Extraordinary claims require extraordinary evidence
Carl Sagan (1934-1996)
Iteration of second-generation drug-eluting stents (DES) utilising novel stent materials, designs and delivery systems, with enhanced biocompatible polymers or bioabsorbable polymers, and new antiproliferative agents, has significantly improved the outcomes of patients undergoing percutaneous coronary intervention compared with early-generation DES1. The availability of several new devices to treat coronary artery disease poses the question as to their relative safety and efficacy. In particular, establishing whether new DES with bioabsorbable polymers are superior, similar or inferior in terms of safety and efficacy compared with second-generation DES with permanent polymers remains an issue of paramount importance. Although several randomised trials have been performed to address this issue, they all had a non-inferiority design for the composite endpoint of death, myocardial infarction and target vessel revascularisation, had in general wide non-inferiority margins, and some of them enrolled low-risk patients2-4. In addition, several trials were based on unrealistic assumptions of non-inferiority, resulting in their being underpowered for their primary endpoint and with non-inferiority margins sometimes exceeding the observed event rates5. Considering that the outcome of patients with coronary artery disease in the last two decades has significantly improved due to enhanced pharmacotherapy and more aggressive invasive therapy, and that differences in clinical outcomes between current DES are relatively small, all studies performed so far have left undetermined whether there are significant differences in terms of safety and efficacy between these new devices.
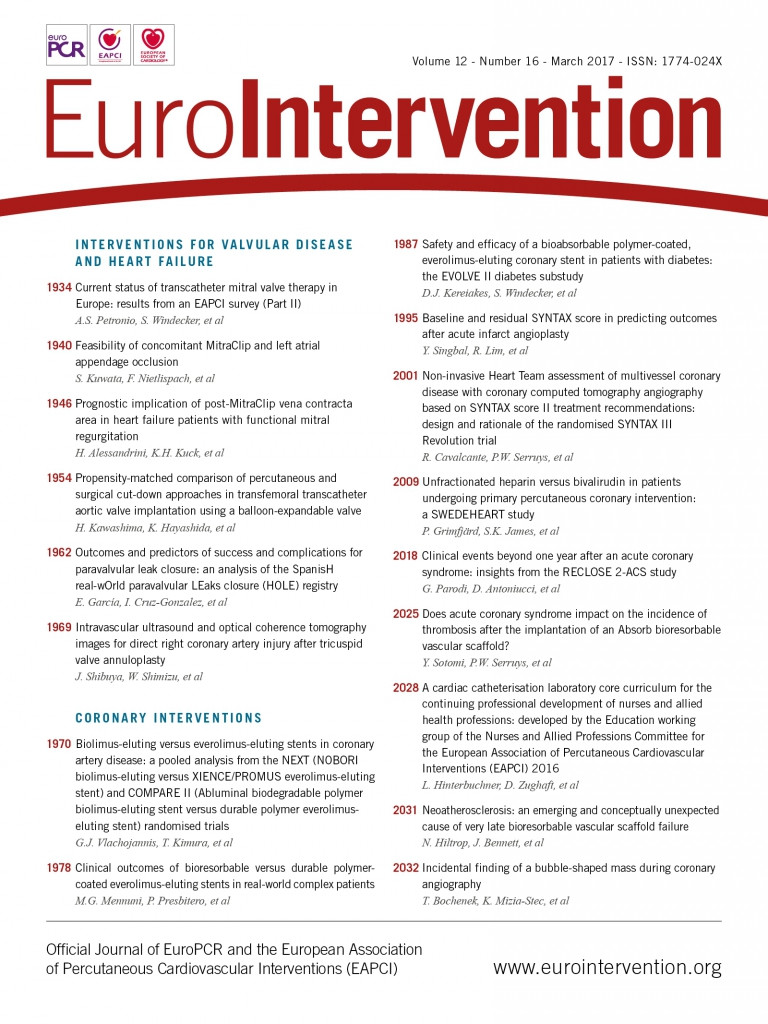
It is within this context that three novel investigations on new-generation DES are reported in the current issue of the journal, with a specific focus on the relative safety and efficacy of bioabsorbable polymer DES versus permanent polymer DES6-8.
The study by Vlachojannis et al6 is an individual patient-level meta-analysis of 5,942 patients with coronary artery disease pooled from two randomised trials, the NEXT trial and the COMPARE trial3,4, comparing the Nobori® (Terumo Corp., Tokyo, Japan) bioabsorbable polymer-based biolimus-eluting stent (BES) versus the XIENCE (Abbott Vascular, Santa Clara, CA, USA) permanent polymer-based cobalt-chromium everolimus-eluting stent (CoCr-EES). Both trials were characterised by low event rates which were almost half those expected, resulting in their being underpowered for their primary endpoint, and justifying the present analysis. In this pooled analysis, three-year rates of death or myocardial infarction (BES 7.8% versus CoCr-EES 6.7%, p=0.07), definite stent thrombosis (BES 0.8% versus CoCr-EES 0.4%, p=0.20), as well as target lesion revascularisation (BES 6.4% versus CoCr-EES 6.4%, p=0.78) were similar between the two groups. However, BES were associated with significantly higher rates of target vessel myocardial infarction compared with CoCr-EES (5.6% versus 4.5%, respectively, p=0.02). As significant imbalances in baseline patient characteristics were apparent after data pooling between subjects treated with BES versus those treated with CoCr-EES, a Cox multivariable analysis was performed, which basically confirmed the main findings of the study.
The study by Mennuni et al is a propensity score analysis of 253 matched pairs of patients with complex coronary artery disease treated with either the SYNERGY bioabsorbable polymer-based EES (Boston Scientific, Marlborough, MA, USA) or the XIENCE stent7. Complex coronary artery disease was defined as the presence of at least one of the following: recent acute myocardial infarction, left main disease, chronic total occlusion, coronary graft disease, in-stent restenosis, more than two vessels treated, and lesion length >34 mm. At one-year follow-up, there were no significant differences in the rates of the composite of all-cause death, myocardial infarction and target lesion revascularisation between the two stent types. The authors conclude that the SYNERGY stent with bioabsorbable polymer coating appears as safe and effective as the XIENCE stent with fluorinated permanent polymer coating.
Finally, the study by Kereiakes et al is a single-arm investigation without a randomisation comparator addressing the safety and efficacy of the SYNERGY stent in patients with diabetes mellitus8. In this study, two separate cohorts of patients were pooled: one was randomised to the SYNERGY stent in the EVOLVE II trial2 and the other was included in the non-randomised single-arm diabetes study following the completion of the EVOLVE II trial. Among the 466 patients included in the study, the 12-month target lesion failure rate was 7.5%, significantly lower than a pre-specified performance goal set at 14.5%. At two years, target lesion failure was 11.2% and definite/probable stent thrombosis was 1.1%, suggesting the safety and efficacy of the SYNERGY stent in diabetic patients.
Although these three studies add valuable information to the body of evidence about new-generation DES, the key question as to whether there are significant differences between bioabsorbable polymer DES versus second-generation permanent polymer DES still remains unanswered. Indeed, in the study by Vlachojannis et al, the permanent polymer-based CoCr-EES was associated with 50% lower rates of stent thrombosis and significantly lower rates of target vessel myocardial infarction compared to BES. These data are in line with a broader network meta-analysis including 51 randomised trials and 52,158 patients which showed significantly lower rates of stent thrombosis with CoCr-EES compared to BES after a median follow-up of 3.8 years9. However, a new generation of bioabsorbable polymer-based DES has been developed which have thinner stent struts, a faster kinetic of polymer absorption, and alternative drugs, such as the SYNERGY stent. In the EVOLVE II trial, similar results were apparent between the SYNERGY stent and the permanent polymer PROMUS™ EES (Boston Scientific) for the one and two-year composite endpoint of target lesion failure, including cardiac-related death, myocardial infarction related to the target vessel, and ischaemia-driven target lesion revascularisation2. However, EVOLVE II is again a non-inferiority trial enrolling only 1,684 patients with low-risk coronary artery disease. On the basis of current evidence, it therefore remains undetermined whether there are significant differences in safety and efficacy between bioabsorbable versus permanent polymer DES. Significant differences in mortality between newer-generation DES are unlikely, but on the other hand it is not possible to exclude differences in the risk of stent thrombosis or myocardial infarction. Assuming an event rate of 1% at one year and a 50% relative risk reduction, 13,000 patients would be needed to demonstrate a statistically significant difference in stent thrombosis between two stents with α=0.05 and β=0.90. Only a trial of that size, which is unlikely ever to be performed, would finally address the question as to whether there are significant differences in safety and efficacy between currently available DES.
Conflict of interest statement
T. Palmerini has received speaker fees and research grants from Abbott. G. Biondi Zoccai has consulted for Abbott Vascular.