We read with interest the paper by Watanabe et al investigating stent apposition in bifurcation lesions when the proximal optimisation technique (POT) was performed followed by side branch dilatation (SBD) versus the conventional kissing balloon inflation technique (KBT)1. We were pleased to read the paper and enjoyed the very well conducted quantitative optical coherence tomography (OCT) analysis. However, we have some concerns regarding the methodological approach and fear a false acceptance of the null hypothesis.
First, in the flow chart presented in Figure 1, we were pleased to see that OCT was performed immediately after initial treatment (POT+SBD or KBT). Analysis of this OCT pullback would clearly answer the research question whether POT+SBD would be superior in terms of stent apposition compared with KBT. Unfortunately, this analysis was not presented in the paper. Instead, all results presented were based on the final OCT pullback. In 40% (n=23) of cases in the POT+SBD group, additional stent optimisation was performed (either re-POT, SB dilatation or KBT) after the post-SBD OCT pullback (7% in the KBT group). Therefore, the study investigates another strategy than the one described in the aims and for which it was statistically powered. In its conclusion, the study accepted the null hypothesis, but this may be due to a type II error as elaborated below.
Second, we know from previous bench studies that stenting followed by SBD results in malapposition opposite the SB take-off (Figure 1A) and that this malapposition will be corrected by re-POT or KBT2,3. We speculate that the actual malapposition after initial treatment is higher and the study possesses a risk of underestimating the malapposition rate in the POT+SBD group, leading to a differential misclassification. Indeed, we agree that the operators needed to act on the OCT findings. We suggest that the authors perform a quantitative OCT analysis at the proposed step to investigate the risk of information bias.
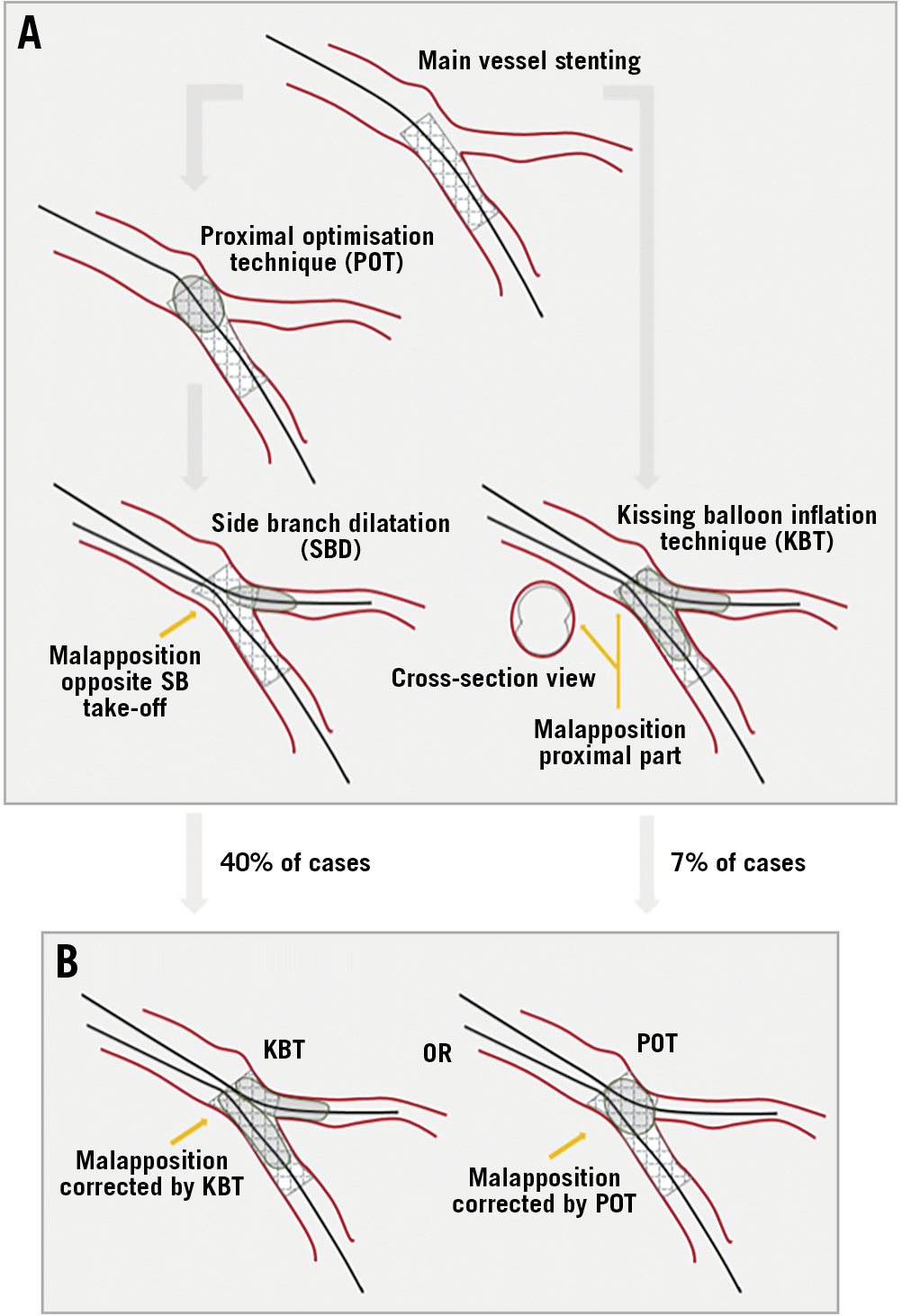
Figure 1. Theoretical procedure versus actual procedure. A) Sketch of the research question. Proximal optimisation technique (POT) followed by side branch dilatation results in malapposition opposite the side branch take-off (left). Kissing balloon inflation technique (KBT) results in malapposition of the proximal part. B) Actual study procedure (right). KBT corrects malapposition opposite the SB. POT corrects malapposition in the proximal part.
Third, the KBT group was treated without initial POT after MV stenting. This step is recommended by the European Bifurcation Club and is a mandatory step to facilitate SB rewiring, expand the proximal stent and avoid abluminal rewiring. Finet and colleagues found in a bench study that the percentage of malapposed stent struts was significantly lower when KBT was preceded by POT4. Therefore, the rate of malapposition might by overestimated in the KBT group with a risk of a differential misclassification (Figure 1A).
Finally, in our opinion the rationale for using KBT in primarily non-true bifurcation lesions is insufficiently explained. Only 28% of the enrolled lesions were true bifurcation lesions, which are the lesions that really benefit from either KBT or SB opening (COBIS II study5).
We suggest that the authors consider performing the as treated analysis needed to investigate if POT+SBD is superior to KBT in terms of malapposition for side branch opening after provisional stenting of coronary bifurcation lesions. It is an important research question raised by Watanabe and colleagues and we hope that the authors will consider our comments.
Conflict of interest statement
The authors have no conflicts of interest to declare in relation to this paper.
Supplementary data
To read the full content of this article, please download the PDF.