Abstract
Aims: The substudy was performed to evaluate the acute and eight-month follow-up effect of final kissing balloon dilatation (FKBD) on fractional flow reserve (FFR) in the side branch (SB) after main vessel (MV) stenting.
Methods and results: We included 75 patients in the Nordic-Baltic Bifurcation Study III FFR substudy: 42 in the FKBD group and 33 in the no-FKBD group. Complete angiographic and FFR eight-month follow-up was obtained in 25 (60%) patients in the FKBD group and 21 (63%) patients in the no-FKBD group. In the FKBD group the post-PCI mean SB FFR was significantly higher compared to the no-FKBD group (0.92 vs. 0.85, respectively; p=0.011). No significant difference in FFR value between treatments was detected at eight-month follow–up (0.91 vs. 0.87; p=0.19). There were no significant changes in mean SB FFR during the follow-up period (0.92 vs. 0.91; p=0.80) in the FKBD group and (0.87 vs. 0.87; p=0.91) in the no-FKBD group.
Conclusions: FKBD in simple stenting of bifurcation lesions improved acute functional outcome in SB compared to leaving the SB jailed. No significant difference was detected at follow-up. In both groups there was no significant functional late loss during follow-up. Thus, both strategies were equally effective in ensuring that side branch jailing would not cause ischaemia in the long term.
Introduction
Coronary bifurcation lesions are one of the most challenging subsets in interventional cardiology. Treatment of these lesions is associated with increased procedural costs, higher complication rates, and worse outcomes compared with percutaneous coronary interventions (PCI) of simple coronary lesions1,2. The provisional side branch (SB) intervention strategy is preferred for most bifurcation lesions because no previous study has shown the benefit of systematic stenting with two stents over this strategy3-7.
During a provisional strategy procedure, the operator has to decide whether the SB needs further treatment. The significance of an ostial side branch stenosis can be evaluated by visual estimation of angiographic stenosis severity, quantitative coronary analysis (QCA), Thrombolysis In Myocardial Infarction (TIMI) flow evaluation and fractional flow reserve (FFR). FFR is a stenosis-specific physiologic parameter reflecting both the degree of functional significance and the downstream myocardial territory11-13. Angiographic evaluation of stenosis severity has shown a weak correlation with the functional severity of ostial SB lesions8-10. Available jailed SB FFR data have provided us some reassurance that SB with moderate and severe ostial stenosis were often not functionally significant. Some discrepancies regarding the lower cut-off value for significance of angiographic diameter stenosis and limited data on FFR follow-up warrant additional data in this area.
The Nordic-Baltic Bifurcation Study III14 was a randomised clinical study comparing final kissing balloon dilatation (FKBD) vs. no-FKBD in simple stenting of coronary bifurcation lesions.
In this substudy we compared: 1) the influence of final kissing balloon dilatation (FKBD) technique on FFR in the SB; 2) the durability of FFR in the SB at eight-month follow-up; and 3) FFR and quantitative coronary angiography (QCA) of the SB ostium after PCI and at eight-month follow-up.
Methods
Patients and study design
The present study was a pre-planned substudy within the Nordic-Baltic Bifurcation Study III (NCT0091419914). The Nordic-Baltic Bifurcation Study III included 477 patients and assessed whether routine FKBD after successful stenting of the main vessel (MV) would improve outcomes in patients with coronary bifurcation lesions14. The FFR substudy was conducted in four centres and included 75 patients of which 33 and 42 patients were randomised to the no-FKBD group and the FKBD group, respectively. Decision to offer a patient inclusion in the FFR substudy was made at the operator’s discretion. A flow diagram of the study is shown in Figure 1.
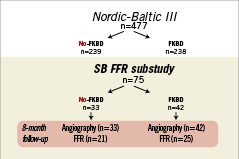
Figure 1. Flow diagram of the study.
Patients who were treated with a SB stent or had significant dissection after SB dilatation were not included in the FFR substudy.
Study procedure
Coronary stenting of the MV was performed with standard interventional techniques; if there was TIMI-3 flow in the SB after MV stenting, the patient was randomised to ±FKBD. Pressure measurements were performed before final angiograms using a 0.014 inch pressure guidewire (PrimeWire™; Volcano, San Diego, CA, USA; or Pressure Wire®; Radi Medical Systems, Uppsala, Sweden). The pressure wire was passed through the struts of the MV stent, and FFR was measured at least 5 mm distal to the jailed SB stenosis. Nitroglycerine was administrated before FFR measurements. Adenosine was infused through the femoral vein at at least 140 µg/kg per minute to induce maximal coronary blood flow. FFR results did not influence treatment strategy, thus SB lesions with post-PCI FFR<0.75 were not treated.
The sirolimus-eluting CYPHER SELECT® Plus (Cordis/Johnson & Johnson, Miami Lakes, FL, USA) coronary stent was used in the study.
Follow-up
All patients in the FFR substudy had angiographic follow-up at eight months. SB FFR follow-up was completed in 25 (60%) patients in the FKBD group and in 21 (63%) patients in the no-FKBD group.
Coronary angiograms obtained at baseline, at completion of the stenting procedure, and at eight-month follow-up were submitted to the joint angiographic core laboratory (Aarhus University Hospital, Skejby, Aarhus, Denmark and Pauls Stradins Clinical University Hospital, Riga, Latvia).
QCA was performed with the use of a computer-based system dedicated to bifurcation analysis (Qangio XA version 7.2; Medis, Leiden, The Netherlands).
Statistical analysis
Differences in categorical variables between the two groups were analysed using the Chi-square test or Fisher´s exact test. Continuous variables were analysed using an independent sample t-test and the Mann-Whitney U test. Data are expressed as mean (SD) or frequencies. Two continuous variables were analysed using the Pearson correlation test. Categorical versus continuous variables were analysed using the ANOVA test. P-values less than 0.05 were considered statistically significant.
Results
From March 2007 to September 2008, 83 patients were enrolled in the FFR substudy. The FFR measurements could not be obtained in eight (10%) lesions, due to SB dissection by the pressure wire in three cases and wiring failure in five cases. Those patients were excluded from further analysis. Baseline clinical characteristics are listed in Table 1 and showed no significant differences between the two treatment groups. Nineteen percent of patients had diabetes and most patients had stable angina (95%).
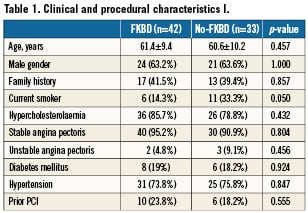
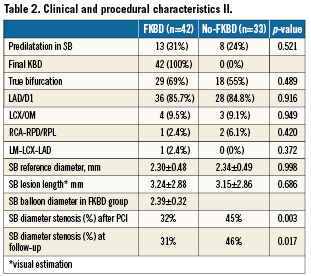
Details on procedure and lesion characteristics for the two groups are reported in Table 2. Most lesions were located in the left anterior descending artery (85%). Lesions were classified as “true bifurcation lesions” in 69% in the FKBD group vs. 55% in the no-FKBD group (p=0.49). The SB was predilated in 31% and 24% of cases (p=0.52) in the FKBD and no-FKBD groups, respectively.
After PCI and at follow-up there was a negative correlation between QCA percent diameter stenosis and FFR (Figures 2 and 3). After MV stenting, SB ostial diameter stenosis >50% was found in 24 (32%) cases according to QCA, while FFR <0.75 was found in only six (8% of total population) cases. All six (19%) of lesions with FFR <0.75 after PCI were in the no-FKBD group . The absence of FKBD was a strong predictor of FFR<0.75 (p=0.006) post PCI. At eight month follow-up, SB ostial stenosis was >50% in 18 (39%) cases according to QCA, while FFR was <0.75 in only four (9%) cases. Of these, one (4%) case was in the FKBD group and three (14%) cases were in the no-FKBD group (p=0.31).
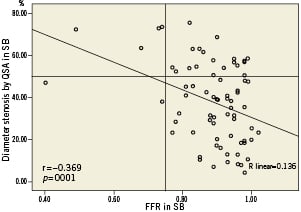
Figure 2. SB QCA vs. FFR after PCI. All cases with FFR <0,75 were in the no-FKBD group.
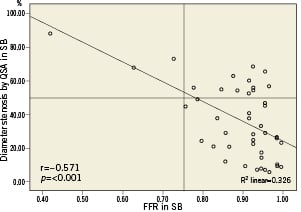
Figure 3. SB QCA vs. FFR at follow-up.
In the FKBD group the mean SB FFR value post PCI was significantly higher compared to the no-FKBD group (0.92 vs. 0.85, respectively; p=0.011). No significant difference was detectable at eight-month follow-up (0.91 vs. 0.87; p=0.19) (Figure 4). Mean SB stenosis by QCA post PCI and at follow-up was significantly higher in the no-FKBD group (Figure 5). Figure 6 shows the changes in FFR from post PCI to follow-up for patients with complete FFR evaluation. No patients in the FKBD group vs. three in the no-FKBD group had FFR <0.75 immediately after the index procedure. At follow-up one patient in the FKBD and two patients in the no-FKBD changed from non-significant FFR values to FFR <0.75. However, only one of the SB lesions that remained significant were still significant at follow-up. There were no significant changes in mean SB FFR and stenosis by QCA during follow-up in both treatment groups (Figures 6 and 7).
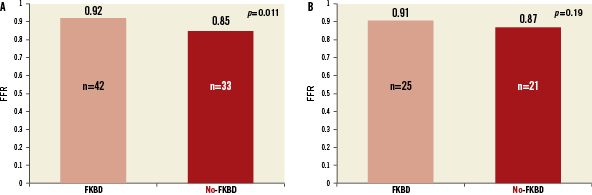
Figure 4. A) Mean FFR in SB after PCI. B) Mean FFR in SB at 8-month follow-up.
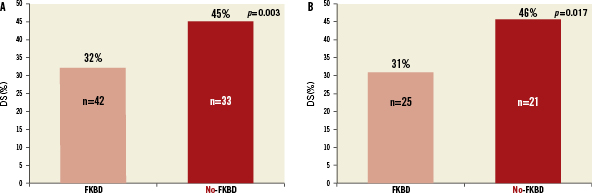
Figure 5. A) Mean SB stenosis by QCA after PCI. B) Mean SB stenosis by QCA at 8-month follow-up.
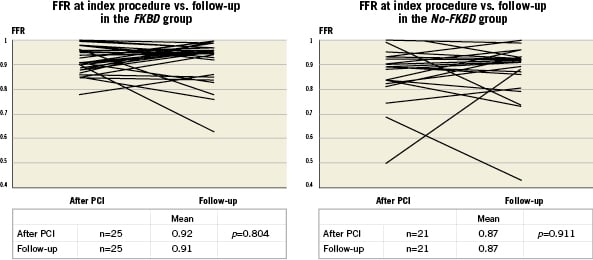
Figure 6. A) FFR at index procedure vs. follow-up in the FKBD group; B) FFR at index procedure vs. follow-up in the No-FKBD group.
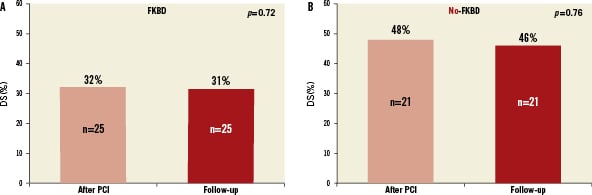
Figure 7. QCA at index procedures vs. follow-up in both groups.
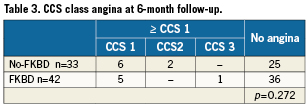
There were only two TLR cases: one in the FKBD group and one in the no-FKBD group. At six-month clinical follow-up there were no cardiac deaths, myocardial infarctions or stent thrombosis. The symptom relief was similar in the two groups (Table 3).
Discussion
The important findings of our study are as follows: 1) in the FKBD group, the mean SB FFR post PCI was improved significantly compared to the no-FKBD group but no functional difference was detectable at follow-up; 2) functional severity of jailed SB lesions after drug-eluting stent (DES) implantation in MV did not change significantly during eight-months follow-up; and 3) in three-fourths of cases angiography overestimated the functional severity of SB lesions after MV stenting when applying the >50% stenosis limit.
Angiographic stenosis severity of jailed SB after MV stenting has shown a weak correlation with functional severity assessed by FFR8-10. Our data supports the notion that angiography often overestimates severity compared to the functional significance of an ostial stenosis in a jailed SB. This is in part due to difficulties in visualising ostial lesions in multiple orthogonal views, and in part due to the fact that such lesions are often very short, reducing the likelihood that they limit blood flow significantly.
The >50% threshold for angiographic significance of ostial SB stenosis was challenged by Koo et al10 and a >75% limit was proposed. Later, the same authors failed to reproduce these findings16 and a >50% threshold again seemed appropriate to avoid false negative assessments. This is also supported by our data. Still, the majority of lesions defined by the 50% limit are false positives when compared to FFR measurements. Therefore, angiographically-assessed diameter stenosis is an inappropriate measure of SB lesion severity.
In both groups there was no significant functional late loss during follow-up. The durability of results as evidenced by FFR data supports the strategy of “just keep the SB open with TIMI-3 flow”.
The cutoff value for functional significance by FFR is debatable. We have adopted the 0.75 limit proposed and investigated by Dr. Koo in his landmark papers on functional side branch evaluation10,16. We find that side branches are often of little prognostic significance and treatment could be difficult. Therefore we find the 0.75 limit appropriate for SB intervention to ensure true functional significance.
The role of FKBD is still a matter of debate. The Nordic-Baltic Bifurcation Study III showed no clinical benefit of this technique at six-month follow-up. These results were limited by only 50% true bifurcation lesions in the study population and the short six-month follow-up period to the primary combined major adverse cardiac event (MACE) endpoint. Subgroup analysis of patients with true bifurcation stenoses showed that FKBD at follow-up significantly improved SB minimal lumen diameter, SB diameter stenosis and binary (re)stenosis14. We found that FKBD improved the functional and angiographic status of a jailed SB, but it did not translate into improved clinical results since six-month MACE rate and symptom relief were similar in both groups. In the context of the COURAGE study, one may anticipate that optimal medical therapy might be equal to PCI treatment of vessels supplying minor myocardial territories15. Furthermore, treatment of a SB (re)stenosis may be challenging, require additional stent or drug-eluting balloon treatment, and may negatively influence the MV result.
Recognising the theoretical advantages of FFR guidance, we would like to point out that the use of the pressure wire may be difficult in a jailed SB. Usually, the SB FFR evaluation will prolong the procedure, a microcatheter may be needed to interchange the regular guidewire for the pressure wire, and the procedure may lead to complications such as dissections and need of additional stenting. Angiographic evaluation is not limited by the need for intravascular assessment and the administration of adenosine. Moreover, two out of three SB with FFR<0.75 after the index procedure had a FFR >0.80 at follow-up, indicating that this may reflect a temporary rather than persistent problem in some cases. In case of TIMI-3 flow, a “wait-and see” strategy thus seems acceptable at the index procedure. Therefore, we do not recommend a mandatory FFR–guided treatment strategy in all bifurcation lesions. However, albeit not risk-free, FFR interrogation of side branches might be considered in cases where it is important to reach a decision on the grounds of vessel relevance. Our preferred strategy for treatment of bifurcation lesions is still the provisional strategy of stenting the main vessel with optional FKBD performed in cases with severe ostial pinching of the SB and/or SB TIMI flow <33,14.
Our FFR SB experience has furthermore given us confidence in accepting less than perfect angiographic SB ostium results in selected patients.
Conclusion
In this FFR substudy of the Nordic Bifurcation Study III on FKBD vs. no-FKBD, acute functional results were improved by FKBD and functional SB results were stable throughout eight-month follow-up in both groups. Insignificantly more patients in the no-FKBD group had functionally significant SB stenosis at follow-up, which might favour FKBD after MV stenting.
Limitations
There are several limitations of our study. The sample size is relatively small, patients were included at the operator´s discretion and follow-up FFR evaluations were not available in all patients. The SB lesion length by visual estimation was rather short at 3.2 mm and our results cannot be extrapolated to long SB lesions. We used QCA software dedicated to bifurcation analysis. The inherent limitation of QCA regarding optimal projection angles, frame selection and manual corrections applies to this study as well. All analyses were made by experienced observers using an elaborate customised standard operating procedure17. Differences between current QCA systems might limit the comparison to other studies16.
Funding source
All the participating centres received an unrestricted research grant from the Cordis/Johnson&Johnson company. The sponsor had no access to the study data and had no role in the design, conduct or reporting of the study.
Conflict of interest statement
The authors have no conflict of interest to declare.