Recently, in these pages, we have discussed issues surrounding peer review and the challenges associated with providing it as rapidly as possible1. Against this background, it is interesting to recall the history of the discovery of X-rays, which of course play a central part in the practice of contemporary interventional cardiology.
In his recent book on the story of radiation called “Strange Glow”, Timothy Jorgensen, a professor of radiation medicine at Georgetown University, retells some fascinating anecdotes on the history of ionising radiation2. None is more fascinating than the initial discovery of X-rays by Wilhelm Conrad Röntgen in Würzburg, Germany, in December 18953. Röntgen was experimenting with Crookes tubes (Figure 1), widely used at the time in physics laboratories, and consisting of a vacuum tube with electrodes at each end. When high voltage is supplied to the electrodes, electrons can overcome the absence of a transmission medium, and jump through the vacuum from the cathode to the anode. In doing so, they emit electromagnetic radiation. By coating the glass tubes with fluorescent material, brightly coloured illumination could be produced. This is the basis for neon lighting. What Röntgen observed was that, whenever he experimented with his Crookes tubes, there was a faint glow on fluorescent screens that were not in the vicinity of the device, and that this persisted even when the tube was completely blocked by other objects in his laboratory. As an avid photographer, he also happened to have photographic film in his laboratory and found that, after exposing it to what he called “X-rays” (because he didn’t know what these rays were), developing the film he could produce a permanent image, similar to what he had seen on the fluorescent screens. On 22 December 1895 he demonstrated his discovery to his wife, by taking an X-ray photograph of her hand (Figure 1), which startled and frightened her in equal measure. “I have seen my own death!”, she is reported to have exclaimed2.
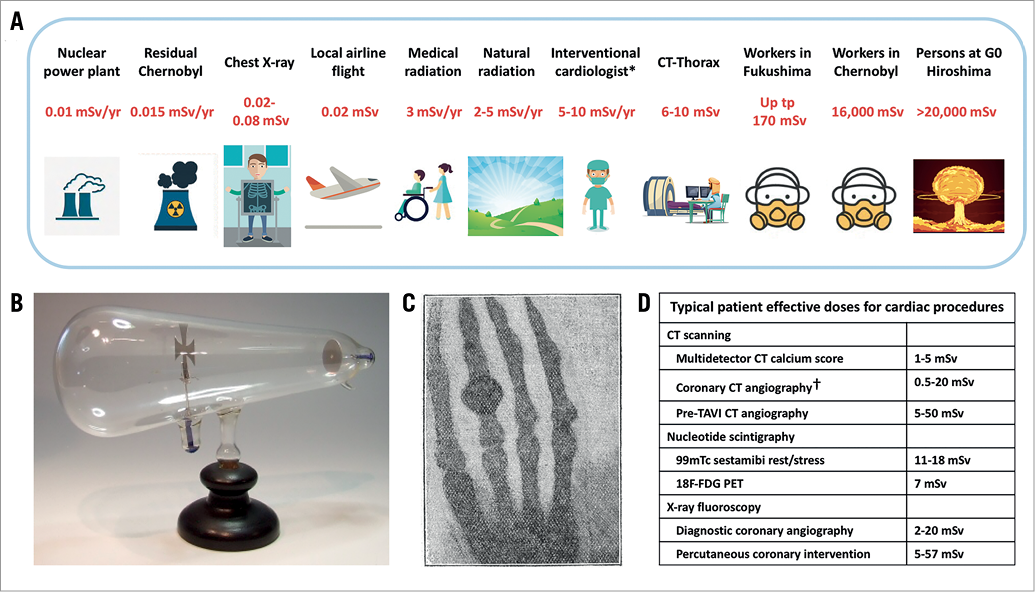
Figure 1. The discovery of X-rays and exposure to ionising radiation. A) Exposure of the general population, patients and occupational workers to ionising radiation. Values shown are cumulative per annum or per single exposure as indicated. B) Photograph of a Crookes tube. Reproduced with permission from https://www.crtsite.com. C) Photograph of the bones in the fingers of a living human hand; reproduced with permission from the report of Röntgen3. D) Estimates of the effective dose received by the patient during common cardiovascular examinations or procedures. Effective dosages based on data reported in the report of National Council on Radiation Protection and Measurements4,5,12. * = performing ca. 500 procedures/year; † = tube current modulation/prospectively triggered; G0 = ground zero
What happened next was almost equally as remarkable. Approaching the Würzburg Physical Medical Society, he had the manuscript of his observations successfully published on 28 December 1895. Moreover, a reprint with a photograph of the X-ray of his wife’s hand was presented as a poster at the Berlin Physical Society meeting on 4 January 1896. Other reprints were picked up by leading newspapers in London and New York over the following week. Within a few weeks, his experiments were replicated at many universities, including McGill University in Montreal. There, a doctor treating a man who had recently been shot in the leg heard about the discovery. Numerous explorative surgeries had failed to locate the bullet and amputation seemed imminent. However, after he had persuaded the professor of physics at the university to perform an X-ray exposure of the leg with his Crookes tube on 7 February 1896, the bullet was found and removed. Röntgen became internationally acclaimed and was awarded the first Nobel Prize in Physics in 1901. This surely represents the most remarkable feat of translation of scientific findings from bench to bedside.
The use of ionising radiation in clinical medicine is growing at a rapid rate. Cardiovascular medicine has been one of the fields to make greatest use of its benefits and it is estimated that cardiology accounts for about 40% of all non-radiation oncology patient exposure4, with X-ray fluoroscopy, CT scanning and nucleotide scintigraphy making the greatest contribution (Figure 1). As a consequence, however, exposure to medical X-rays now represents a significant proportion of a person’s annual radiation exposure (Figure 1), and the impact in terms of the risk of radiation-associated illnesses is not negligible4. As Jorgensen also notes, it is a sad truism of public health that the first indications of toxicity from a technology often come from workers who are occupationally exposed2. Two of the early examples in relation to ionising radiation were the miners of Schneeberg, Germany, and the wristwatch-face painters known as “the radium girls”. Many of the former died mysteriously from lung cancer, which later turned out to be due to exposure to radon gas. The latter applied radium to the faces of watches so that they could be read in the dark and had an unusually high rate of head and neck cancers. It later transpired to be due to radium ingestion caused by “tipping” the ends of their paintbrush in the corner of their lips, in order to keep the tip sharp. In a similar vein, reports soon began to emerge of medical X-ray workers who suffered from radiation-induced illnesses such as leukaemia and anaemia. This led to the publication of safety standards by the Röntgen Society as early as 1916.
In the intervening years, great progress has, of course, been made in both the application of ionising radiation for the diagnosis and treatment of disease, as well as the use of protective measures to limit the exposure of medical personnel involved in its use. Just a few weeks ago, the American College of Cardiology (ACC) in collaboration with four other professional societies produced a comprehensive up-to-date expert consensus document on the optimal use of ionising radiation and cardiovascular imaging5. This excellent document is essential reading for interventional cardiologists and contains eleven chapters focusing on basics such as what measures of radiation to use, how radiation can harm people, and which specific dose reduction strategies can minimise risk to patients and medical personnel.
It is nonetheless somewhat sobering to remember that the basis of the association between the dosage of ionising radiation received and the risk of subsequent disease derives from historical data from the exposure of victims of the first atomic bomb strikes in Hiroshima and Nagasaki in August 19452. Many inhabitants of both cities died in the early phase: the first wave succumbed within three days due to a combination of both trauma and acute radiation sickness (estimated exposure >20,000 mSv); the second wave died after a week or so due to severe gastrointestinal disturbance (estimated exposure 10,000-20,000 mSv); and the third wave died after about a month due to the effects of bone marrow failure (estimated exposure 1,000-10,000 mSv) (Figure 1). At doses below 1,000 mSv, the risk of developing radiation sickness falls off abruptly, and below 500 mSv radiation sickness is usually not seen. Those who survived the early phase represented an ideal population to study the long-term effects of radiation: a wide range of age and gender was represented, and, just like most New Yorkers know where they were when the first plane struck the World Trade Center, most knew exactly their location in relation to ground zero when the bomb struck. From this, their approximate exposure could be estimated. As a result of systematically following 120,000 of these survivors and documenting their subsequent rates of cancer, we now use the derived estimates to assess the risks of exposure to ionising radiation from medical procedures.
Interventional cardiologists are a group of workers who are among the most highly exposed to the risks of ionising radiation5. Measurement of operator exposure using current equipment and operator practices shows an exposure range of 0.2 to >100 uSv per procedure with average values of 8 to 10 uSv per case6. The ACC task force estimates that an interventionist performing 500 procedures per year may have a yearly exposure of up to 10 mSv5. The cumulative dose shown on the radiation monitoring badge at the time of EuroIntervention’s Editor-In-Chief’s retirement from the Thoraxcenter’s cath lab (1976-2012) was 1,012 mSv (personal communication, P.W. Serruys). The cumulative effects of this exposure vary from relatively benign to potentially life-threatening. At the more benign end of the spectrum, a report from the journal Heart some years back sticks out in my memory7. The report contains a photograph of three interventional cardiologists of various years of experience standing in a row with their trouser legs hitched up, revealing progressive loss of hair in the lower calf proportional to the years of exposure to duty in the cath lab. The presumed mechanism is radiation dermatitis induced by radiation scatter under the cath lab table.
At the other end of the spectrum, it is well known to readers of EuroIntervention that particular concerns exist in relation to a possible increase in the incidence of left-sided brain tumours8,9. We also recently published a paper describing modelling of the effects of radiation protection devices on the radiation dose received by the brains of interventional cardiologists10. Investigators noted that the use of ceiling-suspended screens, which are thankfully nowadays universal, was most successful in brain tissue dose reduction; however, this appeared to be particularly sensitive according to how the screen was used. In a typical PA projection, the dose reduction was 82% when the screen was close to the patient versus only 28% when a gap existed between the patient and the screen. Improvements delivered by the industry in terms of X-ray systems are also considerable, as was recently highlighted in a series of patients undergoing CTO intervention with various generations of X-ray system11. However, it is widely accepted that, in the community, knowledge gaps exist concerning the risks of ionising radiation and that we can do more to reduce radiation exposure to our patients and to ourselves.
Medical radiation is a powerful tool. Leveraging its advantages has provided the basis for modern diagnostic cardiology and the treatment of coronary and valvular heart disease in particular. Revisiting the story of the discovery of X-rays reminds us of what a remarkable feat of translational science this was for that or for any era. Remembering and learning from the fate of the atomic bomb survivors in Japan continues to inform our discussion about the risks associated with radiation use for patients and medical personnel. The publication of the ACC expert consensus document on ionising radiation provides a timely reminder to all of us in interventional cardiology of the importance of keeping up to date with best practices for the safe and effective use of radiation.