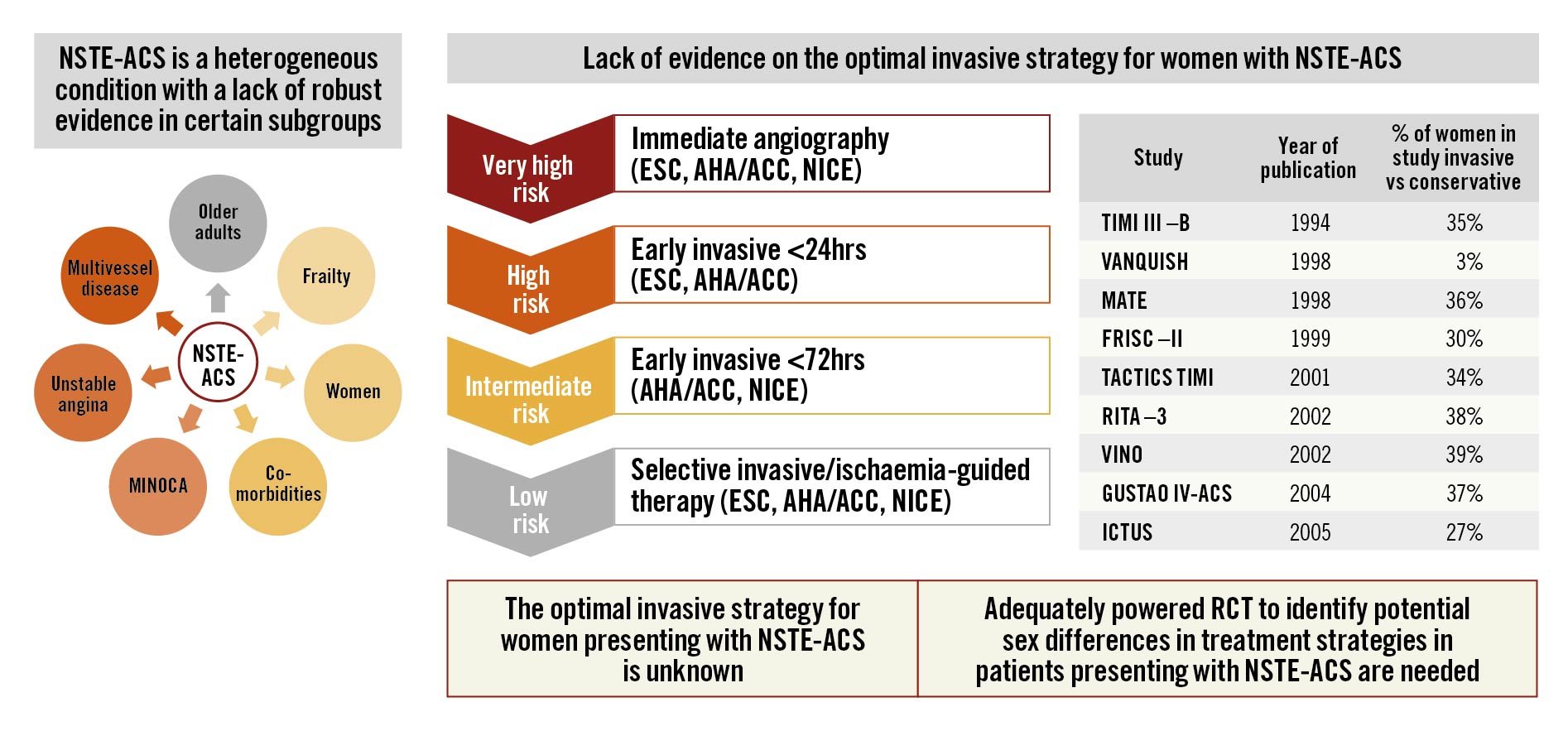
Figure 1. Challenges in the optimal care of patients with NSTE-ACS. AHA/ACC: American Heart Association/American College of Cardiology; ESC: European Society of Cardiology; MINOCA: myocardial infarction with non-obstructive coronary arteries; NICE: National Institute for Health and Care Excellence; NSTE-ACS: non-ST-segment elevation acute coronary syndrome; RCT: randomised controlled trials
Is there evidence for invasive coronary angiography within 24 hours?
The 2020 European Society of Cardiology (ESC) NSTE-ACS guidelines recommend using established risk scores, such as the Global Registry of Acute Coronary Events (GRACE) risk score, as part of the prognostic stratification. A GRACE risk score of >140 is one of the high-risk criteria with a recommendation for invasive coronary angiography within 24 hours. However, this strategy has not been possible to achieve in clinical practice given the challenges of logistics and resource implications for performing angiography within 24 hours and has been further hampered by the COVID-19 pandemic, which has caused major disruptions to cardiovascular care worldwide.
What is the evidence and feasibility behind the recommendation for invasive coronary angiography within 24 hours? The RIDDLE-NSTEMI study (n=2,147, 34% female, mean age 64 years) showed that an immediate invasive strategy was associated with a lower risk of death or MI2, predominantly due to reduced rates of new MI in the precatheterisation period2. In the TIMACS (n=3,031, 35% female, mean age 65 years) and VERDICT (n=2,147, 34% female, mean age 64 years) trials, the benefit associated with an early strategy was limited to the high-risk population (GRACE risk score >140)34. The VERDICT authors speculated that a high GRACE score was associated with high-risk angiographic features (such as left main disease, >70% stenosis of the proximal left anterior descending artery and/or 2- to 3-vessel disease involving the left anterior descending artery)5. These findings form the basis of international guideline recommendations to offer early invasive therapy for high-risk patients. However, in a recent meta-analysis, the early invasive strategy did not confer benefits in mortality or MI, but it did lead to a reduction in the length of stay (median reduction of 22 h, 95% confidence interval [CI]: 8 h-37 h; p=0.003) as well as recurrent ischaemia (relative risk 0.57, 95% CI: 0.40-0.81)6. The findings of the SWEDEHEART study seem consistent with the meta-analysis.
What about the underserved population?
It is important to note that the patient demographics of the trial participants differ from our contemporary patient population, with an underrepresentation of older adults and female patients in the context of an ageing population.
Older adults with NSTE-ACS
The mean age of patients in the SWEDEHEART study was 70 years. Given that the GRACE score is heavily age-weighted, older patients with NSTE-ACS are more likely to be classed as intermediate- or high-risk patients, and therefore invasive therapy would be recommended according to the guidelines. However, randomised controlled trials (RCT) investigating invasive and conservative approaches in older patients with NSTE-ACS have not provided definitive answers on the optimal treatment strategies due to recruitment problems and small sample sizes7.
Women with NSTE-ACS
MI with non-obstructive coronary artery disease (MINOCA) occurs more often in women than men. Many of the RCT evaluating treatment strategies for the management of NSTE-ACS are dated, and women constitute a small minority of participants (Figure 1). In the present SWEDEHEART study, only 31% were women1. Thus, the optimal care of NSTE-ACS in women is still unclear.
Moving forward, what does individualised care look like?
It was hoped that the RapidNSTEMI trial (NCT03707314) would provide some answers on the timing of an invasive strategy, but unfortunately the trial has been terminated early due to slow recruitment. SENIOR-RITA (NCT03052036), a large, multicentre RCT to determine whether a routine invasive approach is superior to conservative management in patients aged ≥75 years, will hopefully shed light on the efficacy of treatment strategies in this group. The requirement for “adequately powered RCT to identify potential sex differences in treatment strategies in patients presenting with NSTE-ACS” has been highlighted as representing a gap in the evidence in the 2020 ESC NSTE-ACS guidelines, emphasising the need for further research (Figure 1). While we await further research, the SWEDEHEART findings (albeit in the context of limitations associated with registry studies) might reassure clinicians that the inability to undertake angiography within 24 hours due to logistical and/or resource implications does not lead to adverse outcomes for patients.
Conclusions
The conundrum of the best care for patients with NSTE-ACS is ongoing. NSTE-ACS patients are a heterogeneous population who are at risk of adverse outcomes. Therefore, one size does not fit all for the optimal care of NSTE-ACS patients. There is a need for risk prediction scores which include diverse population demographics, higher-sensitivity troponin assays, and contemporary treatment options.
Conflict of interest statement
The author has no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.