Abstract
Aims: The EchoNavigator (EN) software (Philips Healthcare, Best, The Netherlands) enables real-time fusion of echocardiography and fluoroscopy by co-registration of the echocardiography probe on the x-ray image. We aimed to evaluate the feasibility and safety of this novel software during MitraClip procedures.
Methods and results: Twenty-one patients were treated with the support of EchoNavigator software (EN+ patients). The primary (safety) endpoint was the total radiation dose. Secondary endpoints were fluoroscopy and total procedure time. The measurements were compared to those of 21 patients treated immediately before the installation of EchoNavigator (EN- patients). More MitraClips (45 vs. 36) were implanted in the EN+ group, mirroring more complex interventions in this group. In EN+ patients, radiation dose (Gy/cm2) was similar compared to EN- patients (146.5±123.6 vs.146.8±134.1, p=0.9). Total procedure time (minutes) was similar in the EN+ group compared to EN- patients (136.2±50.2 vs. 125.7±51.2, p=0.5). The main benefit of the EchoNavigator is the automated real-time fusion of echocardiography and fluoroscopy, leading to easier catheter manipulation.
Conclusions: The use of EchoNavigator software was feasible and safe in all study patients. Further studies are necessary to confirm the benefits of using this software.
Abbreviations
2-D: two-dimensional
3-D: three-dimensional
A2: middle part of the anterior mitral valve leaflet
DRR: digitally reconstructed radiograph
EN: EchoNavigator
EN–: group in whom EchoNavigator software was not used
EN+: group in whom EchoNavigator software was used
Gy: gray
MC: MitraClip
MR: mitral regurgitation
OR: operating theatre
P2: middle part of the posterior mitral valve leaflet
TEE: transoesophageal echocardiography
Introduction
MitraClip® (Abbott Vascular, Abbott Park, IL, USA) implantation is currently the only accepted alternative interventional treatment option for patients with mitral valve regurgitation (MR) who are at high risk for surgery1. The procedure is an adaptation of the Alfieri stitch, but is performed with a catheter technique via femoral vein access and is a beating heart procedure. Alfieri and colleagues described a significant reduction of MR by producing a “double orifice” mitral valve with a stitch adapting the margins of A2 and P2 in severe degenerative disease2. The MitraClip (MC) procedure was initially introduced for the treatment of degenerative mitral valve disease but was also rapidly adopted in functional disease. The procedure significantly reduces MR, immediately improves haemodynamic function3 and has demonstrated good short and midterm clinical results4-6. The crucial steps for a successful procedure are a precise transseptal puncture7 and the placement of the MitraClip at the aimed lesion site. Fluoroscopy and real-time 2-D and 3-D transoesophageal echocardiography (TEE) are the imaging modalities of choice during the procedure8. The images of both techniques are presented to the operator in parallel, and the operator needs to fuse the displayed pictures mentally in order to succeed with the procedure. To support the operator with this demanding task and potentially to reduce the procedure length and the radiation dose necessary during such procedures, Philips Healthcare (Best, The Netherlands) introduced EchoNavigator, a software tool that provides real-time image co-registration and fusion of the TEE and fluoroscopy images during the procedure.
The goal of this study was to evaluate the feasibility and safety of the software during MitraClip interventions.
Methods
We compared the procedural characteristics of the first 21 patients who underwent a MitraClip procedure assisted by the EchoNavigator software to the procedural data of the 21 patients treated immediately before the introduction of the software. The procedures in all 42 patients were performed in a standard way for MitraClip implantation in a hybrid operating theatre (hybrid OR) as described earlier3. The primary safety endpoint was the radiation dose during MitraClip intervention supported by EchoNavigator. Secondary endpoints were fluoroscopy time, length of the overall procedural time and duration of the different procedural steps. The procedural steps were quantified as the time from femoral puncture to placement of the first, second, third and fourth clip. All patients gave written informed consent to be included in this prospective, non-randomised arm of the trial, and the study protocol was approved by the local institutional review board.
ECHONAVIGATOR
For this study, a prototype of the software was used. The EchoNavigator system synchronises and co-registers the echocardiography and fluoroscopy images in real time in hybrid ORs equipped with Philips hardware. Changes in angulation, rotation or position of the TEE probe are immediately registered and updated on fluoroscopy images. In addition, the software provides concordant views of TEE and fluoroscopy by presenting echocardiography images in the same anatomic alignment as the C-arm. Furthermore, if the C-arm is moved, echocardiography image information is updated with the same orientation (Moving image 1).
The key feature of EchoNavigator is the automated localisation of the echo probe in the fluoroscopy, providing real-time co-registration of the two image modalities. This happens in two steps, a detection phase and a tracking phase. The goal of the detection phase is to localise the probe in an x-ray image without using the results from previous images. A detection algorithm scans the entire x-ray frame for the possible presence of a TEE probe. This detection is based upon a technique using the edge models of the object of interest. The edge model for the EchoNavigator is computed from the boundaries of the digitally reconstructed radiograph (DRR) from a tomographic probe model of a TEE probe at a defined position (Moving image 1). The second phase is the tracking phase. In this phase the position of the probe is continuously updated, during both resting and rotating C-arm. Tracking describes the process of taking an estimate of the TEE probe pose as an input and refining it on the current x-ray image to produce an estimate of the current pose of the TEE probe.
The use of the EchoNavigator during MitraClip interventions is of particular interest during two procedural steps: puncture of the interatrial septum, and catheter steering for optimal clip placement. The optimal puncture site is defined by echocardiography, using the X-plane feature allowing simultaneous demonstration of two orthogonally orientated image planes. In agreement with the echocardiographer, the interventionalist marks this optimal puncture site using a tableside control pad by introducing a marker in the echocardiography image (Figure 1A). The marker is automatically updated on the fluoroscopy image (Figure 1B, Figure 1C, Moving image 2). Additionally the interventionalist can rotate and zoom an echocardiography image from the tableside independently from the echocardiographer (Moving image 3). By this means, the navigation of the transseptal puncture needle through the right atrium towards the optimal puncture site is facilitated and a targeted puncture enabled (Figure 1C). After successful septal puncture, the optimal clipping site is defined by the interventionalist in a similar fashion by marking the lesion at the level of the mitral valve in the echocardiography images and using the fluoroscopy images to help catheter manipulation within the left atrium (Figure 2A and Figure 2C).
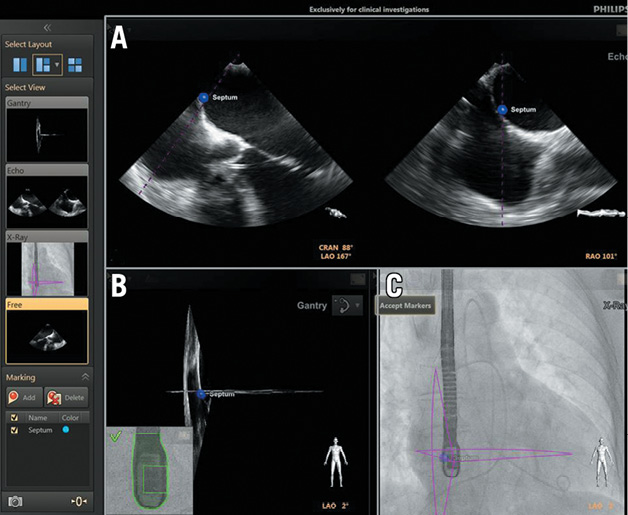
Figure 1. EchoNavigator view with: A) 2-D X-plane echocardiography image. The interatrial septum is marked with a blue dot. B) X-plane echo images with marker, oriented in the same way as the C-arm. The small inlay picture indicates that the TEE probe is registered correctly. C) Outlines of X-plane images together with the blue marker are fused with the fluoroscopy image.
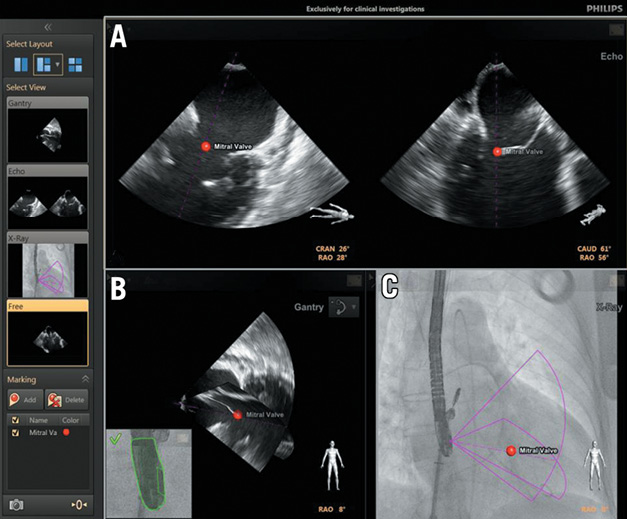
Figure 2. EchoNavigator view with: A) 2-D X-plane echocardiography image. The optimal mitral valve clipping site is highlighted with a red marker. B) X-plane echo images with marker, orientated in the same way as the C-arm. The small inlay picture indicates that the TEE probe is registered correctly. C) Outlines of X-plane images together with the red marker are fused with the fluoroscopy image.
STATISTICAL ANALYSES
Continuous variables are expressed as mean plus standard deviation. Categorical data are given in proportions. The unpaired t-test was used for comparison of the two groups for continuous variables, and Fisher’s exact test was used for binary variables. A p-value of less than 0.05 was considered statistically significant. Statistical analyses were performed using SPSS software (IBM SPSS Statistics version 20.0; SPSS Inc., Chicago, IL, USA).
Results
BASELINE CHARACTERISTICS
The baseline characteristics of the patient population are shown in Table 1. The mean age of the patients was 77±9 years, and 38% of patients were female. At the time of intervention, 95% of patients had severe MR. In 52% of the cases, degenerative MR was the reason for the intervention. Five patients in the EN+ and two patients in the EN- group needed more than two clips. Since the majority of patients treated in Europe received only one or two clips9, additional analyses are given for these patients.
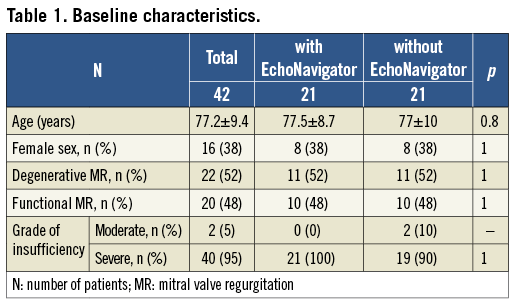
PRIMARY ENDPOINTS
The procedural data are shown in Table 2. Total radiation dose and fluoroscopy time did not differ significantly between the groups. In patients with one or two clips, a trend towards a reduction of radiation dose (–15%) and fluoroscopy time (–5%) was observed (Figure 3). Six out of the seven patients in whom more than two clips were implanted had advanced mitral valve prolapse, usually with multiple segments involved. This condition is therefore less suitable for MC treatment and thus these patients needed more complex procedures.
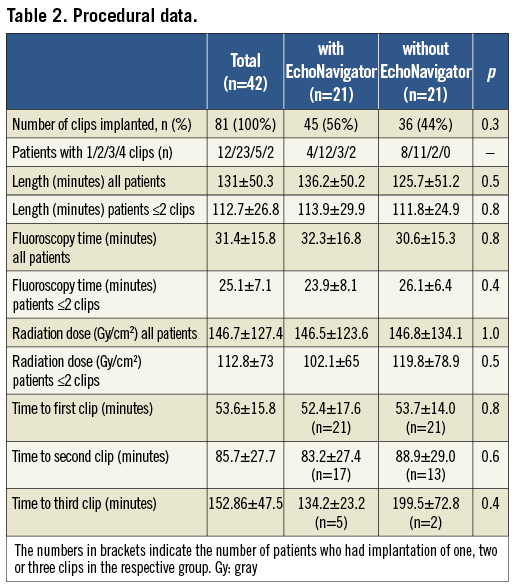
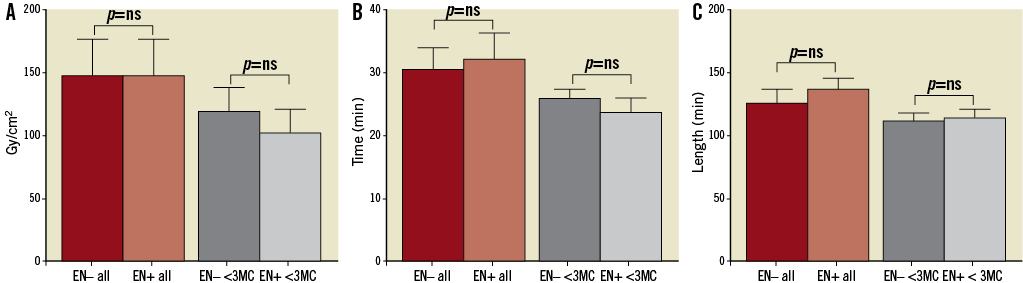
Figure 3. Primary endpoints. (A) Radiation dose in all patients (EN– all and EN+ all) and in those patients with one or two MCs (EN– ≤2 MCs and EN+ ≤2 MCs). (B) Fluoroscopy time in all patients (EN- all and EN+ all) and in those patients with one or two MCs (EN– ≤2 MCs and EN+ ≤2 MCs). (C) Procedure length in all patients (EN– all and EN+ all) and in those patients with one or two MCs (EN– ≤2 MCs and EN+ ≤2 MCs). EN–: control group before installation of EchoNavigator; EN+: with use of EchoNavigator; all: total patient population; ≤2 MC: group of patients with only one or two MCs implanted; Time: fluoroscopy time; Length: procedure length from puncture to closure
SECONDARY ENDPOINTS
While more clips were needed in the EchoNavigator group (45 vs. 36, p=0.3), the length of the interventions was similar for both groups. The higher the number of clips used, the shorter the time duration per clip when the EchoNavigator was used compared to the control group (Figure 4). When two clips were used the time until the placement of the second clip could be decreased by six minutes (7%) and, when three clips were used, a decrease in the length of the procedure of more than one hour (33%) was seen. A fourth clip was placed in only two patients with very advanced mitral valve prolapse in the EchoNavigator group, yet the time to placement of the fourth clip was shorter than the time for placement of three clips in the control group.
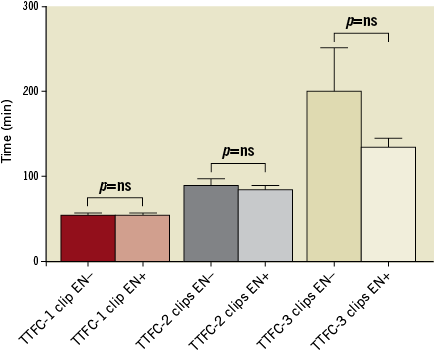
Figure 4. Milestones of the procedure. EN–: control group before installation of EchoNavigator; EN+: with use of EchoNavigator; TTFC: time needed until final clip was placed; 1 clip, 2 clips, 3 clips: number of clips used in the procedure; min: minutes
INFLUENCE OF LEARNING CURVE
A trend towards reduction of radiation dose, procedure length and fluoroscopy time was observed during the second half of patients in whom the EchoNavigator software was used, in those patients where one or two clips were used (Figure 5).
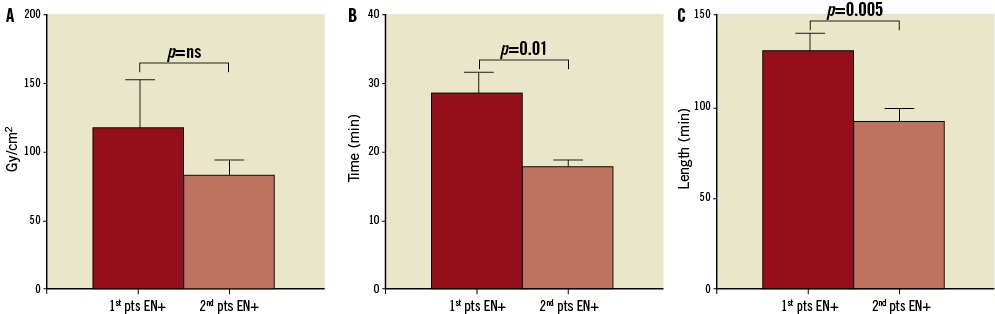
Figure 5. Results representing the learning curve in patients with one or two clips implanted. A) Radiation dose. B) Fluoroscopy time. C) Procedure length. EN+: with use of EchoNavigator; Time: fluoroscopy time; Length: procedure length from puncture to closure; 1st pts: first half of patients (n=10); 2nd pts: second half of patients (n=10).
Discussion
Fluoroscopy and echocardiography are the imaging modalities of choice during MitraClip implantation. Echocardiography provides excellent imaging of the anatomical structures of the mitral valve and especially three-dimensional echocardiography is crucial for the orientation and precise guide steering during the procedure. However, image quality can be suboptimal due to shadowing by catheter overlays, and guidewires may at times not even be detected by echocardiography9,10. Fluoroscopy on the other hand gives a two-dimensional view of the field of interest. In contrast to echocardiography it clearly visualises the catheter and its position and is therefore a necessary part of the procedure. Additionally, the clip itself is better visualised by fluoroscopy. The mental fusion of both image modalities is necessary but also challenging for the operator. Good communication between the operator and the echocardiographer is of great importance to facilitate this process. However, in a standard hybrid OR, the set-up can be unsupportive for easy and effective communication. The EchoNavigator software fuses echocardiography and fluoroscopy and holds the potential to facilitate this process.
This study aimed to evaluate the safety and feasibility of the EchoNavigator software by using a prototype of the programme during MitraClip implantation. As shown by our data, the software was successfully used in all of the first 21 cases planned and was supportive for the procedure. Despite the necessity of using fluoroscopy to co-register both image technologies, the primary safety endpoint (radiation dose), was similar in both groups. The differences in length of the procedure only showed a trend and did not reach statistical significance. The procedure time in the EN+ group was not remarkably higher compared to the EN- group, despite the fact that these data reflect our learning period using prototype software that was updated several times during the study until the currently used stable version was available. In addition, the patients in the EchoNavigator group needed more clips. Given these considerations, the trend to reduction of both radiation dose and intervention time is even more remarkable.
The mean length of the procedure was comparable in both groups, and the times are similar to other published series9,11. Interestingly, the time until a final clip was placed was inversely correlated to the number of clips used. Despite the fact that more clips needed to be implanted in the EchoNavigator group (signalling more complex interventions), the total time needed for the procedure was not relevantly higher compared to the control group. The duration until a third clip was placed was much shorter in the EchoNavigator group compared to the control group. Multiple clips are needed mostly in severe degenerative mitral valve disease, which represent very challenging interventions. This shows that in complex procedures where more clips are used the imaging modality becomes even more important and the use of supporting software is beneficial. With increasing experience the software will not only facilitate difficult interventions in structural heart disease by providing a variety of new image projections to the operator, but also has the potential to reduce procedural time and radiation exposure. The goals of the development of further versions of the software are the implementation of catheter visualisation and the overlay of echocardiographic images for tissue visualisation.
Limitations
This study contains the usual limitations of all non-randomised studies. Sheer luck led to very similar patient groups, and thus comparison appears meaningful despite the small number of patients in each group. Furthermore, this study was designed to test the feasibility and safety of this new software and not to compare head to head the superiority of the software.
Caution is necessary when interpreting our data. The challenge in evaluating medical software during cardiac interventions lies in the complexity of the interventions. We determined factors that are relatively stable in order to measure the performance of the software. However, a lot of variables such as the quality of echocardiography images or anatomical alterations influence the length of an intervention and the need for additional fluoroscopy time. Therefore, we cannot exclude that non-measured factors may have influenced the results.
The EchoNavigator software is only available in combination with specific Philips hardware. However, many interventionalists use competitor hardware and software. Thus, unfortunately, our results only address those colleagues who use such a set-up.
Conclusion
In this non-randomised study, the use of the EchoNavigator was feasible and safe during MitraClip interventions, and tended to reduce the radiation dose and procedure time. A prospective, randomised trial with a larger sample size is needed to demonstrate efficacy of the software.
Funding
The Division of Cardiovascular Surgery at the University Hospital Zurich holds a research grant from Philips Healthcare (Best, The Netherlands).
Conflict of interest statement
R. Corti and P. Biaggi have received speakers’ honoraria from Abbott Vascular, Brussels, Belgium, and Philips Healthcare, Best, The Netherlands. The other authors have no conflicts of interest to declare.
Online data supplement
Moving image 1. Registration of the TEE probe. The clip shows the EchoNavigator screen as seen in the OR. Upper screen shows a TEE view of the septum. Left lower screen shows the TEE screen of the EchoNavigator software. When the automated registration of the TEE probe is successful, the small inlay image of the TEE probe head turns from red to green. The right lower picture shows the angio-screen of the EchoNavigator software with the outline of the ultrasound window.
Moving image 2. Tableside placement of a marker at the atrial septal wall. The clip shows the EchoNavigator screen as seen in the OR. Upper screen shows the regular TEE view. Lower left screen shows the TEE screen of the EchoNavigator software with registered TEE probe. The right lower picture shows the angio-screen of the EchoNavigator software with the outline of the ultrasound window. Yellow markers are placed from the tableside by the interventionalist at the position of the septum in the TEE screen. The markers are automatically fused to the other screens. The marker is labelled afterwards by choosing a description from a list. At the end of the moving image, the X-plane view and the 3-D view of the software are demonstrated.
Moving image 3. Tableside control and rotation of 3-D TEE image. The clip shows the EchoNavigator screen as seen in the OR. Right upper screen shows a regular 3-D TEE. The left upper and lower screens show the 3-D TEE screen of the EchoNavigator software. The right lower screen shows the angio-screen of the EchoNavigator software with the outline of the 3-D ultrasound window. The interventionalist rotates, zooms in and out and places a marker from the tableside in the left lower view.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Registration of the TEE probe. The clip shows the EchoNavigator screen as seen in the OR. Upper screen shows a TEE view of the septum. Left lower screen shows the TEE screen of the EchoNavigator software. When the automated registration of the TEE probe is successful, the small inlay image of the TEE probe head turns from red to green. The right lower picture shows the angio-screen of the EchoNavigator software with the outline of the ultrasound window.
Moving image 2. Tableside placement of a marker at the atrial septal wall. The clip shows the EchoNavigator screen as seen in the OR. Upper screen shows the regular TEE view. Lower left screen shows the TEE screen of the EchoNavigator software with registered TEE probe. The right lower picture shows the angio-screen of the EchoNavigator software with the outline of the ultrasound window. Yellow markers are placed from the tableside by the interventionalist at the position of the septum in the TEE screen. The markers are automatically fused to the other screens. The marker is labelled afterwards by choosing a description from a list. At the end of the moving image, the X-plane view and the 3-D view of the software are demonstrated.
Moving image 3. Tableside control and rotation of 3-D TEE image. The clip shows the EchoNavigator screen as seen in the OR. Right upper screen shows a regular 3-D TEE. The left upper and lower screens show the 3-D TEE screen of the EchoNavigator software. The right lower screen shows the angio-screen of the EchoNavigator software with the outline of the 3-D ultrasound window. The interventionalist rotates, zooms in and out and places a marker from the tableside in the left lower view.

