Abstract
The role of coronary revascularisation with PCI and CABG in patients with stable and unstable coronary artery disease (CAD) is well established and there is a general consensus among guidelines as regards the indications for coronary revascularisation. Although revascularisation has undoubtedly revolutionised the treatment of CAD, it is vital to understand the recent advances and importance of the concomitant use of evidence-based optimal medical therapy (OMT). In contemporary practice, OMT should include an antiplatelet agent (or dual antiplatelet therapy when indicated) and a lipid-lowering drug for all patients, and a beta-blocker and an ACE inhibitor (or angiotensin receptor blocker) for the vast majority of patients, along with addressing cardiac risk factors and lifestyle management. OMT is the recommended initial choice for patients with stable angina pectoris, and the indication for revascularisation would be persistence of symptoms despite OMT and/or improvement of prognosis. For patients with acute coronary syndromes or those who underwent coronary revascularisation with either PCI or CABG, long-term use of OMT improves clinical outcomes and prognosis.
Introduction
Coronary artery disease (CAD) manifesting as chronic stable angina pectoris or acute coronary syndromes (ACS) remains the leading cause of morbidity and mortality globally. Significant and symptomatic CAD is often treated with percutaneous coronary intervention (PCI) or coronary artery bypass grafting (CABG) in contemporary practice. Whilst these mechanical revascularisation procedures have undoubtedly revolutionised the treatment of CAD, it is vital to understand the importance of the concomitant use of evidence-based optimal medical therapy (OMT) in these patients. This review paper examines the evolution of currently used OMT, its role in contemporary clinical practice and future directions.
Historical developments
With the advent of coronary revascularisation (CABG and PCI) and any subsequent advances in technique or technology, these procedures were compared with the standard medical therapy available at that time. These comparative studies, which helped to establish the safety and efficacy of the newer treatment modalities, also led to several fundamental misconceptions. Whilst the initial head-to-head studies did indeed compare interventional versus medical treatment, later studies comparing intervention plus medical treatment versus medical treatment alone were also perceived as comparisons between revascularisation and medical management. This perception may have contributed to slow/delayed uptake of OMT in patients undergoing revascularisation, despite the fact that studies showing superiority of the interventional modality actually showed superiority of intervention complemented by OMT at that time. Furthermore, it is prudent to highlight that OMT is an evolving entity. What constitutes OMT now was not that which was used in clinical trials a few decades ago. Those trials are unlikely to be repeated with current OMT, but it is important to understand the limitations of the data from the early trials. OMT has evolved along with coronary revascularisation1 (Figure 1).
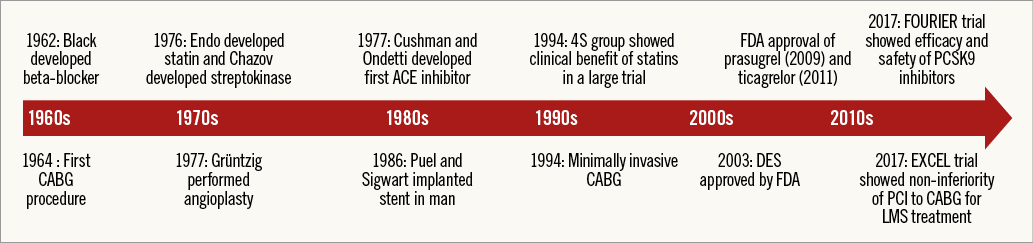
Figure 1. Historical developments in medical therapy and coronary revascularisation.
LIPID-LOWERING DRUGS
It was only in the 1960s that the Framingham study established hypercholesterolaemia as a risk factor for CAD. The discovery of any meaningful treatment for hyperlipidaemias took another few years. In 1976, Akira Endo discovered the lipid-lowering properties of statins2. In 1978, Alberts and Chen found a potent statin, lovastatin, which became the first statin available for clinical use in 1987. Simvastatin was initially approved for marketing in Sweden in 1988 and subsequently worldwide. In 1994, the 4S group showed clinical benefit of simvastatin in a large trial of patients with hypercholesterolaemia. More statins continued to appear in the clinical arena - pravastatin in 1991, fluvastatin in 1994, atorvastatin in 1997 and rosuvastatin in 20032. A potent new class of lipid-lowering drugs, PCSK9 inhibitors (discussed later), has only emerged recently and is currently the focus of intense investigation.
ANTIPLATELET AND THROMBOLYTIC DRUGS
Coronary thrombosis as the cause of acute myocardial infarction (MI) was described in the late 19th century; however, its management was limited to bedrest and supportive therapy for the first half of the 20th century3. In 1974, Elwood and colleagues reported the first randomised controlled trial (RCT) of aspirin in the secondary prevention of mortality from MI. In 1976, Chazov administered intracoronary streptokinase in the treatment of acute MI which led to the first large randomised trial, namely GISSI (Gruppo Italiano per lo Studio della Sopravvivenza nell’Infarto miocardico). In 1988, the Second International Study of Infarct Survival (ISIS-2) demonstrated that the addition of aspirin to thrombolysis further reduces mortality. First-generation P2Y12 inhibitors came into clinical practice in the 1990s. The CAPRIE (clopidogrel versus aspirin in patients at risk of ischaemic events) trial in 1996 established the benefit of clopidogrel over aspirin in atherothrombotic patients, by reducing the rate of recurrent MI. Potent newer oral P2Y12 inhibitors, prasugrel (FDA approval 2009) and ticagrelor (FDA approval 2011), have become available in clinical practice over the last decade. The intravenous P2Y12 inhibitor cangrelor received FDA approval in June 2015.
OTHER CARDIAC MEDICATIONS
In 1962, James Black developed the first beta-blocker, propranolol. A cardioselective beta-blocker, atenolol, was developed in 1976. In 1977, Cushman and Ondetti developed the first angiotensin-converting enzyme (ACE) inhibitor, captopril. In 1992, Pfeffer and colleagues in the SAVE (Survival and Ventricular Enlargement) trial showed that ACE inhibitors prevent ventricular remodelling and reduce mortality post MI. Angiotensin receptor blockers (ARB) were also developed in the 1990s.
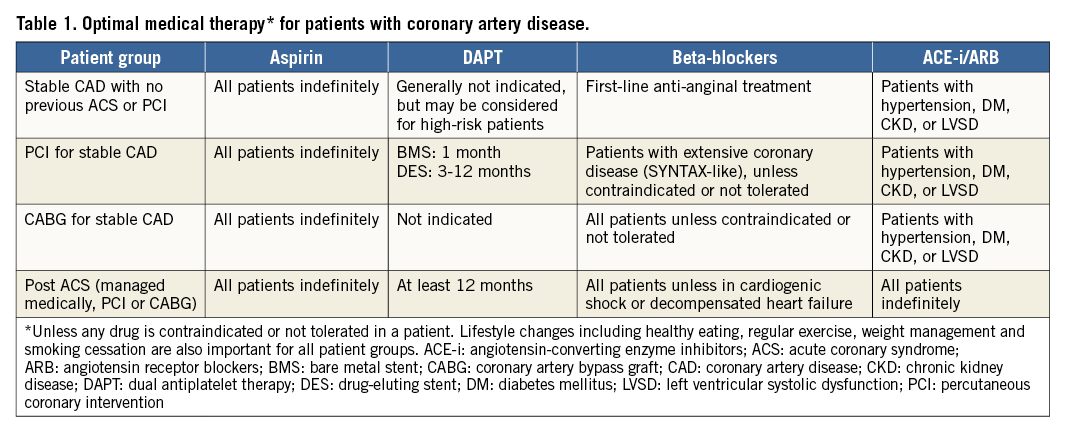
Defining OMT
As OMT has remained a moving target, defining what constitutes it remains challenging. An antiplatelet agent and a lipid-lowering drug are indicated for all patients, unless contraindicated or not tolerated. Dual antiplatelet therapy (DAPT) is recommended in post-ACS (usually 12 months) or post-PCI (three to 12 months) patients. However, DAPT can be considered for selected high-risk stable CAD patients or for a longer duration after an ACS. ACE inhibitors or ARB are recommended for all post-ACS patients and stable CAD patients with hypertension, diabetes mellitus, chronic kidney disease, or left ventricular systolic dysfunction. Beta-blockers are also indicated for all post-ACS patients but their use in stable CAD is debatable4. We advocate the use of a beta-blocker as first-line anti-anginal for symptomatic stable CAD or patients undergoing revascularisation for extensive CAD (i.e., SYNTAX-like patients)5 or post-CABG patients6. OMT should also include appropriate management of other cardiovascular risk factors with drugs and lifestyle interventions. Our recommendation of what should constitute OMT is shown in Table 1.
Current status of optimal medical therapy
OMT FOR STABLE CORONARY ARTERY DISEASE
OMT is the recommended initial choice for patients with stable angina pectoris, especially if there is a low ischaemic burden7. The second Medical, Angioplasty, or Surgery Study (MASS-II), although underpowered (n=611) for clinical outcomes, showed no significant difference in survival between OMT and revascularisation (OMT 69%, CABG 75%, PCI 75%, p=0.09) at 10-year follow-up, despite an increase in the rates of MI and repeat revascularisation in the PCI and OMT groups8. A patient-level meta-analysis of the seven RCTs compared a strategy of initial CABG surgery (n=1,325) vs. initial medical therapy (n=1,325) to assess survival in patients with stable CAD between 1972 and 1984. The CABG group had significantly lower mortality than the medical treatment group at five years (10.2 vs. 15.8%, p=0.0001) and 10 years (26.4 vs. 30.5%; p=0.03). The benefits of CABG surgery were most pronounced for patients in the highest risk categories. CABG conferred a survival benefit in patients with unprotected left main stem or three-vessel CAD, particularly in those with severe symptoms, early positive exercise tests, and/or impaired left ventricular function9. These earlier trials, however, predated what would be described as OMT in contemporary practice. The use of different OMT components in some landmark clinical studies is shown in Table 2.
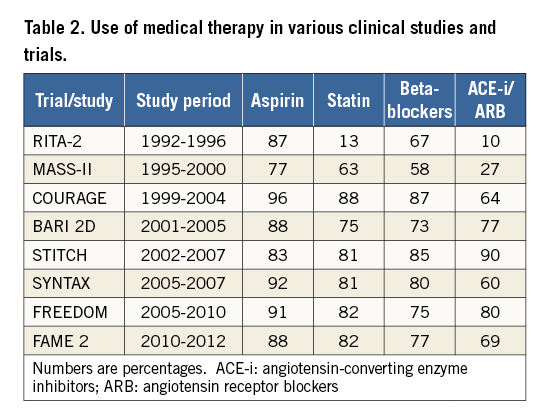
The landmark COURAGE (Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation) trial randomised 2,287 patients with significant 1-, 2- and 3-vessel CAD without left main stem involvement to OMT alone or OMT plus PCI. In this trial, at baseline 96% of patients received aspirin, 88% a statin, 87% a beta-blocker and 64% an ACE inhibitor or ARB. At five years, 95% were taking aspirin, 93% statins, 85% a beta-blocker and 78% an ACE inhibitor or ARB. This trial found no significant difference in the composite endpoint of death or non-fatal MI at 4.6 years of follow-up10. Both groups were also equal in terms of freedom from angina10. However, it should be noted that in a nuclear substudy of the COURAGE trial the reduction in ischaemic myocardium was greater in the PCI group (2.7% vs. 1.6%, p<0.0001)11. However, there was no correlation between the extent of ischaemia and future events12. The primary endpoint, death or MI, was similar in the OMT vs. PCI+OMT groups for no to mild (18% and 19%, p=0.92) and moderate to severe ischaemia (19% and 22%, p=0.53, interaction p=0.65)12.
The Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI 2D) trial enrolled 2,368 type 2 diabetic patients with CAD and randomised them to receive either prompt revascularisation (PCI or CABG) along with intensive medical therapy or intensive medical therapy alone. The primary endpoints were the rate of death and major adverse cardiac and cerebrovascular events (MACCE), a composite of death, MI, or stroke. At five-year follow-up, there was no significant difference in MACCE between the PCI and the medical therapy group. However, the MACCE rate was significantly lower in the CABG group compared with the medical therapy group (22.4% versus 30.5%, p=0.01). Nevertheless, there was no significant survival difference between the medical therapy group and the revascularisation group in either the CABG or the PCI stratum13.
The Fractional Flow Reserve (FFR) Versus Angiography for Multivessel Evaluation 2 (FAME 2) trial randomised 888 patients with stable CAD and at least one functionally significant stenosis (FFR ≤0.80) to OMT alone versus PCI plus OMT. This trial was prematurely terminated due to a highly significant difference in the incidence of the primary endpoint (a composite of death, MI, and urgent revascularisation) in favour of PCI. However, it must be noted that the difference in the primary endpoint was driven by urgent revascularisation and there was no difference in mortality or MI14. A meta-analysis of eight RCTs (n=7,229 patients) comparing initial coronary stent implantation versus OMT found no difference in mortality (OR 0.98, 95% CI: 0.84-1.16), non-fatal MI (OR 1.12, 95% CI: 0.93-1.34) and persistent angina (OR 0.80, 95% CI: 0.60-1.05) over a mean weighted follow-up of 4.3 years15. Other meta-analyses also yielded similar results16. Therefore, it remains appropriate to treat patients with stable CAD with OMT, and the indication for revascularisation with PCI or CABG would be persistence of symptoms despite OMT and/or improvement in prognosis7.
OMT for acute coronary syndromes
The majority of ACS patients rightly undergo coronary angiography and revascularisation with PCI or CABG in contemporary practice. However, OMT is also an indispensable and complementary component in the management of ACS patients. Aspirin administration in patients with a history of ACS is associated with substantial reduction in major vascular events17. DAPT comprising aspirin and a P2Y12 inhibitor improves outcomes in ACS patients compared with aspirin alone7. Newer P2Y12 inhibitors, prasugrel and ticagrelor, have improved outcomes compared with clopidogrel18. ACS patients undergoing PCI and treated with DAPT including prasugrel had lower rates of MI, urgent target vessel revascularisation, and stent thrombosis compared to DAPT with clopidogrel at 15-month follow-up of their index PCI in the TRITON TIMI-38 study19. There was an increased risk of bleeding and no effect on mortality19. However, among patients with NSTE-ACS, prasugrel did not significantly reduce the frequency of cardiac death, MI or stroke, as compared with clopidogrel, in the TRILOGY ACS trial20. In the PLATO trial, among patients with ACS treated with or without an invasive strategy, there was a reduction in the composite endpoint of death from vascular causes, MI or stroke when ticagrelor was included in the DAPT regimen as compared to clopidogrel (9.8% with ticagrelor group vs. 11.7% with clopidogrel; HR 0.84, 95% CI: 0.77-0.92; p<0.001)21. Ticagrelor also significantly reduced the rate of stent thrombosis. DAPT, if tolerated, should be continued for a minimum of 12 months; however, evidence for both shorter (for patients with high bleeding risk) and longer (for patients with high ischaemic/thrombotic risk) duration of DAPT is emerging. Further data and personalised application based on an individual’s bleeding vs. ischaemic/thrombotic risks are warranted. An ACE inhibitor and/or mineralocorticoid receptor antagonist are also indicated in post-ACS patients with diabetes, anterior MI, or evidence of left ventricular systolic dysfunction22. Similarly, β-blockers are recommended after ACS unless the patient has cardiogenic shock, decompensated heart failure or severe overt conduction disease7. Kurlansky et al have recently published data from the Coronary Artery Revascularization Evaluation (CARE) multicentre registry showing a significant improvement in MACE-free survival with the use of antiplatelet, lipid-lowering, and β-blocker therapy (p=0.001 for all three medications) in 3,228 patients with non-ST-elevation MI23.
OMT post revascularisation
OMT remains a cornerstone in the management of patients who have received coronary revascularisation therapy, whether PCI or CABG10,24. The progression of atherosclerosis continues after revascularisation and is associated with deterioration of left ventricular function and recurrent events. OMT may yield beneficial effects by reducing the progression of coronary disease and preventing new plaque rupture or thrombotic events25. Appropriate use of the secondary prevention therapy has been shown to reduce mortality and MI after revascularisation26. The use of OMT for secondary prevention, however, remains suboptimal, even in patients with established CAD who have undergone coronary revascularisation, particularly after CABG27-30. In the Euro Heart Survey, a sizeable proportion of patients with chronic stable angina, managed medically or invasively, were not on OMT and this was associated with poor outcomes31.
A post hoc analysis of the SYNergy between percutaneous coronary intervention with TAXus and cardiac surgery (SYNTAX) trial has shown that only 41% received OMT (defined as the combination of at least one antiplatelet drug, statin, β-blocker and ACE inhibitor) at the time of discharge after revascularisation (PCI or CABG); even fewer were taking OMT at five-year follow-up (PCI 40%; CABG 36%)5. OMT was associated with a significant reduction in five-year mortality (HR 0.64, 95% CI: 0.48-0.85, p=0.002) and the composite endpoint of death/MI/stroke (HR 0.73, 95% CI: 0.58-0.92, p=0.007)5 (Figure 2). This study suggested that all the components of OMT are important for reducing adverse outcomes. Furthermore, OMT improved outcomes in both the PCI and CABG arms without any significant interaction (p-value=0.44), confirming the importance of OMT for both PCI- and CABG-treated patients5.
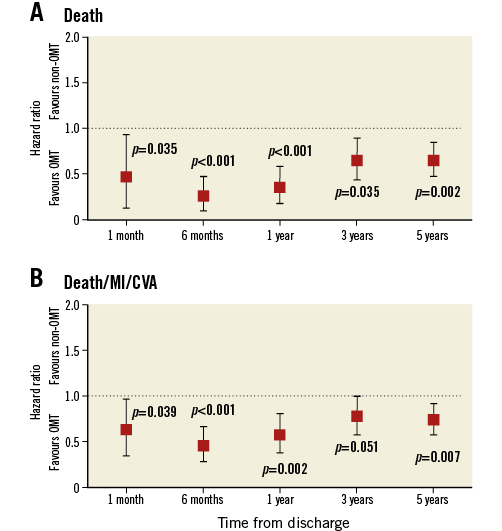
Figure 2. Effect of OMT on clinical outcomes in the SYNTAX patients. OMT significantly lowered the risk of death (A) or the composite endpoint of death/MI/CVA (B) throughout five-year follow-up. Hazard ratios (HR) with 95% confidence interval (CI) are shown (reproduced with permission from Iqbal et al, Circulation 20155). CVA: cerebrovascular accident; MI: myocardial infarction; OMT: optimal medical therapy
A post hoc analysis of the DAPT trial has shown that only 63% of the patients were on OMT (defined as a combination of aspirin, statin, β-blocker for all and ACE inhibitor/ARB where indicated by guidelines). Patients receiving OMT had lower rates of MI (2.7% versus 3.7%, p=0.003), MACCE (4.6% versus 5.7%, p=0.007), and bleeding (1.6% versus 2.5%, p<0.001) compared with patients not receiving OMT. However, death (1.6% versus 1.9%, p=0.155) did not differ32. In the CARE registry, 973 patients undergoing CABG and 2,251 patients undergoing PCI for non-ST-elevation MI derived significant benefits from OMT over a long-term (5+ years) follow-up, regardless of the revascularisation strategy23. The use of OMT was an independent predictor of MACE-free survival (HR for non-compliance 2.79, 95% CI: 2.19-3.54, p<0.001)23. Therefore, it is essential that, post revascularisation, patients should continue to use OMT on a long-term basis. Authors have also suggested that, for patients non-adherent to OMT, CABG outcomes are better than PCI, whereas for patients adherent to OMT both PCI and CABG offer similar outcomes23. Although this is based upon retrospective data derived from subgroup analysis of a modest number of patients, it is biologically plausible, as CABG outcomes may not be affected by disease progression in native vessels proximal to the graft, whereas PCI only addresses the treated segment33. It would therefore be reasonable to consider the likely adherence with OMT in decision making about the preferred method of revascularisation but more importantly to improve adherence in both PCI- and CABG-treated patients34.
Future directions
OMT AWARENESS
Further work is needed to raise awareness among physicians and patients about continuation of OMT, especially after revascularisation. OMT is complementary to and not competitive with PCI or CABG. Adherence to long-term medical therapy, especially in asymptomatic patients, remains low. The importance of OMT should be emphasised to patients at each clinical encounter to improve compliance. Combining the OMT agents in a single tablet (polypill) may also improve adherence35. It is essential to identify and address the barriers to OMT use including treatment costs, lack of awareness among physicians and patients, inadequate follow-up, side effect of tablets, etc.36,37. Further studies to understand the reason for OMT underutilisation and potential interventions to improve OMT utilisation and adherence are needed.
MONITORING COMPLIANCE AND THERAPEUTIC EFFECT
It may also be more appropriate to focus on achieving the desired therapeutic effect of the medication (lipid profile with statins, heart rate control with β-blockers and blood pressure control, etc.), rather than prescription of medication alone. However, it must be noted that statins have pleiotropic effects (on inflammation, endothelial function, etc.) beyond lipid lowering and therefore are beneficial for patients with established CAD or ACS, even if the lipid profile is normal.
Farkouh et al have shown that only 8% of patients in the Future Revascularization Evaluation in Patients with Diabetes Mellitus: Optimal Management of Multivessel Disease (FREEDOM) trial, 18% of patients in the COURAGE trial and 23% of patients in the BARI 2D trial achieved their target for controlling blood pressure, cholesterol, diabetes and smoking cessation38. In the ProspeCtive observational LongitudinAl RegIstry oF patients with stable coronary arterY disease (CLARIFY) registry (n=33,177), nearly 41% of patients on β-blockers had a heart rate above 70 bpm39. A post hoc study of the BARI 2D trial evaluated the relationship between survival/cardiovascular events and control of six risk factors (no smoking, non-high-density lipoprotein cholesterol <130 mg/dl, triglycerides <150 mg/dl, blood pressure [systolic <130 mmHg; diastolic <80 mmHg], glycosylated haemoglobin <7%) in 2,265 patients followed up for five years. The number of risk factors below predetermined target levels was strongly related to death and the composite of death, MI, and stroke. The authors concluded that simultaneous control of multiple risk factors through protocol-guided intensive medical therapy improves cardiovascular morbidity and mortality40. Therefore, it is important to monitor heart rate, blood pressure, lipid profile and HbAIc periodically in order to optimise the secondary prevention therapy.
LIFESTYLE MODIFICATIONS
Along with revascularisation and OMT, all cardiac patients should be encouraged to adopt a healthy lifestyle including healthy eating, regular physical activity and management of other cardiac risk factors. Patients who continue to smoke after revascularisation have poor long-term outcomes41,42. In the SYNTAX trial, smokers had worse clinical outcomes due to a higher incidence of recurrent MI. Smoking was an independent predictor of the composite endpoint of death/MI/stroke (HR 1.8, 95% CI: 1.3-2.5, p=0.001) and MACCE (HR 1.4, 95% CI: 1.1-1.7, p=0.02). Exercise-based cardiac rehabilitation has also been shown to improve outcomes and functional status but its uptake remains low43. A systematic review of prospective cohort studies and randomised controlled trials of patients with established CAD has shown mortality reduction with smoking cessation (relative risk [RR] 0.64, 95% CI: 0.58-0.71), increased physical activity (RR 0.76, 95% CI: 0.59-0.98) and dietary changes (RR 0.56, 95% CI: 0.42-0.74)44. Bittner et al have also shown that simultaneous control of multiple cardiovascular risk factors improves outcomes40. There is definite room for improvement in patient education about lifestyle modifications and it should be an integral part of medical management45.
NEED FOR NOVEL THERAPIES
There are data suggesting that, over the past two decades, fewer investigational cardiovascular drugs have entered clinical trials46. This may reflect more emphasis on developing interventional products (newer stents, etc.). However, there are many avenues where further developments are warranted including prevention of myocardial dysfunction and cardiac regeneration therapies. A notable achievement in recent years is the development of inhibitors of the PCSK9 (proprotein convertase subtilisin/kexin type 9) enzyme. Evolocumab is a monoclonal antibody that inhibits PCSK9 and lowers low-density lipoprotein (LDL) cholesterol levels by approximately 60%. The Further Cardiovascular Outcomes Research with PCSK9 Inhibition in Subjects with Elevated Risk (FOURIER) double-blind, placebo-controlled trial randomised 27,564 patients with atherosclerotic cardiovascular disease and LDL cholesterol levels of 70 mg per decilitre (1.8 mmol per litre) or higher whilst on statin therapy to receive evolocumab or matching placebo as subcutaneous injections. The primary efficacy endpoint was the composite of cardiovascular death, MI, stroke, hospitalisation for unstable angina, or coronary revascularisation. The key secondary efficacy endpoint was the composite of cardiovascular death, MI, or stroke. The median duration of follow-up was 2.2 years. At 48 weeks, evolocumab caused a 59% reduction in LDL, from a median baseline value of 92 mg per decilitre (2.4 mmol per litre) to 30 mg per decilitre (0.78 mmol per litre) (p<0.001). Relative to placebo, evolocumab treatment caused a 15% relative reduction in the risk of the primary endpoint (9.8% vs. 11.3%, p<0.001) and a 20% relative reduction in the key secondary endpoint (5.9% vs. 7.4%, p<0.001)47. There was no effect on cardiovascular mortality, but there was a statistically significant 27% reduction in MI and a 21% reduction in stroke. Multiple other PCSK9 inhibitors are under clinical development and evaluation.
NEED FOR FURTHER DATA
Whether a strategy of routine revascularisation (with PCI or CABG, as appropriate) plus OMT reduces rates of death or MI, or improves quality of life compared to an initial approach of OMT alone in patients with substantial ischaemia is uncertain. The ongoing International Study of Comparative Health Effectiveness With Medical and Invasive Approaches (ISCHEMIA) trial is being performed to determine the optimal approach to managing patients with stable CAD, moderate-to-severe ischaemia, and symptoms that can be controlled medically. Further data to define patient subgroups which may benefit from longer-term DAPT are also warranted.
Conclusion
All patients with stable coronary artery disease or acute coronary syndromes should receive OMT, unless contraindicated or not tolerated. OMT improves outcomes in cardiac patients and may have more impact than the choice of percutaneous versus surgical revascularisation. OMT should be the initial choice for stable CAD patients and complementary to revascularisation therapy for patients undergoing PCI or CABG for symptomatic or prognostic reasons.
Authors’ perspective
– Medical therapy for coronary artery disease has evolved in parallel to coronary revascularisation techniques.
– OMT is the initial therapy of choice for patients with stable coronary disease.
– Revascularisation is indicated for refractory symptoms or prognostically significant coronary disease.
– OMT improves outcomes in patients with stable coronary artery disease and acute coronary syndromes treated medically or invasively.
– OMT is complementary to PCI or CABG and should be continued after revascularisation.
Conflict of interest statement
The authors have no conflicts of interest to declare.