The implantation of overlapping stents is a common technique in clinical practice for the treatment of long lesions or as a bail-out strategy in case of stent edge dissection or incomplete plaque coverage. The use of overlap is supported by evidence showing unacceptably high neointimal proliferation and restenosis rates when a gap is left between adjacent stents1.
However, during the bare metal stent (BMS) and the first drug-eluting stent (DES) era, overlap was reported to be a site of increased late lumen loss and was associated with a higher rate of target lesion revascularisation (TLR) and thrombosis compared with single layer stented segments2-4.
Imaging studies demonstrated that, although the overlap segments are generally associated with delayed healing and a thinner neointimal layer compared with non-overlap segments, in some cases the overlapped struts stimulate a thicker neointimal reaction5. These two opposite and apparently unpredictable healing patterns could favour, respectively, stent thrombosis or restenosis.
To try to understand the pathophysiological basis of the differential healing responses at the site of overlap, we should consider that it constitutes a peculiar microenvironment where the expansion of two stents might provide increased vessel wall injury and inflammation that could be related to the stent design, strut thickness, polymer biocompatibility and drug eluted6.
In addition, overlapping struts create complex haemodynamic disturbances that could influence the healing process. In particular, low wall shear stress has been identified as an important factor impacting on atherogenesis7, neointimal growth, in-stent restenosis and stent thrombosis8-10, and the vessel wall area in the overlapped segments is exposed to an overall lower shear stress compared to the adjacent areas covered by a single stent11.
More specifically, the struts of overlapping stents can be found in two different configurations, namely aligned one on top of the other or in alternating fashion. These two configurations are associated with two different shear stress patterns. The aligned configuration provides a larger obstacle to blood flow increasing recirculation zones with low shear stress11, while in the other scenario blood can flow between alternating struts with higher velocity magnitudes11.
The differential haemodynamics associated with differential overlapping patterns could be the basis for the heterogeneous effect of overlapping stents on neointimal growth.
The haemodynamic effect of overlap is therefore dependent on unpredictable factors such as overlapping strut configuration and predictable factors such as stent structural characteristics. This should be considered when implanting stents or bioresorbable scaffolds12.
The introduction of second-generation DES represents a remarkable advance in the field with novel stent design, reduced strut thickness, improved polymer biocompatibility, and novel drugs. These newer-generation DES have consistently been shown to be superior to the first generation in several large randomised trials. Recent studies evaluating the clinical outcomes after implantation of overlapping second-generation DES have reported comparable angiographic and clinical outcomes to non-overlapping DES, especially in terms of repeat revascularisation13,14. However, such investigations were performed predominantly in stable patients excluding thrombotic lesions.
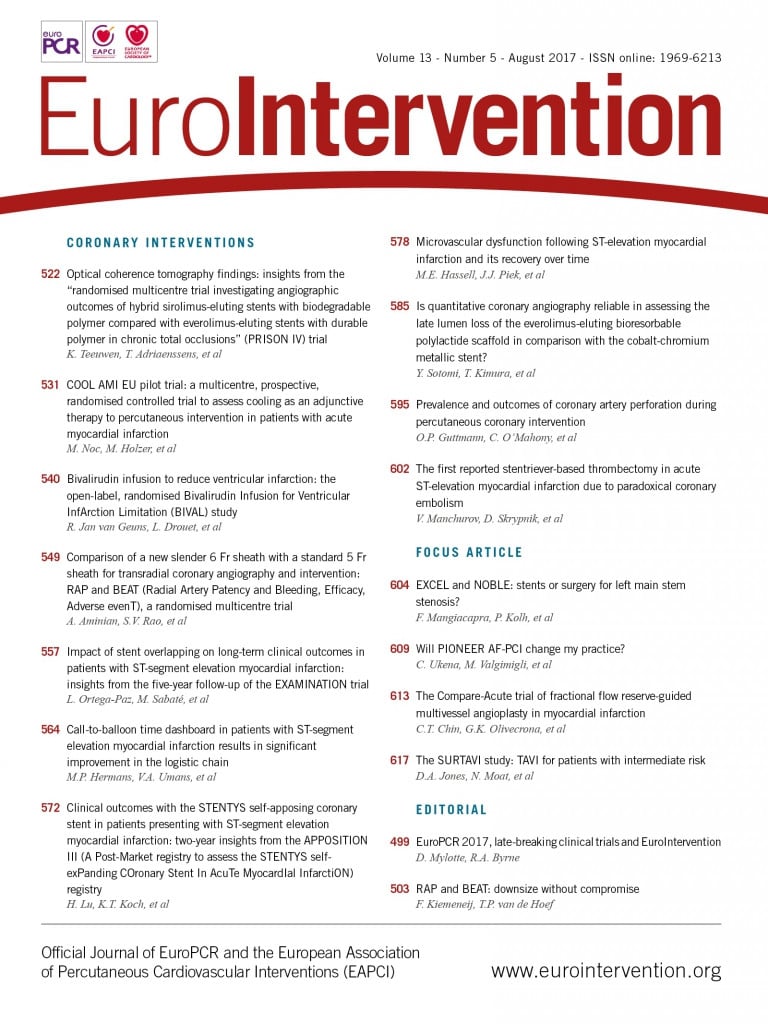
In this issue of EuroIntervention, Ortega-Paz et al15 report an evaluation of the impact of stent overlap on clinical outcomes after primary PCI as a sub-analysis of the EXAMINATION trial.
At five-year follow-up, the overlap group showed similar event rates compared with the non-overlap group. Patients receiving overlapping bare metal stents (BMS) had a trend towards a higher rate of the patient-oriented composite endpoint (PoCE) and device-oriented composite endpoint (DoCE) with a numerically increased occurrence of stent thrombosis. The authors should be congratulated for this investigation as it represents an evaluation of the effect of stent overlap in a specific patient subset, namely those with acute myocardial infarction, a group previously lacking in the literature. In this setting, a particular prothrombotic milieu is present, adding complexity to the overlap microenvironment. Such an acute condition could favour early thrombotic events after stent implantation. In addition, the vasoconstriction and the presence of thrombotic material could be associated with stent underexpansion and malapposition after thrombus resolution. This condition might prompt late thrombotic events especially at the overlapping site.
However, in the study of Ortega-Paz and colleagues, no major differences were observed in terms of clinical events between patients receiving overlap and non-overlap stenting, either at short or at long-term follow-up.
Although this is a post hoc analysis of a randomised trial and no formal power calculation was performed on this specific topic, the reported results are reassuring, especially when considering the second-generation DES group where everolimus-eluting stents (EES) were used.
It could be speculated that the stent design, the low strut thickness and the biological properties of the durable fluoropolymer of the EES, providing very low thrombogenicity and inflammatory cell attachment16, could minimise the differences between overlapping and non-overlapping segments. Such an effect was not present in the BMS group where a trend towards a higher rate of PoCE, DoCE and stent thrombosis was reported.
Translating this to clinical practice, the use of second-generation DES seems to abolish the disadvantages of overlapping stents, even in the acute settings where operators might be more reluctant to implant additional stents.
However, even though the present study is in line with previous reports on second-generation DES overlap, prospective studies evaluating this topic are still missing, and specifically designed investigations are necessary to evaluate fully the impact of second-generation DES overlap on clinical outcomes in both stable and unstable patients.
Conflict of interest statement
The authors have no conflicts of interest to declare.