Abstract
Aims: Paediatric patients with mitral valve (MV) disease have limited options for prosthetic MV replacement. Based on long experience with the stented bovine jugular vein graft (Melody valve) in the right ventricular outflow tract, we aimed to test the use of the Melody valve as a surgical implant in the mitral position in a small group of infants with congenital mitral disease.
Methods and results: Eight patients, aged from 3 months to 6.2 years, with congenital MV dysplasia underwent Melody valve implantation in the mitral position between March 2014 and October 2015. Once sutured to the MV annulus, the Melody valve was expanded through a balloon catheter to achieve the best diameter (12-20 mm). Two patients needed ECMO assistance after traditional MV repair and a Melody valve was successfully implanted as possible bail-out. However, neither of them recovered from multi-organ failure and both died, in spite of the well-functioning Melody prosthesis. During follow-up, only one patient underwent catheter-based balloon expansion of the valve.
Conclusions: The medium-term results of this procedure are encouraging. The Melody valve opens up the opportunity to carry out MV replacement in more children at an earlier time point, and it has potential to revolutionise the treatment of MV disease.
Introduction
Congenital malformation of the mitral valve is a rare defect. Clinical and surgical management of this disease remains a therapeutic challenge in the wide spectrum of morphological abnormalities and there is a high risk of morbidity and mortality1-3. In the last decade, the development of new valve technologies has made the percutaneous replacement of dysfunctional valves possible4,5. The Melody® valve (Medtronic, Minneapolis, MN, USA) is a stent-mounted valved bovine jugular vein graft that is approved for transcatheter implantation into the right ventricular outflow tract position where it has been shown to restore pulmonary valve competence and relieve right ventricular outflow tract obstruction, even in young patients6. Based on this successful experience, in the last couple of years a novel use of the Melody valve in paediatric patients has been proposed. Following the preliminary results at Boston Children’s Hospital7,8, we tested the use of the Melody valve as a surgical implant in the mitral position in a small group of infants with severe mitral regurgitation and/or mitral stenosis who had undergone failing conservative valve repair.
Methods
The medical records of eight patients who underwent Melody valve implantation in the mitral valve position in our institution between March 2014 and January 2015 were reviewed. Clinical, echocardiographic, surgical, and follow-up data were collected. The techniques of valve modification and implantation have been reported previously by the pioneer surgeons at Boston Children’s Hospital8 and are summarised in Figure 1. Data were analysed using standard descriptive statistics.
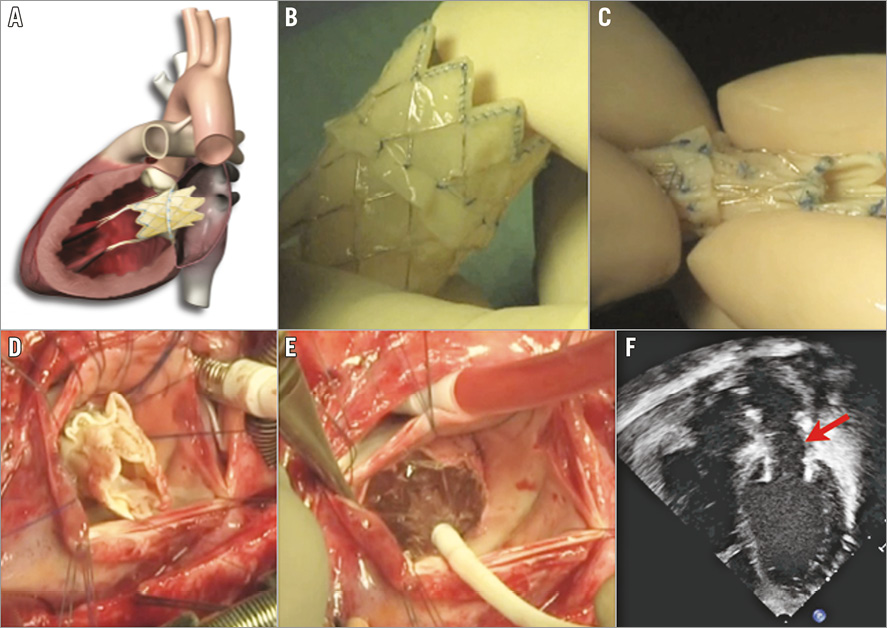
Figure 1. Steps of Melody valve implantation in the mitral position. A) Cartoon explaining the Melody valve in the mitral position. B) Preparation of the Melody valve. C) Downsizing of the Melody valve. D) Suture of the Melody valve in the mitral position. E) Balloon inflation. F) Post-procedural transoesophageal 2D echocardiography showing the stented Melody valve in the mitral position.
This study was performed in compliance with the Declaration of Helsinki. All parents received detailed instruction on the off-label use of the device and the potential risks of the procedure. Surgical and medical alternative options were carefully discussed before the parents signed the informed surgical consent form for the procedure.
Results
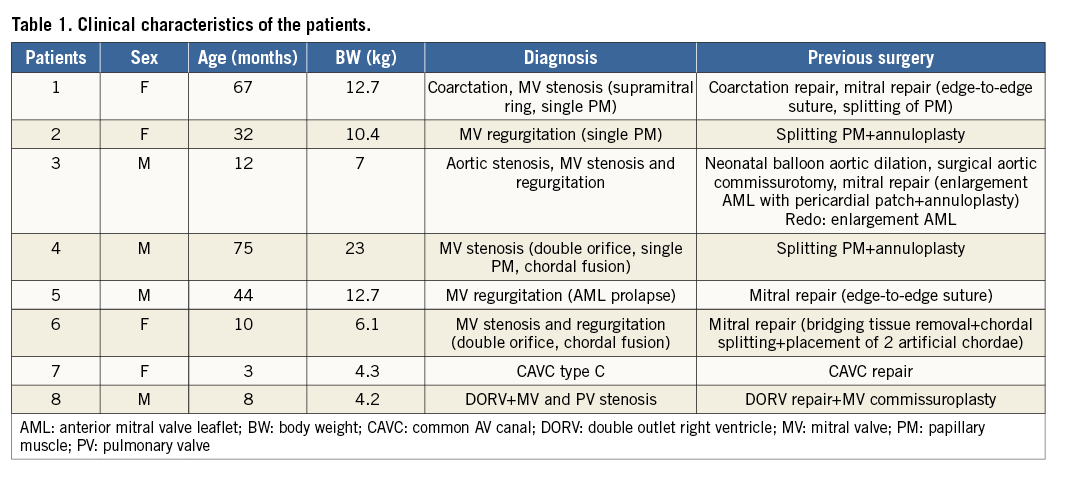
Table 1 outlines the clinical characteristics of the patients. Eight patients underwent successful surgical placement of a Melody valve in the mitral position. Median age at the time of the surgical procedure was 12 months (range 3-75 months), median weight 9.3 kg (range 4.2-23 kg). The lesions responsible for the mitral valve replacement were isolated congenital mitral valve dysplasia in four patients, Shone’s syndrome in two patients, double outlet right ventricle with mitral and pulmonary valve stenosis in one patient, and common atrioventricular canal type C in one patient. At baseline, mean diastolic inflow gradient was 13 mmHg (range 6-20 mmHg). Seven patients had moderate or worse mitral regurgitation.
All patients had undergone at least one previous surgical attempt to repair the dysfunctional mitral valve, and three patients (patients 1, 2 and 3) had two conservative surgical valve revisions before being referred for Melody valve implantation. Surgically, the native mitral valve was approached by opening the right atrium. The valve and mitral subvalvular apparatus were completely removed in all patients. In five patients, the Melody valve was modified before implantation by removing part of the distal crown of the stent to prevent systolic left ventricle outflow tract obstruction. Once sutured to the mitral annulus, the Melody valve was expanded through a balloon catheter to reach a suitable diameter according to the patient’s age and body surface area. The valves were dilated by a minimum of 12 mm in the smallest patients to a maximum of 20 mm in the oldest patient. In all cases, a single point of prolene was used to anchor the valve to the posterior wall of the left ventricle to prevent excessive device motion during the physiologic annular systolic motion. The atrial septum, removed to allow access to the mitral valve, was reconstructed with a pericardial patch and fenestrated with a 4 mm punch to allow future catheter access to the prosthesis. Median cardiopulmonary bypass time was 150 minutes (range 84-260 minutes). After surgery, all patients were anticoagulated first with heparin then with aspirin 5 mg/kg/day.
The median duration of hospitalisation was 19 days (range 17-42 days). Two patients died during hospitalisation. Both patients needed extracorporeal membrane oxygenation (ECMO) assistance for severe left heart failure and consistent high pulmonary venous pressure immediately after surgery. The Melody valve was successfully implanted a few days after the primary surgical procedure as possible bail-out in critically ill patients; however, neither of them recovered from multi-organ failure and both died in spite of a well-functioning mitral valve prosthesis.
At discharge, none of the six living patients had more than mild mitral valve insufficiency, and mean mitral diastolic inflow gradient decreased from a median value of 13 to 6 mmHg (range 4-14 mmHg). Four patients had paravalvular leaks that were not haemodynamically significant. In all but one case the leak resolved over time. After surgery, one patient with Shone’s syndrome and severe aortic valve stenosis presented residual obstruction of the left ventricle outflow tract related to a severely dysplastic aortic valve. In this patient, a mechanical obstruction of the left ventricular outflow tract due to the Melody valve’s structural stent was excluded based on transoesophageal and transthoracic echocardiographic evaluation. The patient was started on beta-blockers and, seven months after the procedure, underwent successful cardiac catheterisation to expand the Melody valve and a percutaneous aortic valvuloplasty to relieve aortic valve stenosis was performed (Figure 2).
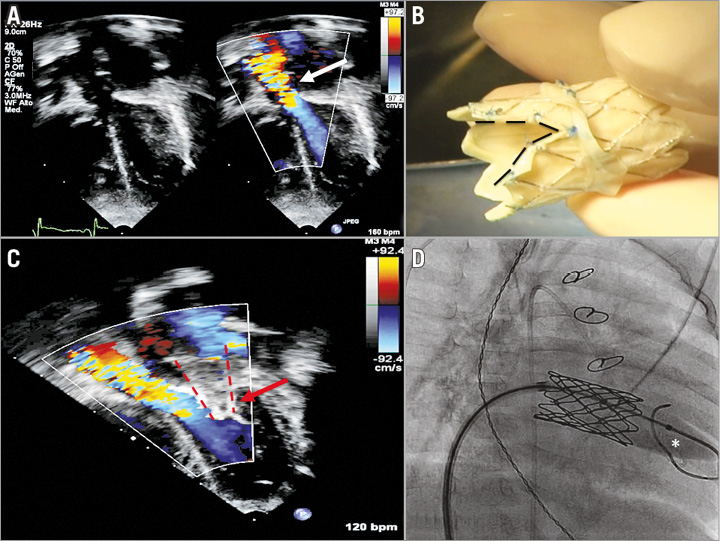
Figure 2. Images of patient #3, Shone’s syndrome. A) Pre-operative echocardiographic study (3 chambers projection) shows the narrow left ventricle outflow tract and aortic valve stenosis. B) To prevent further obstruction of the left ventricular outflow tract, the Melody valve was shortened before implantation by trimming the distal crown and making a deep V-shaped incision on the side facing the left ventricle outflow tract. C) Postoperative echocardiographic study (3 chambers projection) shows the Melody valve in the mitral position (red arrow) and the flow acceleration through the stenotic aortic valve; the flow acceleration starts above the left ventricular outflow tract at the level of the aortic valve and is not related to the Melody’s structural stent. D) Cardiac catheterisation was performed seven months after Melody valve implantation to expand the prosthesis.
At a median follow-up of 19 months (range 9-19 months), none of the six patients had been readmitted for heart failure. The majority of the valves demonstrated competent functioning by Doppler echocardiography and there were no complications such as stent fractures or the need for surgical reinterventions. As previously mentioned, only one patient underwent cardiac catheterisation. Another patient was admitted for arrhythmias that had been present since birth and were related to a left ventricle diverticulum that was not removed during surgery.
Discussion
The present case series confirms the feasibility, safety, and clinical efficacy of the surgical implantation of the Melody valve in the mitral position for the treatment of a congenitally dysfunctional mitral valve in paediatric patients. The results indicate that there is a high rate of procedural success and low procedural mortality and morbidity.
Despite the significant advances in the management and treatment of complex congenital heart defects, surgical repair of mitral valve dysfunction in children still carries a high mortality risk9,10. In our centre, the indications for surgical mitral valve repair are related to the mechanism of the stenosis and/or insufficiency, the integrity of the valvular apparatus, the age of the patient, and the Z-score of the left ventricle. Conservative surgery is preferred and feasible in most patients1,10-13; however, this is not always possible and in some cases mitral valve replacement is the only option. There are three major concerns associated with the use of valve prostheses in children. First of all, a fixed size prosthesis cannot follow the somatic growth of the patient. Thus, children who undergo mitral valve replacement at a younger age have a higher prevalence of reoperation14 to implant new, larger valves as they outgrow their replacements. Second, once implanted, fixed-diameter prostheses restrict the growth of the valve annulus, limiting the size of the valves that can be implanted in subsequent replacement operations2,15. Finally, two types of prosthesis can be implanted: bioprostheses, which are safer but prone to failure a few years after implantation, particularly in younger patients16; mechanical valves, which show better haemodynamic flow characteristics in small sizes, have a low profile with less potential for left ventricular outflow tract obstruction, and have longer durability17, but have an absolute requirement for anticoagulant treatment and in which bleeding or thromboembolic events are the main side effect. The international normalised ratio (INR) varies widely depending on health, medications, and diet, and it is even more sensitive to these factors in the paediatric population.
Conceived as a temporary device to replace failing pulmonary valves, the Melody valve has shown adequate performance even under high pressure such as in pulmonary hypertension18. In recent years, it has been used in a small cohort of teenagers and adult patients for the treatment of dysfunctional bioprosthetic mitral or tricuspid valves with promising results19. The valve stent dimensions range between 10 and 22 mm, and can be adapted to the patient’s anatomy. More importantly, when implanted at the smaller end of this range, it can be balloon-expanded during cardiac catheterisation as the child grows, potentially delaying further surgical procedures.
In our group of patients, Melody valve implantation reduced inflow obstruction and valve regurgitation in all, improving clinical symptoms. The procedure was well tolerated. The time of hospitalisation was within the range of hospitalisation days for mitral valve replacement surgery in our institution. All patients were discharged on antiplatelet therapy. The Melody valve permits avoidance of anticoagulants in children. In our population, we overlapped heparin and aspirin therapies for approximately five days after surgery until aspirin therapy became effective after which heparin was stopped and the patients were discharged on aspirin. No thromboembolic events occurred at medium-term follow-up. This is a unique advantage of the Melody valve. Paediatric patients receiving a prosthetic mitral valve require anticoagulation therapy and may face a significant risk of bleeding or thrombus formation in the immediate postoperative period due to an unpredictable drug dose response. These patients are generally not discharged from the hospital before meeting anticoagulation goals, but this often presents a clinical challenge and frequent blood tests. In the long term, anticoagulation therapeutic goals are dependent on patient illness, medication and food interactions, and altered oral intake. The anticoagulant nature of the drugs also means that it will be difficult for wounds to heal, such as the cuts and scrapes that children are apt to acquire in daily activity and, in case of trauma, there is a higher risk of severe complications.
Neonates and infants are obvious candidates for the Melody valve in the mitral position because appropriately sized mitral valve prostheses are often not available for small patients, while suitable alternatives are accessible for patients with a valve annulus larger than 18 mm. Two patients in our series had a mitral annulus larger than 18 mm and could have been good candidates for a valve prosthesis. However, we felt it was safer to implant the Melody valve. First of all, in order to overcome the problem of valve prosthesis replacement due to patient growth, the tendency in the operating room is to “oversize” the mitral valve prosthesis to delay a future mitral valve replacement. However, as the size/weight ratio increases, there is an increase in the early mortality associated with initial mitral valve replacement2. The Melody valve is safer as it does not need to be oversized because it can be expanded progressively, following the patient’s growth. The normal mitral valve annulus size in adult patients is between 30 and 35 mm; the Melody valve can expand up to 24 mm leading to a potentially long period free from surgical revisions, especially in younger children.
Based on the evolving understanding of the morbidity and mortality risks of mitral valve repair in babies and young children, along with the positive, although limited, experience with Melody valve implantation in the mitral position, it may be reasonably argued that Melody valve replacement of a dysfunctional mitral valve should be considered as a first surgical option in some, if not all, patients. This is particularly true for those patients with a challenging mitral valve anatomy which, on echocardiographic imaging or on surgical inspection, clearly has unfavourable characteristics for good surgical results. In fact, the use of the Melody valve as a second surgical option in case of severe haemodynamic and clinical deterioration may be useless. In our experience, the “delay” in two patients who after surgery had residual valve dysfunction and needed ECMO assistance led to a death, despite the “technical success” of the procedure (patients 6 and 8) (Table 1).
The most challenging problem in relation to implantation of the Melody valve in the mitral position in very young patients with a small left ventricle is that the device protrudes significantly into the left ventricle and may potentially result in obstruction of the left ventricular outflow tract. In five patients in the present series (patients 2, 3, 6, 7 and 8), we shortened the valve by trimming of the distal crown and making a deep V-shaped incision facing the left ventricle outflow tract (Figure 2B).
Conclusions
In paediatric patients with mitral valve disease every effort should be made to preserve the native valve by plastic reparative procedures. When valve replacement is necessary, the Melody valve should be considered a valid option.
The expandable Melody valve in the mitral position opens up the opportunity to carry out mitral valve replacement in more children and at an earlier age, and it has the potential to revolutionise care for infants and children with complex mitral valve disease. Moreover, additional advances in transcatheter valve technology techniques might allow non-operative replacement options.
Due to the rarity of the disease, further multicentre studies should be planned to define the clinical indications for the procedure, and the long-term outcome of the device under systemic pressure.
| Impact on daily practice The main gap in current knowledge is how to treat young patients with mitral valve dysfunction optimally. Our retrospective, observational study reviewed the safety and durability of the Melody valve inserted in the mitral position. If proven to be safe and durable, the expandable Melody valve in the mitral position opens up the opportunity to carry out mitral valve replacement in more children and at an earlier age, and has the potential to revolutionise care for infants and children with complex mitral valve disease. |
Conflict of interest statement
The authors have no conflicts of interest to declare.