Abstract
Aims: Right ventricular dysfunction (RVdy) is negatively associated with survival after left heart valve surgery. It is unclear whether RVdy has the same impact in patients undergoing transcatheter aortic valve implantation (TAVI). We sought to evaluate the prognostic impact of different grades of RVdy on TAVI, with and without concomitant left ventricular dysfunction (LVdy), and the possible impact of TAVI on RVdy.
Methods and results: Among 870 consecutive patients with severe symptomatic aortic stenosis undergoing TAVI, 226 patients (26%) presented with a concomitant diagnosis of RVdy. Patients were divided into three groups, Group 1: normal RV systolic function, i.e., tricuspid annular plane systolic excursion (TAPSE) >16 mm (n=644, 74%); Group 2: mild-to-moderate RVdy, i.e., TAPSE 10-16 mm (n=180, 20.6%); Group 3: severe RVdy, i.e., TAPSE <10 mm (n=46, 5.2%). Patients in Groups 1 and 2 showed a similar overall mortality rate at one month (5% vs. 8%, OR 1.1 [0.7-1.55], p=0.2) and at one-year follow-up (15% vs. 19%, HR 1.5 [0.84-2.2], p=0.09), respectively. Compared to Groups 1 and 2, patients in Group 3 showed a significantly higher overall mortality at one month (22%, OR 3.3 [1.8-4.1], p<0.001, and OR 2.1 [1.7-3.1], p=0.02, respectively) as well as at one-year follow-up (45%, HR 2.6 [2.1-3.45], p<0.001, and HR 1.9 [1.5-2.7], p=0.02), respectively. Pulmonary hypertension >60 mmHg (HR 1.5 [1.1-2.2], p=0.03), AF (HR 1.6 [1.1-2.4], p=0.01), creatinine clearance <30 mL/min (HR 1.92 [1.3-2.5], p=0.003), LVEF <30% (HR 1.5 [1.1-2.9], p=0.03), severe RVdy (HR 2.9 [2.7-3.3], p=0.002), severe RV dilation (HR 1.7 [1.2-2.2], p=0.005) and severe biventricular dysfunction (HR 3.9 [2.7-4.1], p=0.002) were independent predictors of one-year mortality. Among survivors, the majority of patients in Groups 2 and 3 experienced a significant improvement in NYHA class.
Conclusions: Severe RVdy limits the expected benefit of TAVI. In current risk scores right heart failure is not considered. The present study advocates the evaluation of this strong predictor in a more complete pre-procedural work-up.
Abbreviations
AF: atrial fibrillation
COPD: chronic obstructive pulmonary disease
CRS: CoreValve Revalving System
LVEF: left ventricular ejection fraction
MI: myocardial infarction
RV: right ventricle
TAM: tricuspid annular motion
TAPSE: tricuspid annular plane systolic excursion
TAVI: transcatheter aortic valve implantation
Introduction
Transcatheter aortic valve implantation (TAVI) is an effective therapeutic option in patients with severe aortic stenosis deemed at high or prohibitive risk for conventional surgical aortic valve replacement1,2. Despite a large amount of literature concerning possible factors associated with or predictive of an adverse prognosis, the impact of coexisting right ventricular dysfunction (RVdy) on TAVI outcome, with or without concomitant left ventricular dysfunction (LVdy), is unclear. On the other hand, it is also uncertain whether the improved left heart haemodynamics after TAVI could exert a beneficial effect on RVdy.
We thus sought to evaluate, in a multicentre registry of high-risk patients undergoing TAVI, the prognostic impact of different grades of RVdy on TAVI, with and without concomitant LVdy, and the possible impact of TAVI on RVdy.
Methods
STUDY DESIGN AND PATIENT POPULATION
From January 2010 to April 2013, a total of 870 consecutive patients affected by severe aortic stenosis were treated with the third-generation 18 Fr CoreValve ReValving® System (CRS) device (Medtronic CoreValve LLC, Irvine, CA, USA). This registry was approved by the local ethics committees and all the data are fully available to the enrolling centres. All patients were evaluated for TAVI by the local “Heart Team” which included a clinical cardiologist, an interventional cardiologist, a cardiac surgeon and a cardiac anaesthesiologist. The evaluation of the “Heart Team” led to the indication for TAVI being approved after careful assessment of all the clinical/anatomical conditions determining a higher risk of mortality/morbidity after surgery. All patients scheduled for TAVI and who gave written consent for the procedure and registry were enrolled in the study. There were no exclusion criteria for inclusion in this registry. However, for the present study, patients with a failed aortic bioprosthesis were excluded from the analysis and evaluated in a different publication3. Patients with prior mitral valve surgery were also excluded from the current analysis. Enrolled patients were divided into three groups, Group 1: normal RV systolic function, i.e., tricuspid annular plane systolic excursion (TAPSE) >16 mm (n=644, 74%); Group 2: mild-to-moderate RVdy, i.e., TAPSE 10-16 mm (n=180, 20.6%); Group 3: severe RVdy, i.e., TAPSE <10 mm (n=46, 5.2%).
Follow-up was scheduled in all patients at one, six, 12 months and then yearly.
Patients were followed up by means of outpatient clinics and regular contact with general practitioners.
DEVICE AND PROCEDURE
The CoreValve prosthesis as well as the procedure have been described elsewhere4-6. After the procedure, most patients were managed in an intensive care unit or coronary care unit for at least a day, and a temporary PM was left in place for at least 48 hours. All patients received acetylsalicylic acid (at least 100 mg before the procedure and lifelong) as well as clopidogrel (300 mg bolus plus 75 mg daily for three to six months unless prolonged administration was required for previous coronary intervention with drug-eluting stents). During the intervention, unfractionated heparin was administered to achieve an activated clotting time of 200 to 250 seconds for the duration of the procedure.
In the case of significant concomitant coronary disease, percutaneous intervention was performed before TAVI.
DATA COLLECTION AND DEFINITIONS
Transthoracic echocardiography was performed before TAVI, within three days after TAVI, and at one, six and 12 months by a senior cardiologist. Right ventricular function by means of tricuspid annular motion (TAM) or tricuspid annular plane systolic excursion (TAPSE), and RV size were determined and categorised according to the American Society of Echocardiography, European Association of Echocardiography, and the Canadian Society of Echocardiography recommendations7. In particular, a severe RV dilation was defined as a basal diameter ≥5 cm and/or an end-diastolic area ≥30 cm2 7. Frailty was defined according to Winograd and colleagues8.
Severe pulmonary hypertension (SPH) was defined as a systolic pulmonary artery pressure >60 mmHg. One-year clinical follow-up, or a medical record reporting a fatality, was available in all patients, while echocardiographic follow-up was available in all patients who reached one-year follow-up. Endpoints were defined according to VARC-2 definitions9.
STATISTICAL ANALYSIS
Continuous variables with normal distribution are presented as mean+standard deviations and compared using ANOVA with Bonferroni corrections. Variables not following a normal distribution are presented as counts and percentages and were compared with a Mann-Whitney test for comparisons between groups. The cumulative incidences of clinical events at follow-up were assessed with the Kaplan-Meier method and log-rank test.
Variables included in the baseline characteristics and procedural tables were tested for association with one-year survival rates and included in the model if they were univariately significant at 0.25 to estimate the risk-adjusted hazard ratio (HR). A Cox regression model was used to estimate HRs and 95% confidence intervals (CIs) to compare groups for all-cause mortality; in this model RVdy was entered as a categorical variable (1=normal, 2=moderate, 3=severe), with normal RVdy as the reference. Other variables included were SPH, logistic EuroSCORE, STS score, previous MI, COPD, LVEF, previous stroke, AF, creatinine clearance <30 ml/min, tricuspid regurgitation severity, left atrial size, presence of diabetes, and previous coronary artery bypass graft. To assess the validity of the Cox proportional hazards model, a proportional assumptions hazard was checked graphically. To assess the validity of the logistic regression model, a Hosmer-Lemeshow test was performed. Spearman’s correlation analysis was used to assess the interoperator agreement with respect to echo parameters.
All probability values reported are two-sided, and a probability value <0.05 was considered to be significant. All data were processed using the Statistical Package for Social Sciences, Version 20 (IBM Corp., Armonk, NY, USA).
Results
Baseline and procedural features of the study population according to baseline RV function are shown in Table 1 and Table 2. Severe RVdy at the time of the procedure was present in 46 patients, i.e., 5.2% of the population. Patients with severe RVdy more frequently had a glomerular filtration rate <30 ml/min compared to patients with moderate and mild/none RVdy. They also had a higher mean logistic EuroSCORE as well as a higher incidence of clinically relevant frailty. A severe dilation of the RV was numerically but not statistically higher in patients with severe RVdy.
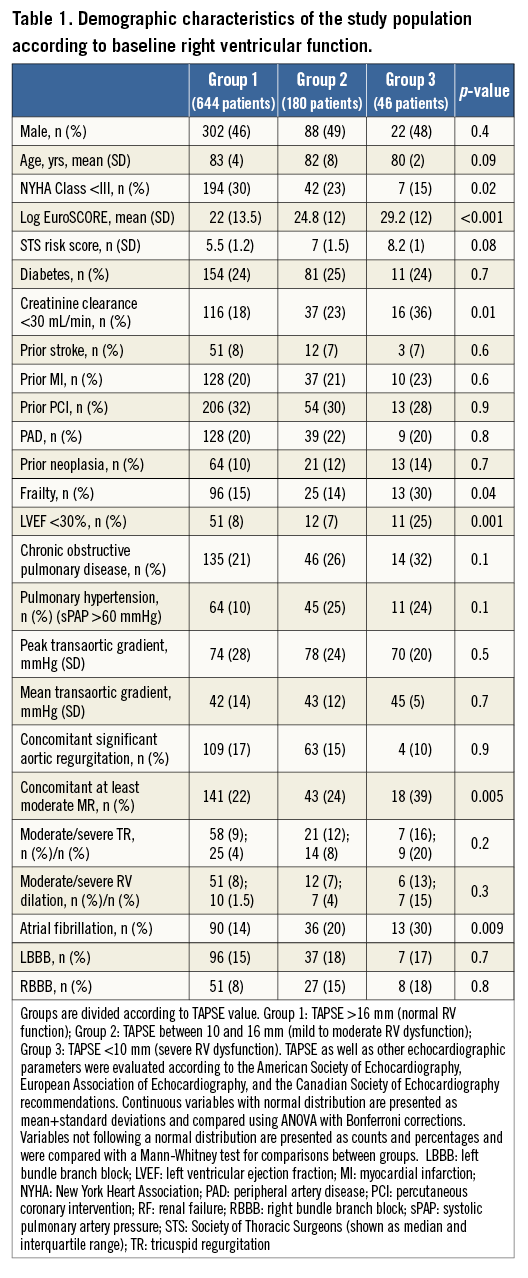
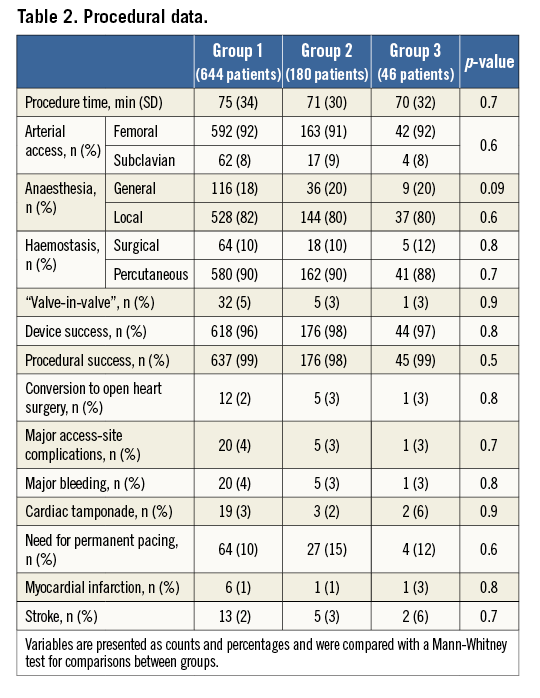
Atrial fibrillation (AF), concomitant moderate-severe mitral regurgitation, NYHA Class III-IV at presentation and the presence of severe LV dysfunction were significantly more frequent in patients with severe RVdy. No significant differences were observed across groups with regard to procedural data.
Analysis of mortality
OVERALL MORTALITY
At one month, patients with none or moderate RVdy showed similar overall mortality rates (5% vs. 8%, OR 1.1 [0.7-1.55], p=0.2). On the other hand, patients with severe RVdy had a significantly higher overall mortality (22%) compared to patients with none or moderate RVdy (OR 3.3 [1.8-4.1], p<0.001 and OR 2.1 [1.7-3.1], p=0.02, respectively) (Figure 1, Table 3).
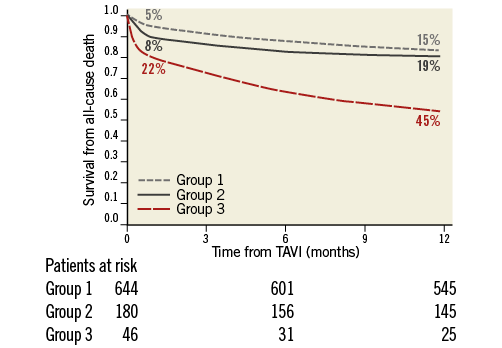
Figure 1. Kaplan-Meier analyses for one-month and one-year overall mortality.
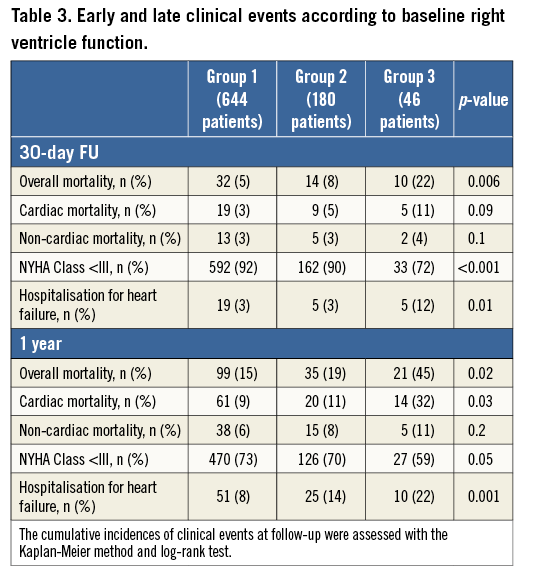
At one year, mortality rates were still similar between patients in Groups 1 and 2 (15% and 19%, HR 1.3 [0.77-1.98], p=0.4) and patients in Group 3 had a significantly higher overall mortality (45%, HR 2.6 [2.1-3.45], p<0.001, and HR 1.9 [1.5-2.7], p=0.02, respectively) (Figure 1, Table 3).
According to Cox regression analysis (with a model that included SPH, logistic EuroSCORE, STS score, previous MI, COPD, previous stroke, previous CABG, AF, creatinine clearance <30 ml/min, and at least moderate tricuspid regurgitation), SPH (HR 1.5 [1.1-2.2], p=0.03), AF (HR 1.6 [1.1-2.4], p=0.01), creatinine clearance <30 mL/min (HR 1.92, [1.3-2.5], p=0.003), LV ejection fraction <30% (HR 1.5 [1.1-2.9], p=0.03), severe RVdy (HR 2.9 [2.7-3.3], p=0.002), severe RV dilation (HR 1.7 [1.2-2.2], p=0.005) and biventricular dysfunction (HR 3.9 [2.7-4.1], p=0.002), were independent predictors of mortality at one year.
Patients with severe biventricular dysfunction (11 patients) (Table 1) experienced a very high rate of overall mortality at one year (eight fatalities, 72%).
CARDIAC MORTALITY
At one month, patients with none or moderate RVdy had a comparable cardiac mortality (3% and 5%, respectively, OR 1.2 [0.8-1.8], p=0.1). Compared to Groups 1 and 2, patients with a severe RVdy had a significantly higher cardiac mortality (11%, OR 2.5 [1.6-4.2], p=0.005, and OR 1.88 [1.2-3.1], p=0.04, respectively) (Figure 2, Table 3).
v 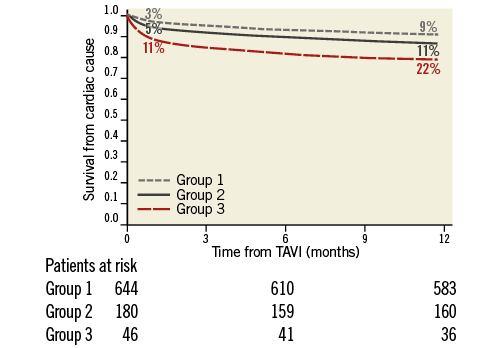
Figure 2. Kaplan-Meier analyses for one-month and one-year cardiac mortality
.
Consistently, patients with none or moderate RVdy showed similar cardiac mortality at one year (9% vs. 11%, HR 1.4 [0.7-2.1], p=0.8). Compared to Groups 1 and 2, patients with severe RVdy had a significantly higher cardiac mortality (32%, HR 2.2 [1.3-2.9], p=0.002, and HR 1.3 [1.1-2.2, p=0.02], respectively) (Figure 1, Table 3).
As mentioned above, patients with severe biventricular dysfunction experienced a high rate of overall mortality. Of note, six out of eight fatalities were “cardiac”, being related to an end-stage heart failure; the remaining two fatalities were the consequence of pneumonia.
NON-CARDIAC MORTALITY
Severe RVdy was not associated with a higher risk of non-cardiac mortality at one month or at one year (Table 3).
RATE OF HOSPITALISATION FOR HEART FAILURE AND NYHA FUNCTIONAL CLASS
At 30 days, the rate of hospitalisation for heart failure was significantly higher (12% vs. 3% and 3%, p<0.001), and the percentage of patients with NYHA Class
RIGHT VENTRICULAR DIMENSIONS AND FUNCTION AT ONE MONTH AND ONE YEAR AFTER TAVI
Among patients presenting with severe RVdy at baseline, a full recovery of the RV function has not been observed. In 12 patients (26%), the RV function improved to moderate at one month. From one month to one year, no further cases of improved RV function were observed. Possibly as a consequence of a low rate of events, the improvement in RV function did not independently predict mortality. Among patients with moderate RVdy, an improvement was more frequent (74 patients, 41%).
As for interoperator agreement, the highest value of concordance was achieved for RV dysfunction (Spearman’s correlation coefficient, 0.70-1.00), followed by RV dilation (0.58-0.9) and pulmonary pressure >55 mmHg (0.68-0.85).
Features of patients according to their initial RVdy grade and subsequent change are listed in Table 4. Notably, regardless of the severity of RVdy at baseline, patients with a significant improvement in RV function had a significantly lower rate of SPH, AF, and GFR <30 ml/min compared to patients in whom RV function was unchanged.
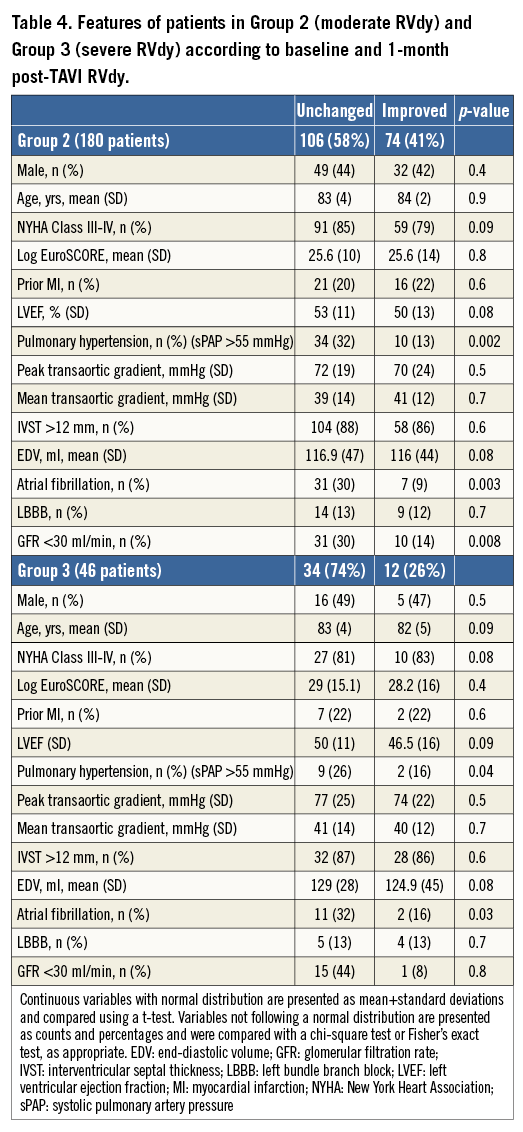
According to Cox regression analysis, the absence of SPH (HR 2.4 [2.1-3.1], p=0.02), the absence of AF (HR 2.01 [1.74-2.8], p=0.003), and of a GFR <30 ml/min (HR 2.3 [1.7-3.1], p=0.04) were independent predictors of an improvement in RVdy severity. The advent of percutaneous devices able to minimise the severity of tricuspid regurgitation may actually give a further option to improve the quality of life of these patients in whom the chances of impacting significantly on prognosis are scarce10.
Discussion
RVdy is independently associated with a reduced survival after left heart surgery11-13; however, data evaluating the prognostic impact in the field of TAVI are inconclusive. The present study, in patients referred to TAVI for symptomatic severe high-risk aortic stenosis, adds the following information to our current knowledge:
1. The presence of concomitant RVdy is relatively frequent in these patients.
2. Severe RVdy and severe RV dilation independently predict overall mortality.
3. Severe RVdy is a stronger predictor of one-year mortality as compared to severe LV dysfunction.
4. In patients with severe RVdy, an improvement in RV function can be expected in a minority of the patients.
5. To a greater extent, this improvement is more likely in the absence of AF, SPH, or severe renal failure.
6. The improvement in RV function seems not to be associated with improved survival.
The role of the right ventricle in the morbidity and mortality of patients presenting with cardiopulmonary disease is crucial although often underestimated. Indeed, the systematic assessment of right heart function is not routinely carried out, primarily because of the focus on the evaluation of the left heart, but also due to the paucity of large-scale studies providing normal reference values of right heart size and function. In addition, the most appropriate method to assess RV contractility is unclear14.
There are a number of different parameters to assess RV function, ranging from two- or three-dimensional volume and EF estimation to non-volumetric assessments. The former, however, are not recommended, considering the lack of standardised references as well as the gross approximation needed in terms of geometry14. The non-volumetric assessments, either global or regional, also have several limitations and rely on geometric assumption as well.
In the present study, we utilised TAPSE because it is the most extensively investigated and used in routine practice14. It measures the systolic excursion of the RV annular segment along its longitudinal plane, from a standard apical four-chamber window. TAPSE (or TAM) represents the longitudinal function of the right ventricle in the same way that mitral annular plane systolic excursion by Doppler tissue imaging does with the left ventricle. As with other regional methods, it assumes that the displacement of the basal and adjacent segments in the apical four-chamber view is representative of the function of the entire right ventricle, an assumption that is not valid in many disease states or when there are regional RV wall motion abnormalities13. Nevertheless, TAPSE strongly correlates with radionuclide angiography14 and has been validated against biplane Simpson’s ejection fractions and fractional area shortening15,16. Overall, more than 40 studies enrolling more than 2,000 patients have validated the clinical utility of TAPSE7.
The prognostic value of RV function has been investigated with cardiac magnetic resonance imaging (CMR) in patients with dilated cardiomyopathy, showing that an RV ejection fraction of <45% is significantly associated with adverse outcome17. To the best of our knowledge, our study is the first to underline on a nationwide level the importance of RVdy in high-risk patients undergoing TAVI, perhaps independently from the degree of tricuspid regurgitation that, similar to mitral regurgitation for the left ventricle, is a confounding factor when evaluating contractility. In a recent sub-analysis of the PARTNER II trial (inoperable cohort), Lindman and colleagues found that moderate or severe TR, and right heart enlargement, were independently associated with increased one-year mortality. However, the association between moderate or severe TR and an increased hazard of death was only found in those with minimal mitral regurgitation at baseline. In other words, moderate/severe TR was associated with a threefold higher hazard of death at one year in patients with minimal MR but not in those with concomitant moderate or severe MR. This actually challenges the “true” independency of TR as a predictor18. The interplay between mitral regurgitation, TR and RVdy has been investigated largely in the surgical setting: indeed, it has recently been shown in aortic stenosis patients that, after surgical aortic valve replacement, LV hypertrophy decreases, but the degree of diffuse interstitial myocardial fibrosis remains unchanged19. Diffuse myocardial fibrosis has been linked with diastolic dysfunction and elevated LV end-diastolic pressures, promoting post-capillary pulmonary hypertension20. The elevation of pulmonary pressure induces RV pressure overload, RV dilation and distortion, with subsequent “secondary” tricuspid regurgitation. Pulmonary hypertension, because of left heart stiffness associated with aortic stenosis and/or mitral regurgitation, may thus increase the severity of TR. This phenomenon has a clear pathophysiological implication, i.e., an increased pressure (pulmonary hypertension) and volume (TR) overload.
Surprisingly, Lindman and colleagues18 failed to find an independent association between RVdy and survival, although RVdy was associated with worse clinical outcomes. On the other hand, they found an independent association between severe RV dilation and mortality. There could be several explanations for these findings: the authors included a relatively small number of patients with RVdy (fewer than 50 patients), and the retrospective nature of the analysis may have been associated with incomplete echocardiographic assessment because the initial protocol of the PARTNER II trial did not focus on the influence of multivalvular disease.
In our cohort, severe RVdy and severe RV dilation were associated with an almost threefold higher and a more than twofold higher risk of one-year mortality, respectively. These two factors can actually be considered as two ways of looking at the same phenomenon, i.e., the failure of the right heart circulation negatively affecting the survival of patients treated for left heart disease.
Along with these two strong predictors, even SPH, although to a lesser extent, did independently predict mortality. This finding is consistent with that from the FRANCE-2 substudy21 but divergent with respect to the PARTNER II inoperable cohort in which it did not.
SPH clearly has a non-linear relationship with RVdy and dilation: along with pulmonary vascular bed tone, pulmonary pressure is determined by stroke volume and the antegrade flow from the RV. It is thus conceivable that the more the RV fails and dilates, the more its contractility will be reduced, and so will the contribution to pulmonary systolic pressures. This pathophysiological link is visible from the similar rates of SPH in patients with moderate or severe RVdy in our population (Table 1).
An improvement in RVdy severity did not exert a beneficial effect on survival. This positive effect could be attenuated by the stronger impact of other negative predictors. Indeed, there are known clinical features (renal failure, COPD, previous stroke, frailty), and procedural issues (paravalvular leaks, periprocedural stroke and bleeding events) that may exert such a strong negative impact on early and late outcomes that they overwhelm the role of an improved right heart haemodynamic1-6.
Of note, both severe renal impairment and frailty were significantly more frequent among patients with severe RVdy, and the absence of these clinical features, along with the absence of atrial fibrillation, predicted the improvement in RV function.
Severe RVdy seems to be a stronger predictor of one-year mortality than severe LV dysfunction (LVEF ≤30%). This result is unprecedented18,21-23.
Of note, currently used risk scores do not address right heart failure or function; the present study advocates the inclusion of this strong predictor in a more complete diagnostic work-up.
Finally, the present study shows that patients with severe biventricular dysfunction have an ominous prognosis: this condition was associated with an almost four times higher mortality rate as compared to the general population. It is obvious that the small sample size does not allow a definite conclusion. Nonetheless, such an end-stage setting truly challenges the indication for TAVI in terms of clinical equipoise. The advent of percutaneous devices aimed at reducing the severity of tricuspid regurgitation by modifying the valve geometry may provide a further tool to impact positively on the quality of life of these patients in whom the chances of ameliorating the prognosis are scarce10.
Limitations
As is obvious from the nature of a registry, the lack of any randomisation and differences in local “experience” could have added bias to our results. Although there was no central adjudication of events nor a central core lab, our data have been collected in a nationwide registry and extensively monitored. This database encompassed the first high-volume centres for TAVI in Italy, i.e., a homogeneous scenario of expertise where the effect of “the learning curve” is improbable or at least shared across centres. Evaluation of RV dysfunction, in particular in the presence of significant TR, can be misleading, in addition to the technical limitations of two-dimensional echocardiography used to assess the RV. Cardiac magnetic resonance (CMR) is currently the gold standard for the assessment of RV function. Unfortunately, systematic CMR exams were not carried out for clear logistic and economic reasons. Nonetheless, the use of TAPSE (or TAM) has been largely validated and is supported by both European and American Society of Echocardiography guidelines. Invasive haemodynamic data would have been of great interest; however, systematic right heart catheterisation was not performed.
Conclusions
Severe RVdy or a severe RV dilation independently predicts mortality in high operative risk patients undergoing TAVI for severe aortic stenosis. Severe RVdy is a stronger predictor than severe LV dysfunction. Although not associated with an improved survival, RVdy can improve after TAVI, in particular when moderate at baseline. Of note, while the expected benefit of TAVI in terms of mortality is limited, the benefits in terms of quality of life are substantial, even in this end-stage setting, and should be considered by the “Heart Team”. The presence of a biventricular dysfunction dramatically worsens the prognosis after TAVI.
| Impact on daily practice Severe RVdy or a severe RV dilation independently predicts mortality in patients undergoing TAVI. Although not associated with improved survival, RVdy can improve after TAVI. While the expected benefit in terms of mortality is limited, the benefits of TAVI in terms of quality of life are substantial, even in this end-stage setting. |
Conflict of interest statement
F. Bedogni and A.S. Petronio are TAVI medical proctors for Medtronic. A. Latib serves on a Medtronic advisory board. However, Medtronic had no role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The other authors have no conflicts of interest to declare.