Device description
Name and manufacturer: Nile CroCo stent and Nile PAX stent; Minvasys, Gennevilliers, France.
Approval status: CE mark Nile CroCo 2005, Nile PAX 2009.
Platform: Cobalt-chromium.
Strut thickness: 73 µm.
Coating: Nile CroCo: not coated. Nile PAX: polymer-free with paclitaxel coated on the abluminal surface in crystallised form. Drug concentration: 2.5 µg/mm2 with 100% of the drug released in 45 days.
Specific stent design: The Nile CroCo and Nile PAX stent platform comprises three different segments, a distal zone composed of six to eight cells depending on diameter, a median zone with eight to ten cells and a proximal zone with seven to nine cells to ensure the same metal:artery ratio along the entire length of the bifurcation, which also allows the proximal part of the stent to adapt to the proximal part of the artery during overdilation induced by kissing (Figure 1A).
Guiding: 6 Fr compatible.
Classification according to MADS: Provisional T-stenting in the “A” category.
Delivery system: The Nile CroCo and Nile PAX stents have the same delivery system which is based on two independent monorail balloon catheters, one for stent deployment in the main branch (MB) and the other for opening the stent towards the side branch (SB) enabling permanent guidewire access to the two branches. To aid positioning, three radiopaque markers are fitted on the MB balloon catheter, one at each end and one at the level of the bifurcation (Figure 1B). It also incorporates a peel-off sleeve which avoids the separation of the proximal shafts of the catheters.
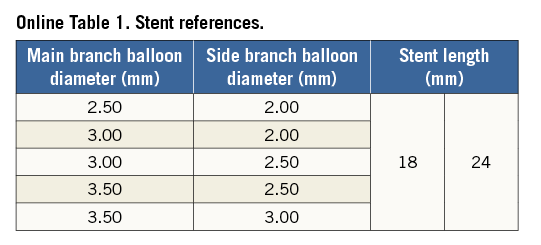
Stent sizes: Different variants exist with MB balloon diameter ranging from 2.5 to 3.5 mm and SB balloon diameter from 2.0 to 3.0 mm (Online Table 1).
Stent length: 18 mm and 24 mm.
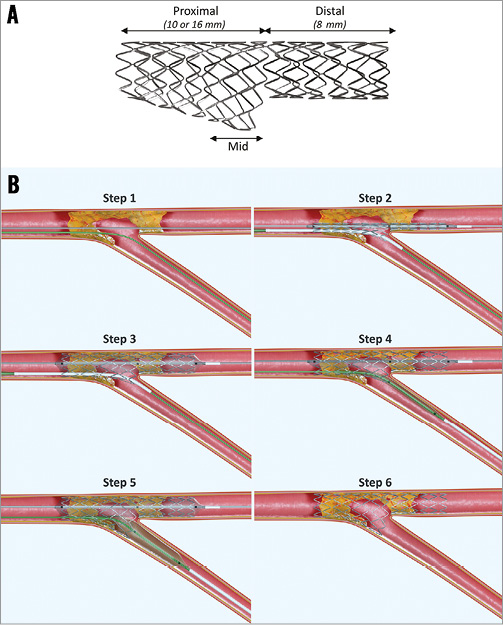
Figure 1. Stent design and procedural steps. A) Stent design. B) Procedural steps.
Procedural details1 (Figure 1B)
This system needs the positioning of two guidewires, one in the MB and one in the SB with systematic predilatation of the MB. Predilatation of the SB is recommended if the lesion appears to be significant. After selecting the stent size according to the distal diameters of the main and side branches, the system is inserted on the two guidewires, the stent-carrying balloon on the guidewire to the MB, and the SB balloon on the guidewire to the SB. The system is then advanced together until it crosses the stenosis and the central marker is at the level of the carina of the bifurcation. The system stops at the carina, at which point the operator will feel resistance.
Twisting of wires can occur in around 40% of cases, which can be easily solved by retrieving the system in the guiding catheter and re-piloting the SB or alternatively the MB guidewire.
Once the stent is positioned, the MB balloon is inflated and the stent implanted in the MB. The SB balloon is advanced so that it crosses the stent cells, which is achieved easily as the SB guidewire is already there. It is then positioned at the SB ostium. A kissing inflation is then recommended. Overextension of the proximal segment of the bifurcation is avoided thanks to the special SB balloon shape. The delivery system is then removed, leaving the two guidewires in place. If necessary, an additional stent can be implanted very easily due to the opening of the stent in the SB.
Clinical data
Experience with this stent has essentially been reported in two publications, the first with the Nile CroCo2 and a second with the Nile PAX paclitaxel version3.
In the first publication2, Bruno Garcia Del Blanco reported the results of a series of 151 patients treated successively at Val Hebron Hospital, Barcelona. Sixty percent of patients had a Medina class 1,1,1 bifurcation, with 73% of patients having a significant lesion at the ostium of the SB. The radial approach was used in 75% of procedures, using a 6 Fr approach catheter in 82% of cases. Guidewire crossing requiring repositioning was noted in 33% of cases. A kissing inflation with the system was performed in 95% of cases. An additional stent was used in the MB in 19% of cases, and in the SB in 10% of cases. Complete success with positioning of the Nile stent in the MB was achieved in 99% of cases, and the result in the SB was optimal in 90% of cases without additional stents. Among 138 patients with a complete follow-up at six months, the MACE rate was 14% and the rate of revascularisation was 7.2% despite the patient profile being relatively severe, including 55 patients with myocardial infarction <24 hours.
In the second publication3, procedural and 30-day follow-up data of the paclitaxel-eluting version (Nile PAX) were presented from a non-randomised international (Europe and Brazil) multicentre prospective study. Among 101 patients enrolled, 29% were diabetic, and in 80% of cases the LAD-diagonal branch bifurcation was the target lesion with 62% also having an SB lesion. In total, 102 lesions were treated, of which 62% had a stenosis on each of the main or side branches. Procedural success was achieved in 97% of cases. An additional stent was implanted in the SB in 25% of cases. Longer-term (nine-month) clinical follow-up data of this study were presented at EuroPCR 2011 (B. Garcia). The rate of restenosis was 13.9% in the MB, 12.8% in the SB and a total of 18.6% in the bifurcation, which led to a revascularisation rate of 12.6% with a single myocardial infarction during the follow-up period.
Ongoing studies
The 12.8% rate of SB restenosis found in the Nile PAX trial3 has prompted a recent study linking implantation of this stent with the systematic use of a paclitaxel-eluting balloon (Danubio; Minvasys) in the SB at the end of the procedure after kissing inflation. The study was presented at EBC Bordeaux 2014 (J. Berland), and the results are about to be published. Fifty patients from eight French centres were enrolled with systematic centrally analysed angiographic follow-up at six months. The primary endpoint of the study was late lumen loss (LLL) at the ostium of the SB which was slightly negative (–0.04±0.33 mm) at six months. Consequently, the rate of restenosis in the SB was only 2%.
Unique features
This is currently the only dedicated stent commercially available in Europe designed for permanent access of guidewires to the two branches of a bifurcation, facilitating easy performance of the provisional T-stenting technique and additional use of a drug-eluting balloon or stent to treat the SB. These qualities make it a very useful tool for the dilatation of distal stenosis of the left main trunk, as confirmed in the presentation at EuroPCR 2012 of a series involving 38 patients from four international institutions (J. Berland).
Potential improvements
A sirolimus-eluting version of the stent with a biodegradable polymer matrix is currently under development (Nile SIR). This coating technology will also be incorporated in the upcoming version of the stent dedicated to the treatment of the distal left main coronary artery (Nile LM SIR).
Conflict of interest statement
J. Berland reports having received lecture honoraria and consulting fees from Minvasys.
Online data supplement
Online Table 1. Stent references.
Moving image 1. OCT final assessment: posterior descending artery (PDA) to distal right coronary pullback.
Moving image 2. OCT final assessment: right postero-lateral artery (R-PLA) to distal right coronary artery (RCA) pullback.
Moving image 3. Coronary angiogram pre-intervention left anterior oblique (LAO) projection.
Moving image 4. Coronary angiogram pre-intervention LAO caudal projection.
Moving image 5. Coronary angiogram pre-intervention right anterior oblique (RAO) 125° projection.
Moving image 6. Ostial PDA balloon predilatation.
Moving image 7. Ostial R-PLA balloon predilatation.
Moving image 8. Angiographic control post balloon.
Moving image 9. Placement of the Nile PAX stent LAO projection.
Moving image 10. Angiographic control after placement of the Nile PAX stent.
Moving image 11. Main branch stent inflation.
Moving image 12. Side branch balloon advancement.
Moving image 13. Side branch balloon positioning.
Moving image 14. Kissing balloon inflation.
Moving image 15. Post-kissing angiography.
Moving image 16. Final angiogram 125° RAO projection.