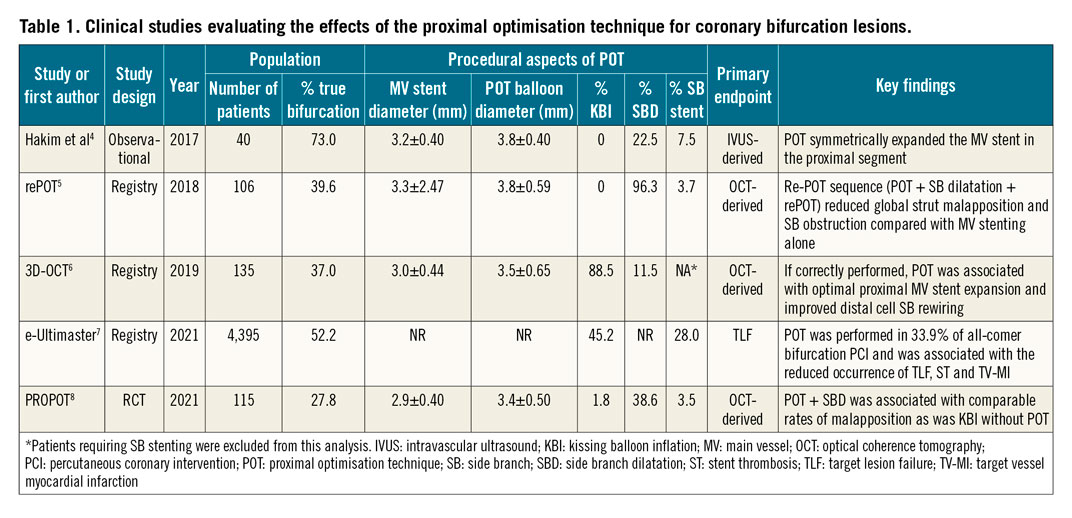
Initial recognition of the inherent risk of side branch (SB) loss when treating coronary bifurcations led the pioneers of percutaneous coronary intervention (PCI) to propose kissing balloon angioplasty as a potential remedy, aiming at simultaneous treatment of both bifurcation branches1. As the evolution of PCI progressed, an increased awareness of the fractal nature of coronary bifurcations gave rise to the concept of bifurcation stenting optimisation, adapting the fixed-diameter metallic scaffold to different diameters of bifurcating coronary arteries. In 2008, the proximal optimisation technique (POT) was introduced to practising clinicians at the annual European Bifurcation Club (EBC) consensus meeting to optimise the expansion and apposition of the main vessel (MV) stent proximal to the SB, where the vessel is larger compared to the distal segment, beyond the SB2. Apart from circular expansion of the proximal MV stent, the expected benefits of POT were improvement in SB rewiring by minimising the risk of inadvertent abluminal wire position and facilitation of the distal cell access. Following encouraging data from the bench3, observational and registry-based clinical studies were designed to prove the concept in vivo (Table 1). Symmetrical expansion in the proximal MV stent following POT was confirmed by intracoronary imaging4, as well as the need for repeat POT in case of SB dilatation (SBD)5. Furthermore, attention was drawn to the crucial role of procedural accuracy in terms of POT balloon size and positioning6. Finally, a large contemporary registry recently showed that, while routine application of POT in everyday practice was still lower than expected (33.9%), its use was associated with improved clinical outcomes7.
Similar to POT, kissing balloon inflation (KBI) can correct underexpansion and malapposition in the proximal MV, the added value being regaining the central position of the carina, albeit at the cost of potentially causing elliptical deformation of the proximal MV stent by the overlapping balloons.
Against this background, the Proximal Optimisation Technique Versus Final Kissing Balloon Inflation in Coronary Bifurcation Lesions trial (PROPOT)8 was the first randomised trial to compare POT+subsequent SBD versus KBI in 120 patients treated with provisional bifurcation PCI, in terms of OCT-assessed strut malapposition at the end of the procedure.
The overall results showed similar malapposition rates for both KBI and POT+SBD in the proximal MV stent segment (7.7% vs 10.4%, respectively, p=0.33), at the bifurcation core (1.1% vs 1.4%, p=0.67), and in the distal segment adjacent to the carina (5.3% vs 6.2%, p=0.59). The amount of SB obstruction, expressed by the rate of overhanging struts at the SB ostium, was also comparable (7.6% in the KBI group vs 9.9% in the POT+SBD group, p=0.16). Importantly, the rate of clinical adverse events was low and similar in both groups. Hence, the authors concluded that POT+SBD may offer no advantage over conventional KBI without POT in simple crossover stenting. While this conclusion does reflect the presented data, there are at least three important issues to be considered when interpreting the overall trial results.
First, the ability of POT alone to correct proximal malapposition and underexpansion after crossover stenting, which is its primary function, was not directly tested. Instead, the PROPOT trial evaluated the impact of SBD on MV stent geometry following angiography-guided POT. However, routine SBD is not recommended after crossover stenting, especially for the non-left main bifurcations. Hence, the general recommendation to perform POT after crossover stenting seems to remain unchallenged by the results of the PROPOT trial and is furthermore supported by the existing clinical evidence base (Table 1).
Second, only a quarter of patients completed the rePOT sequence (POT-SBD-POT), which has previously been shown to correct the potential distortion of the MV stent if SBD alone, without repeat POT, is performed5. Hence, the lack of repeat POT may explain the observed greater maximum malapposition distance at the bifurcation core’s distal edge in the POT+SBD group. Furthermore, if SBD after POT is needed, systematic use of a very short (4 mm) balloon, without repeat POT, was recently shown to reduce the risk of malapposition9, making it an attractive and simpler technique compared with either KBI or the rePOT sequence.
Third, clinical applicability of the PROPOT results may be limited by: a) the trial’s specific definition of malapposition (<100 mµ) that does not correspond to the current consensus (>400 mµ), and b) the risk of performance bias, since the wire position was checked at the middle optical coherence tomography (OCT) run, and any abluminal wiring in the absence of POT could be routinely corrected before proceeding with KBI, potentially resulting in a lower rate of malapposition compared with everyday clinical practice, still mainly relying on angiographic guidance.
In summary, despite heterogeneity in the study design, the clinical data accumulated so far (Table 1) show the efficacy of POT to correct proximal underexpansion after crossover stenting and the potential to improve patient outcomes. Taking it a step further, procedural standardisation, including POT balloon sizing and positioning, is needed to ensure that the expected benefits of optimisation techniques seen on the bench are translated into the clinical arena. What the PROPOT trial ultimately showed is that, if OCT is used as a standard to check the SB wire position following MV stenting and prior to any SBD, then KBI without POT appears to have similar effects on the MV stent geometry to POT+SBD.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.