Abstract
Aims: We aimed to investigate the influence of the guidewire recrossing point on the incidence of incomplete stent apposition (ISA) after kissing balloon dilatation (KBD), and also clinical and angiographic outcome at nine months in a prospective multicentre registry.
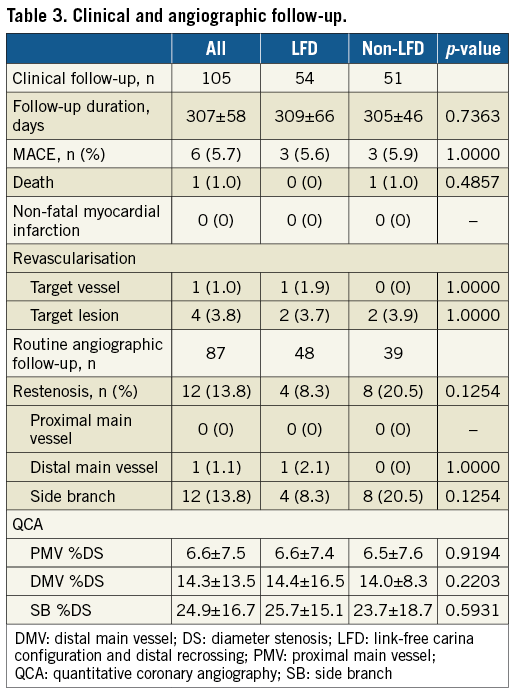
Methods and results: One hundred and five patients underwent single crossover stenting across the side branch (SB) and subsequent KBD. The jailing configuration of the SB orifice and the guidewire recrossing position were assessed by off-line 3D-OCT in the core lab. We defined the cases that achieved both link-free carina configuration and distal recrossing as the LFD group (54 cases), and the other cases as the non-LFD group (51 cases). ISA in the LFD group was significantly smaller than that in the non-LFD group (6.7±5.9% vs. 17.0±10.5%, p<0.0001). The distal recrossing rate was 83%. Proximal recrossing increased ISA compared with distal recrossing, particularly in parallel bifurcations (17.1±10.1% vs. 6.3±6.0%, p<0.0001). At follow-up, though event rates did not differ, SB restenosis in the non-LFD group tended to be higher than in the LFD group (20.5% vs. 8.3%, p=0.1254).
Conclusions: The guidewire recrossing point and the location of a stent link at the SB orifice had an influence on the ISA. KBD with optimal conditions under 3D-OCT guidance may reduce SB restenosis.
Abbreviations
ISA: incomplete stent apposition
KBD: kissing balloon dilatation
MV: main vessel
OCT: optical coherence tomography
SB: side branch
3D: three-dimensional
Introduction
Percutaneous coronary interventions (PCI) in coronary bifurcation lesions, which represent approximately 15-20% of all angioplasties1, result in more frequent acute closure due to stent thrombosis and restenosis compared to non-bifurcation lesions2-4. The variable morphology of coronary bifurcation lesions has inspired the development of many stent implantation techniques1. The currently recommended treatment is a simple single stent crossing over a side branch (SB) and provisional SB stenting1. In this technique, the advantages of final kissing balloon dilatation (KBD) are still debated5-8. Optical coherence tomography (OCT) is an imaging technique with approximately 10 times better resolution than intravascular ultrasound for evaluation of individual stent struts implanted in the coronary artery9. Three-dimensional (3D) reconstruction of OCT images can be used to clarify the configuration of an implanted stent, particularly at the coronary bifurcation10,11. A recent single-centre experience revealed that both the strut configuration and rewiring position before SB dilatation affect the incidence of non-apposed struts at the SB orifice after final KBD12. Stent malapposition and distortion could potentially be a cause of adverse events3,13,14. We investigated the influence of the guidewire recrossing point in the SB assessed by 3D-OCT or two-dimensional (2D)-OCT on the incidence of non-apposed struts at the SB orifice, and also clinical and angiographic outcome in the long term in a prospective multicentre registry.
Methods
STUDY DESIGN
The 3D-OCT Bifurcation Registry is a multicentre prospective registry that enrolled patients who underwent PCI for de novo bifurcation lesions with SBs having a diameter of at least 2 mm under OCT guidance in 10 participating centres from June 2014 to December 2015. The main exclusion criteria were in-stent restenosis, cardiogenic shock, chronic total occlusion, chronic kidney disease (creatinine ≥1.5 mg/dl), and emergency procedures. Single stent treatments with final KBD were extracted for the initial analysis.
PROCEDURE AND OCT ACQUISITION
The bifurcation treatment strategy and stent type were selected at the operator’s discretion. OCT images were obtained using the ILUMIEN™ FD-OCT Imaging System (St. Jude Medical, St. Paul, MN, USA) and the Dragonfly™ intravascular imaging catheter (also St. Jude Medical) after guidewire recrossing into the SB (every attempt), and after final KBD. OCT acquisition before the procedure was not mandatory. To assess the guidewire recrossing position, OCT pullback was performed from a main vessel (MV) at least 10 mm distal from the SB. A high-resolution mode pullback speed is recommended, using 100% contrast for blood clearance. Of the 10 participating centres, in three centres (Osaka Saiseikai Nakatsu Hospital, Yamaguchi University Hospital, and Yamaguchi Grand Medical Center) which had dedicated 3D reconstruction software, guidewire recrossing was performed under 3D-OCT guidance onsite. In the other centres, the guidewire recrossing was judged with 2D-OCT images. The guidewire recrossing point was confirmed at each attempt. It was recommended that the operator attempt to recross the distal cell until confirmation of distal rewiring by 2D- or 3D-OCT. The 3D-OCT images of all cases were reconstructed in the core laboratory later.
CLINICAL AND ANGIOGRAPHIC FOLLOW-UP
Patients underwent clinical and routine angiographic follow-up at nine months after the index procedure. Occurrence of death, myocardial infarction, and target vessel revascularisation was recorded, and incidences of angiographic restenosis at the bifurcation segment, defined as 50% diameter stenosis within the proximal MV or within 5 mm of the distal MV or SB ostia, were evaluated.
QUANTITATIVE CORONARY ANGIOGRAPHY
Quantitative coronary angiography (QCA) was performed using the QAngio® XA version 7.3 (Medis Specials, Leiden, the Netherlands) before and after the PCI procedure and follow-up. A bifurcation-dedicated tool was used for the analysis15. The reference vessel diameter, percent diameter stenosis, minimum lumen diameter of each branch, and bifurcation angle were measured.
THREE-DIMENSIONAL OCT IMAGE RECONSTRUCTION AT THE CORE LABORATORY
Three-dimensional reconstruction of the OCT images and assessment of the guidewire recrossing position were performed using the OCT data from all participating centres at the core laboratory. After importing the raw OCT data into an off-line workstation, automatic stent strut detection and enhancement were performed using dedicated software16. Images were exported as bitmap sequence files and imported into volume-rendering software called INTAGE Realia (CYBERNET, Tokyo, Japan). Two independent analysts assessed the configuration of the overhanging struts on the SB ostium and the recrossing position on a “cut-away” view and a “fly-through” view, respectively, of the 3D-OCT. The jailing configurations at the SB orifice and the rewiring position were classified according to a previous report12. Briefly, in the link-connecting type, there was a link connecting to the carina and, in the link-free type, there was no link at the carina. The larger area enclosed by both the carina and the stent strut, with at least one distal top of the stent hoop located on the SB ostium, was defined as the distal cell. The small triangular cells enclosed by the most distal hoop and the carina were defined as the far distal cells, which were included into the distal rewiring in this study. In the present study, the cases were divided into two groups according to the jailing configuration and rewiring position as follows: LFD group, cases with both the link-free (LF) type and distal (D) rewiring, and the non-LFD group, which included all other cases (Figure 1). Furthermore, bifurcation types (parallel or perpendicular) were assessed by 3D-OCT as per the previous report10. Briefly, the perpendicular type was defined as the bifurcation in which the SB opening is visible as an elliptical shape and not concealed by the carina when viewed perpendicular to the vessel wall. In contrast, the parallel type was defined as the bifurcation in which the proximal course of the SB is concealed behind the carina.
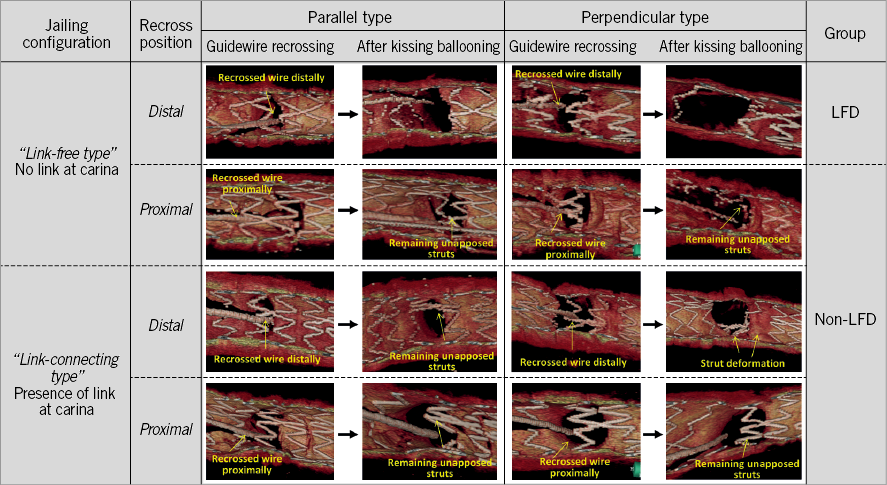
Figure 1. Representative pictures according to the jailing configuration, recrossing position and 3D bifurcation type. In the link-free type, if the guidewire was recrossed distally, jailed struts were removed optimally (LFD group). In other cases, unapposed struts at the SB ostium and strut deformation were observed (non-LFD group).
QUANTITATIVE OCT ANALYSIS
Quantitative off-line analysis of the OCT images was performed using proprietary computer software (St. Jude Medical). Frame-by-frame cross-sectional images were analysed by an experienced analyst, who counted every single strut on each frame at the bifurcation segment and at 1 mm intervals 5 mm proximal and distal to the bifurcation. The lumen area and stent area, as well as strut incomplete apposition, were measured.
Incomplete stent apposition (ISA) was defined as a distance between the strut marker and the lumen contour greater than the specific strut thickness plus the axial resolution of the OCT (14 µm)17. In this study, all non-apposed SB struts were considered ISA. Strut apposition was assessed at four segments: the proximal MV segment (extending 5 mm proximal to the first cross-section where the SB was visible); two sides of the bifurcation (divided into two 180° halves towards or opposite the origin of the SB); and the distal MV segment (extending 5 mm from the last cross-section in which the SB was visible)18. All distances were measured in perpendicular cross-sections from OCT pullback in the MV. The number of ISA struts was counted (Figure 2).
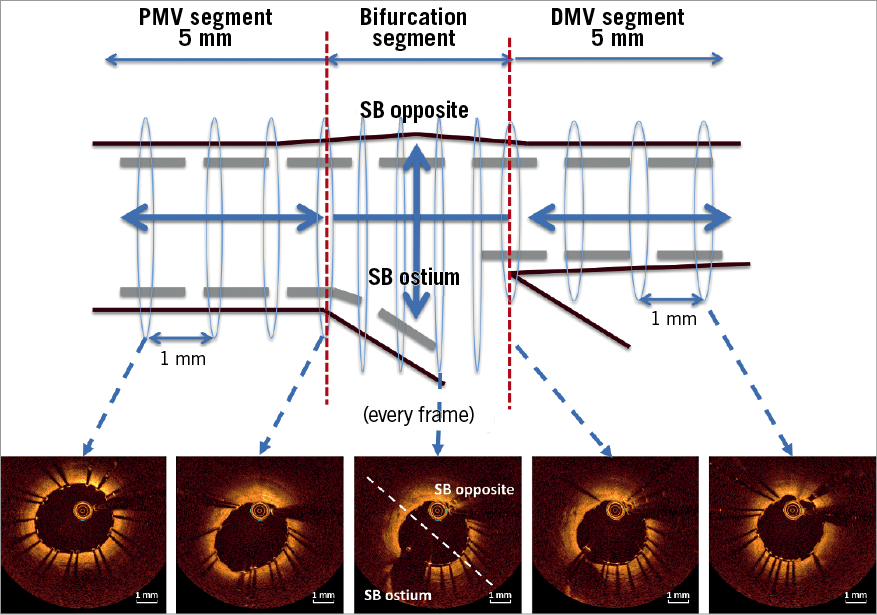
Figure 2. Segment location in bifurcation segment. The bifurcation segment was analysed for every cross-section and proximal main vessel (PMV) and distal main vessel (DMV) were analysed every 1 mm.
STATISTICAL ANALYSIS
Discrete variables are represented as counts and percentages. Continuous variables are represented as means±SD or median and interquartile range. Continuous variables were compared using either the Student’s t-test for normally distributed variables or the non-parametric Wilcoxon rank-sum test for non-normally distributed variables. Categorical variables were compared using the χ2 test or Fisher’s exact test. Inter- and intra-observer agreement for assessment of jailing configuration was assessed by the kappa statistic. A p-value of 0.05 was considered significant. Statistical analysis was performed using JMP, version 12 for Windows (SAS Institute, Cary, NC, USA).
Results
A total of 168 bifurcation lesions of 168 patients were included. Of these, 155 lesions were treated with the single-stent procedure. Final KBD was performed in 118 lesions. The guidewire recrossing position was assessed by OCT in 118 lesions, but clear 3D-OCT images were obtained for only 106 lesions (89.8%). A guidewire shadow prevented assessment in nine lesions (75.0%) and a non-uniform rotational distortion prevented assessment in three lesions (25.0%). No final MV pullback was obtained in one case. A total of 105 lesions were analysed with regard to both the guidewire recrossing position before SB dilatation and ISA at the bifurcation segment after KBD.
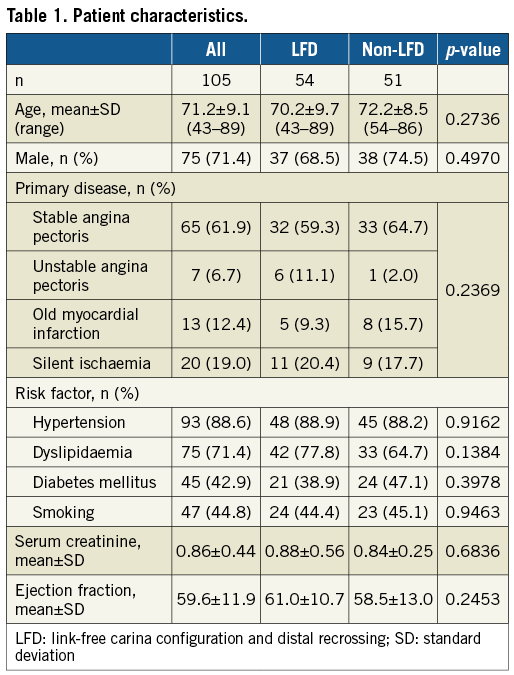
Patient and lesion characteristics are shown in Table 1 and Table 2. The frequency of distal rewiring was 65.9% (69/105) at the first attempt, eventually increasing to 82.8% (87/105). According to the jailing configuration, it was 70% (33/47) in the link-connecting type whereas 93% (54/58) of the link-free type successfully passed through the distal cell (p=0.002). Thus, 54 cases were classified as the LFD group (link-free configuration and distal rewiring) and the others (51 cases) were the non-LFD group. Regarding OCT guidance (3D: n=55, 2D: n=50), achievement of distal recrossing under 3D guidance was more frequent compared to that under 2D guidance (90.9% [50/55] vs. 74.0% [37/50], p=0.035). The number of attempts at distal recrossing was greater under 3D-OCT guidance (1.6±0.7 in 3D vs. 1.1±0.3 in 2D, p<0.001), while the radiation time and contrast volume under 3D guidance were not increased compared to those under 2D guidance (37.3±17.1 min in 3D vs. 31.7±15.7 min in 2D, p=0.059, 146±45 ml in 3D vs. 171±55 ml in 2D, p=0.013). Inter- and intra-observer agreement regarding the rewiring position was 0.9093 and 0.8638, respectively.
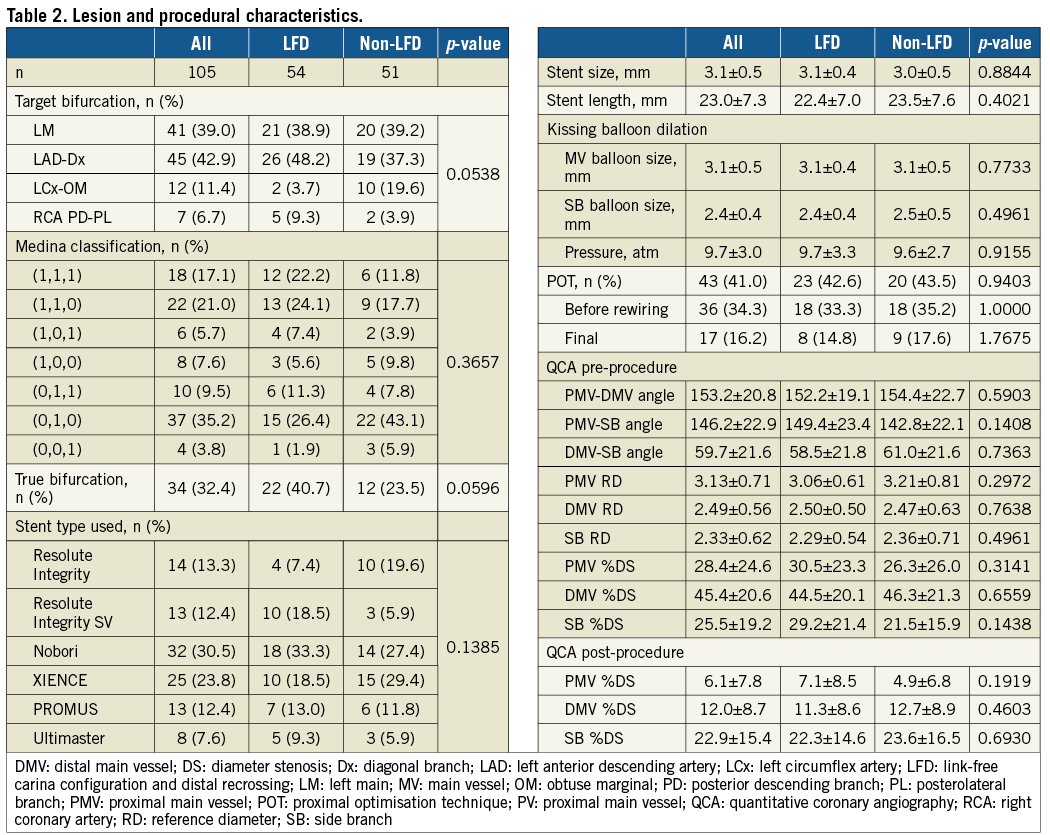
The incidence of ISA in the LFD group was consistently smaller than that in the non-LFD group, especially at the SB ostium (Figure 3). In more detail, the LFD group was significantly smaller than the other subtypes of non-LFD group in terms of the incidence of ISA at the SB ostium (Figure 4). There were 80 cases of the parallel bifurcation type and 25 cases of the perpendicular type. Mean angle between distal MV and SB measured by QCA was 54±18° in the parallel type and 77±23° in the perpendicular type (p<0.001). In the LFD group, the parallel type differed significantly from the perpendicular type in the frequency of ISA, while in the non-LFD group there was no significant difference between the two types (Figure 5A). In addition, particularly in the parallel type, proximal rewiring significantly increased the frequency of ISA compared to distal rewiring (Figure 5B).
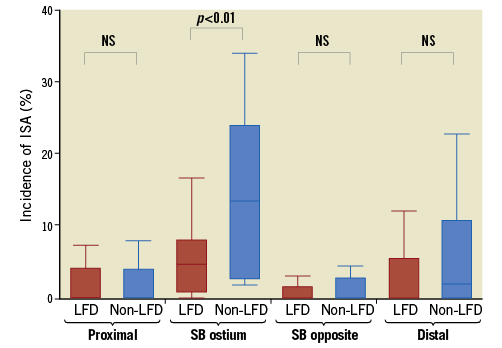
Figure 3. Incidence of incomplete stent apposition at each segment.
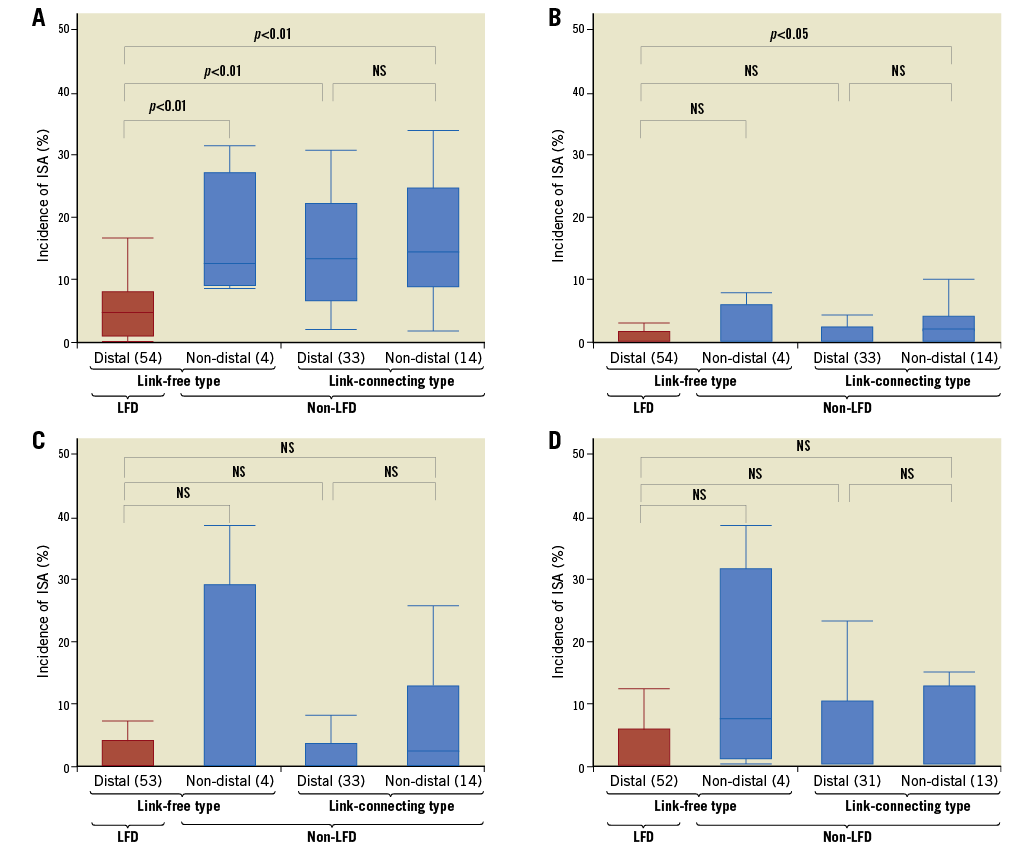
Figure 4. Incidence of incomplete stent apposition at each segment according to the jailing configuration and rewiring position. A) Side branch ostium, B) side branch opposite, C) proximal main vessel and D) distal main vessel.
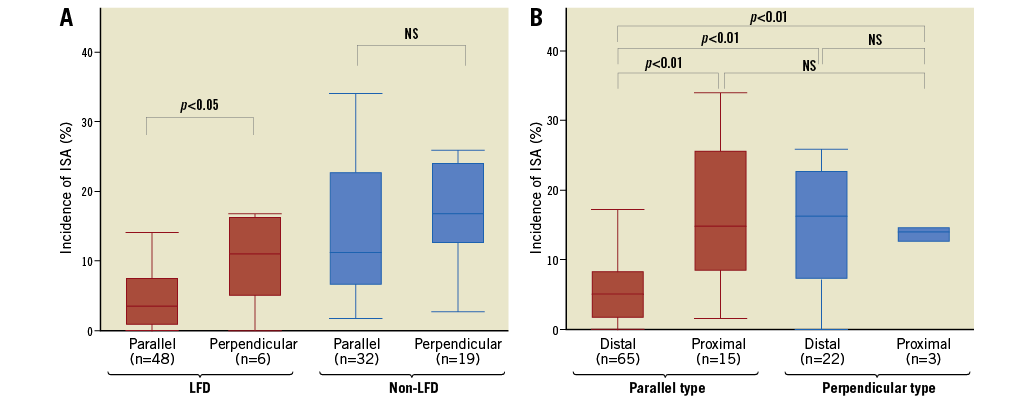
Figure 5. Incidence of incomplete stent apposition according to the 3D bifurcation type. A) The impact of bifurcation angle is more obvious in the LFD group than in the non-LFD group. B) Distal rewiring is important in the parallel type bifurcation.
For the follow-up, although the prevalence of cardiac events did not differ between the two groups, one patient in the non-LFD group died suddenly one month after the procedure (Supplementary Figure 1). Eighteen patients refused the routine angiographic follow-up, thus 87 (82.9%) patients underwent angiography. The incidence of restenosis at the bifurcation segment, particularly at the SB ostium, in the non-LFD group was more than twice as much as in the LFD group, without statistical significance (20.5% vs. 8.3%, p=0.1254) (Table 3).
Discussion
The main findings in this multicentre prospective registry were as follows. 1) The feasibility of off-line 3D-OCT for assessing the guidewire recrossing position was approximately 90%. 2) Achievement of distal recrossing under 3D guidance was more frequent than under 2D guidance (90.9% vs 74.0%, p=0.035). 3) The jailing configuration and the guidewire recrossing position before KBD were associated with the incidence of final ISA at the bifurcation segment. 4) When using the link-free type with distal recrossing, the bifurcation type (parallel or perpendicular) was related to the incidence of ISA after final KBD. Particularly in the parallel type, proximal rewiring significantly increased ISA compared to distal rewiring. 5) The incidence of SB restenosis in the non-LFD group tended to be higher than that in the LFD group.
A previous single-centre experience demonstrated that both distal rewiring and a link-free configuration were important factors for reducing ISA at the bifurcation12. However, several limitations might have affected the results such as the retrospective design of the study, the small number of cases (13), the biased selection of the drug-eluting stent (DES) type used (59% Nobori® [Terumo Corp., Tokyo, Japan] BES, 30% XIENCE® [Abbott Vascular, Santa Clara, CA, USA] EES), and procedural factors due to the limited number of operators in the single centre. Therefore, we conducted a multicentre prospective registry. This is the first original study with a relatively large number of cases by 3D-OCT.
Distal rewiring is generally recommended when dilating the SB orifice. The present study demonstrated that both the jailing configuration and rewiring position are important for optimal SB dilatation. In the link-free type, distal rewiring decreased the incidence of ISA compared with proximal rewiring, whereas there was no statistical advantage of distal rewiring in the link-connecting type. Therefore, a link-free configuration is favourable for SB dilatation. The link location at the bifurcation, however, is not controllable and the operator cannot intentionally implant a stent in a favourable configuration. Fewer longitudinal links per crown might reduce the incidence of the link-connecting configuration (Supplementary Table 1). The present study demonstrated that 3D bifurcation type (perpendicular or parallel) was also associated with the incidence of ISA after KBD. In the parallel bifurcation, distal rewiring could reduce the ISA at the bifurcation segment after final KBD, while in the perpendicular bifurcation ISA was not always reduced by distal rewiring. Although the optimal rewiring position might differ according to the jailing configuration and the bifurcation angle, it is highly likely that a proximal rewiring in parallel bifurcations will lead to far more severe malapposition.
Regarding the rewiring position, there has been no technique to grasp the appropriate cell robustly. The operator manipulates the guidewire under fluoroscopic guidance. Alegría-Barrero et al reported that successful distal recrossing on the first try occurs only 66.7% of the time when the rewiring position is checked by 2D-OCT19. The ISA at the bifurcation segment after final KBD under 2D-OCT guidance was significantly reduced compared with that under fluoroscopic guidance. In our study, the prevalence of distal rewiring at the first attempt was 65.9%, finally increasing to 83%. Notably, 100% distal rewiring was observed with the link-free type under 3D guidance, whereas 84.5% was observed under 2D guidance. The definition of distal rewiring between previous 2D- and our 3D-based assessment might be different because it is difficult to distinguish the smaller or larger distal cell only by 2D-OCT. Despite this, 2D- or 3D-OCT may help to avoid a proximal rewiring.
A clinical advantage of KBD after crossover stenting is not yet established1. The purpose of KBD is to avoid jailing struts and to keep the SB orifice area large5, but SB dissection, stent distortion, and subsequent metal carina are potential consequences of KBD1. In previous studies investigating the CYPHER® SES (Cordis [now Cardinal Health], Milpitas, CA, USA) or the XIENCE EES20, a favourable configuration might be less than recent two-link stents, because these stents had more links (six and three). Moreover, distal rewiring was achieved in approximately 70% to 80% of cases under fluoroscopic guidance. Those factors might interfere with the beneficial effects of KBD. 3D-OCT potentially obviates KBD in a parallel bifurcation where a proximal recrossing may lead to the risk of stent struts floating in the MV. Residual struts and stent distortion generated by SB dilatation could cause clinical adverse events. There are no reports describing a cut-off value of residual struts or the degree of stent distortion for predicting adverse events. Further studies would be needed.
Limitations
3D-OCT was performed in the core lab and the actual 3D-OCT guidance was performed only in half of the cases (55/105). Core lab analysis was performed after the procedure, so that the study was rather observational and was not designed to address the benefit of “3D-OCT guidance”. Furthermore, the present study was not performed in a randomised manner. These were the major limitations of the present study. Thus, the advantage of 3D-OCT guidance could not be fully evaluated in comparison with 2D-OCT guidance. The results according to comparison between 3D- and 2D-OCT guidance may be partially due to the difference in procedure/strategy between the 3D- and 2D-OCT guided centres. Our findings from the registry, however, indicated that 3D-OCT could be useful for guiding the insertion of the guidewire into the appropriate cell. Current OCT/OFDI consoles are equipped with online 3D reconstruction packages. The operator can assess the jailing configuration and rewiring position during the procedure. Based on the jailing configuration, the operator can select the optimal recrossing position, thereby potentially performing optimal KBD. A novel technique by which the stent can be adjusted under 3D guidance has been reported21. POT may facilitate distal recrossing and improve proximal apposition. Thus, relatively less usage of POT before KBD might affect the rate of distal recrossing. The various types of DES included were one of the major limitations. In addition, physiological assessment of the SB after KBD or at follow-up was not performed routinely. The number of cases remains small, and thus more detailed analysis is needed. The lack of statistical power regarding the clinical outcome is also a limitation. To investigate the clinical impact of 3D-OCT guidance for bifurcation stenting, a large number of randomised trials is necessary.
Conclusions
According to 3D assessment, ISA, including non-apposed SB struts in bifurcation lesions, is influenced not only by the recrossing position of the guidewire, but also by the presence of a stent link at the SB ostium and by the angle between the distal MV and SB. Furthermore, KBD with optimal conditions under 3D-OCT guidance might reduce SB restenosis.
| Impact on daily practice In bifurcation stenting, confirmation of both the guidewire recrossing point and the jailing configuration with 3D-OCT is important to lead optimal side branch dilatation after kissing ballooning. In the link-free type, distal recrossing reduced non-apposed jailed struts at the side branch orifice, while in the link-connecting type a case-by-case selection of the recrossing point under 3D-OCT guidance may be needed to achieve better side branch opening. |
Funding
This study was supported by an unrestricted research grant from the 3D-OCT Bifurcation Registry.
Conflict of interest statement
T. Okamura and J. Shite have received honoraria for technical consulting from St. Jude Medical. The other authors have no conflicts of interest to declare.
Supplementary data
Supplementary Table 1. Incidence of link-free type configuration and incomplete stent apposition according to the stent type used.
Supplementary Figure 1. A case involving the sudden death of a patient one month after bifurcation stenting.
To read the full content of this article, please download the PDF.